- Submissions

Full Text
Developments in Anaesthetics & Pain Management
Therapeutic Effectiveness of Endoscopic Anterior Cervical Canal Decompression with Trans Vertebral Approach for Cervical Spondylotic Myelopathy Under Local Anesthesia: Endo-ACCD Surgery for Cervical Spondylosis Myelopathy
Jianfeng Zhang1*, Fei Gao2* and Yi Feng1,2
1Department of Anesthesiology, Peking University People’s Hospital, China
2Department of Pain Medicine, Peking University People’s Hospital, China
*Corresponding author:Jianfeng Zhang, Department of Anesthesiology, Peking University People’s Hospital, China Fei Gao, Department of Pain Medicine, Peking University People’s Hospital, China
Submission:July 01, 2025;Published: August 07, 2025

ISSN: 2640-9399 Volume3 Issue1
Abstract
Objective: Cervical Spondylitis Myelopathy (CSM) is a serious degenerative disease that significantly
affects the life quality of patients. Surgical treatment remains the preferred choice. However, traditional
open decompression and fusion surgery can cause considerable trauma to patients with CSM. In recent
years, some scholars have proposed full endoscopic surgery, which also has its drawbacks, especially in
anterior cervical approaches, as it relies on general anesthesia and lacks effective protective measures for
the trachea and esophagus.
Methods: In this study, we made a first attempt to perform Endoscopic Anterior Cervical Canal
Decompression (EACCD) with trans vertebral approach for CSM under Local Anesthesia. Its effectiveness
and safety were also observed. Eleven patients were included. The therapeutic efficacy was evaluated by
Visual Analog Scale (VAS), modified Japanese Orthopaedic Association (mJOA) score, and total efficacy
rate at pre-operation and post-operation 1, 3 and 6 months.
Result: All cases achieved good therapeutic effects. The VAS and mJOA were significantly improved at
different follow-up time points compared with the pre-surgery. The total efficacy rate at post-operation 1,
3 and 6 months was 0, 18.18% and 72.73% respectively. No severe complications were observed.
Conclusions: This research provides a new surgical option for better treating CSM. Compared to surgery
under general anesthesia with endotracheal intubation, EACCD under local anesthesia offers patients
a more comfortable experience and a safer medical model, further shortening the duration of surgical
trauma and hospital stay. Additionally, directly observing the esophagus under the endoscope avoids the
extra impacts of the gastric tube and contrast agent on the CSM patients.
Keywords:Endo-PCCD; Lateral decubitus position; Local anesthesia; VAS; NDI; mJOA
Abbreviations: CSM: Cervical Spondylotic Myelopathy; CT: Cervical Computed Tomography; EACCD: Endoscopic Anterior Cervical Canal Decompression; ECG: Electro Car Diogram; Endo-PCCD: Endoscopic Posterior Cervical Canal Decompression; mJOA: Modified Japanese Orthopaedic Association Scores; MRI: Magnetic Resonance Imaging; OPLL: Ossification of the Posterior Longitudinal Ligament; VAS: Visual Analog Scale.
Introduction
Cervical Spondylotic Myelopathy (CSM) is a type of spinal cord dysfunction caused by chronic compression of the cervical spinal cord [1]. Patients with CSM typically present with gait disturbance, pain and numbness in limbs and even dyschezia as well as dysuria in severe cases [2,3]. While in the initial phase of this disease, the symptoms are usually non-specific and unnoticeable to the patients, which may cause deterioration of the CSM patients’ condition. This is also the reason why CSM is easily overlooked, especially for patients who over 60 years of age. Available data have indicated that up to 25% of the general population experiences varying degrees of spinal cord compression [4]. Furthermore, elderly males are more susceptible to CSM [5]. Therefore, timely accurate diagnosis and effective therapy are critical to saving patients. To date, there are many theories related to the CSM development and some influential ones are described below. First, the hyperplastic surrounding tissues including ligamentum flavum, osteophytes or intervertebral disc led to direct mechanical compression of the spinal cord. Second, overlapping injuries induced by incorrect excessive flexion/ extension movements can result in different degrees of spinal cord compression and lastly, spinal cord blood supply disorder may be present when the surrounding tissues cause compression of vertebral artery or its branches [2,6,7].
Regardless of the cause of CSM, of cause, early surgery should always be most recommended [8], since there is evidence that the rates of disabilities in activities of daily living with non-operative treatment are 21%, 28%, 56% at 2, 3 and 10 years, respectively. Surgical approaches of CSM can be implemented using either anterior, posterior or combined procedures, depending on the specific situation. Generally, patients with ligament flava hypertrophy or hyperplasia of the facet joints are treated through posterior approach. While those with Ossification of the Posterior Longitudinal Ligament (OPLL) or significant kyphosis would benefit from an anterior approach [9,10]. However, the traditional open surgical approach has the drawbacks of great trauma, bleeding and multiple complications such as esophageal perforation, in turn, significantly prolong the length of the hospital stay and increase the financial burden of patients.
In recent years, endoscopic treatment of CSM has been widely used with the continuous advancement of endoscopy technology. Endoscopic therapeutic techniques for CSM offer several potential advantages over traditional open surgery, specifically reduced bleeding, minimal trauma, faster recovery and improved patient comfort. Nonetheless, cervical decompression under endoscopy currently still relies on general anesthesia, which poses numerous intraoperative management challenges for anesthesiologists, particularly in terms of airway management. The head and face of patients need to be draped in normal sterile fashion, even during endoscopic surgery, increasing the risk of tracheal tube dislodgment or kinking. Furthermore, general anesthesia with tracheal intubation inherently increases perioperative risks for patients such as difficult extubation, postoperative nausea and vomiting, especially for elderly patients. More importantly, frequent and vigorous cervical activity during surgery resulting in airway edema can also elevate the risk of post-extubation asphyxia. Therefore, it is imperative to explore a new operation mode that allows patients to complete the surgery under local anesthesia or mild sedation. After all, communication with patients during surgery is sometimes better than electrophysiological monitoring modalities.
Materials and Methods
Patient characteristics
We retrospectively analyzed the clinical data of 11CSM patients who have experienced Endoscopic Anterior Cervical Canal Decompression (EACCD) surgery, admitted to the Department of Pain Medicine, Peking University People’s Hospital from September 2021 to Mar 2024. This evaluation was approved by the Ethics Committee of Peking University People’s Hospital (approval No. 2023PHB). The informed consent in the current study was waived, due to there was no direct individuals contact. And all patients provided verbal consent for this case series to be published. Routine blood tests, coagulation tests, biochemical routine, imaging examinations including Cervical Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) and Electro Cardio Graphic (ECG) examination were performed on the day of hospital admission.
The inclusion criteria were:
a. The diagnosis of ventral cervical spinal cord compression
between two adjacent segments was confirmed with imaging
examination.
b. Participants who had the indications for EACCD surgery.
c. Visual Analog Scale (VAS) pain scores>3 points when patients
first sought medical advice.
d. Pre-operative modified Japanese Orthopedic Association
Scores (mJOA)≤14 points.
While the exclusion criteria were:
a. Patients with dorsal cervical spinal cord compression and
severe cervical segmental instability.
b. Patients are unwilling or unable to cooperate with the followup.
Endoscopic posterior cervical canal decompression
The patient was placed in the supine position with the head backwards. Then, the conventional intravenous access was established and the vital signs were monitored. Subsequently, routine disinfection was performed and a sterile drape was laid out after locating the narrow segment using C-arm fluoroscopy. The puncture point was determined at the intersection of the horizontal level of the narrow segment and the medial edge of the sternocleidomastoid muscle, followed by layer-by-layer infiltration anesthesia using 10~15mL of 0.5% lidocaine until the surface of the vertebral body was reached. It was important to note that before making the puncture channel, the “two-finger method” should be used to separate the external carotid artery from the internal esophagus and trachea to avoid additional tissue damage. An approximately 15mm transverse incision was then made at the puncture point. The skin, hypodermis and superficial layer of cervical fascia were sequentially incised and a blunt guide rod was placed. Next, the lateral carotid sheath and the medial visceral sheath were bluntly separated until the surface of the prevertebral fascia. The working cannula of the cervical endoscope was inserted along the guiding rod, after which the endoscope and trephine were placed. It is noted that the front-end of the working cannula was designed with a curved oblique opening. The bevel should be rotated outward to avoid damage to the medial esophagus and trachea when placing the working cannula. Once the endoscope observes the prevertebral fascia, the bevel should be rotated inward under direct endoscopic visualization, positioning the internal trachea and esophagus to the outer side of the working cannula, in order to avoid tissue damage. Moreover, the trachea and esophagus should be pushed by the bevel of working cannula to fully expose the vertebra.
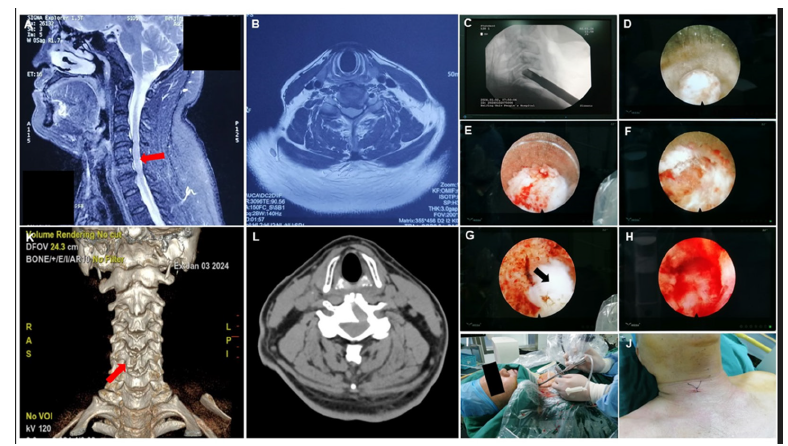
Then, the cryogenic plasma knife (DZX-G3040-A340, Shaanxi, China) was carried out to reveal the surface of vertebral body and disc by clearing surrounding tissue, especially the prevertebral fascia. Controlling bleeding promptly was needed to ensure a clear surgical field during the exposure of the vertebra. Moreover, the position of the trephine was observed and adjusted to bring it close to the center of the vertebral body and avoid pedicle damage, under C-arm lateral fluoroscopy. The selection of the endoscope and trephine was as follows: If the patient’s intervertebral disc width was greater than 18mm, a 6.9mm endoscope and an 8.0mm trephine were chosen; If the patient’s intervertebral disc width was less than 18mm, a 5.3mm endoscope and a 6.4mm trephine were selected. The trephine then rotated and cut from the anterior inferior of the inferior vertebra direction to the posterior superior direction along the vertebral body. For instance, if the compression site of CSM patient is between C5 and C6, the trephine is used to rotate from the anteroinferior aspect of the C6 vertebra in a posterior-superior direction until reaching the posterior longitudinal ligament. This was the so-called trans vertebral approach. The aforementioned rotated cutting process carries certain risks of internal fracture collapse; therefore, it is necessary to proceed under continuous guidance from the C-arm fluoroscopy. The herniated intervertebral disc material and the osteophytes were removed successfully to adequately decompress the spinal cord, allowing for good dural pulsation to be observed. During decompression, a continuous flow of saline with a degree of pressure should be maintained to ensure a relatively bloodless operative field. Finally, the instruments including the endoscope, trephine, and working cannula were removed and the incision was closed without drain (Figure 1).
Fgure 1:The surgical procedure. Note: A: The MRI of the patient before surgery. The compression site is marked with red arrow at the junction of the C5 and C6 spinal cord segments; B: patient pre-operative MRI cross-section; C: the front-end of trephine touched the anterior inferior of the vertebra under C-arm lateral fluoroscopy; D, the paravertebral fascia is exposed; E, the process of rotating and cutting using trephine; F, the process of rotating and cutting using trephine; G, the nucleus pulposus is exposed (black arrow); H, the dural sac is exposed, and the pulsation of dural sac can be observed under direct endoscopic visualization. I, surgery in progress; J, the skin was closed by surgical stitching; K, CT guidance and 3D reconstruction after surgery; L, patient post-operative CT cross-section.
Efficacy evaluation and follow-up observation
Baseline clinical characteristics were collected including age, sex, disease course, length of stay, surgical levels, operative time, VAS and mJOA upon admission. The therapeutic effects were assessed by evaluating the mJOA, VAS and total efficacy rate. The mJOA, a refinement of the original JOA score, is a clinical tool used to evaluate the severity of myelopathy, particularly in patients with CSM. And the VAS score is a commonly used self-assessment instrument for evaluating pain intensity. Additionally, to assess the overall effect of EACCD for treating CSM, we introduce the concept of total efficacy rate. In the current study, the standards of effective treatment were VAS<3 points and mJOA>14 points. The therapeutic efficiency rate (%) =effective/n×100. Follow-up examinations were conducted by an experienced medical assistant at 1 months, 3 months and 6 months.
Statistical analysis
Data handling and statistical tasks were performed by an independent researcher with the help of SPSS 25.0 software (IBM Corporation, Armonk, NY, USA). To check if the quantitative data adhered to normal (Gaussian) distributions, the Shapiro-Wilk test was conducted. In this study, aside from age, all numerical variables like disease course, length of stay, operative time, mJOA and VAS followed a non-normal distribution. Consequently, age is thus expressed as means and Standard Deviations (SD), whereas the other quantitative data are given as median and interquartile range. For comparing the mJOA and VAS at various follow-up times, the Friedman test is used, while the Mann-Whitney U test is applied for post hoc pairwise comparisons. P-values that were less than 0.05 were considered to show statistical significance.
Result
Participant demographic and clinical characteristics
The present study included a total of 11 patients, consisting of 6 males and 5 females, with an average age of 55 (±9.445). The average duration of the CSM and the average length of hospital stay were 14.82 months and 2.9 days, respectively (these two sets of measurements did not conform to a normal distribution) (Table 1).
Table 1:Participant demographic and clinical characteristics.
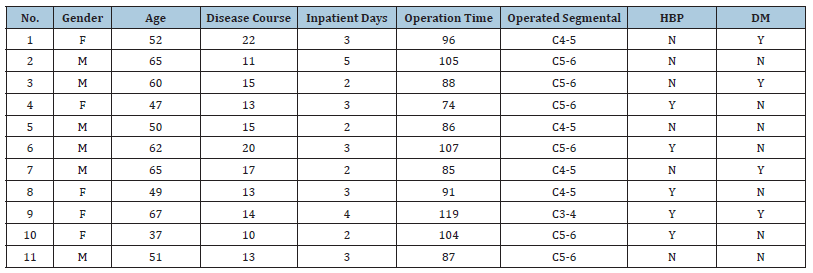
Abbreviations: HBP: High Blood Pressure; DM: Diabetes Mellitus.
The changes of VAS and mJOA for all time points
As shown in Figure 2A, there was a notable reduction in VAS after EACCD surgery at different follow-up intervals compared to pre-operation (#P1mon=0.04, Z=-2.842; #P3mon=0.08, Z=-2.673; #P6mon=0.05, Z=-2.810). Moreover, compared to 1-month postsurgery, the follow-up at six months post-surgery showed a significant decrease in VAS (*P=0.019, Z=-2.342). While no statistically different was observed between post-surgery 1 month and 3 months. The findings of functional assessments were like VAS (Figure 2B). The mJOA decreased significantly at different time point compared to baseline (#P1mon=0.01, Z=-2.588; #P3mon=0.005, Z=-2.807; #P6mon=0.003, Z=-2.943). Similarly, the mJOA significantly improved in post-EACCD 3 months and 6 months compared to 1 month (*P3mon =0.012, Z=-2.527; *P6mon=0.003, Z=-2.937).
Fgure 2:The alterations of VAS and mJOA at each time point. Note: The changes of VAS(A) and mJOA (B) for all time points. Results are presented as median with range.
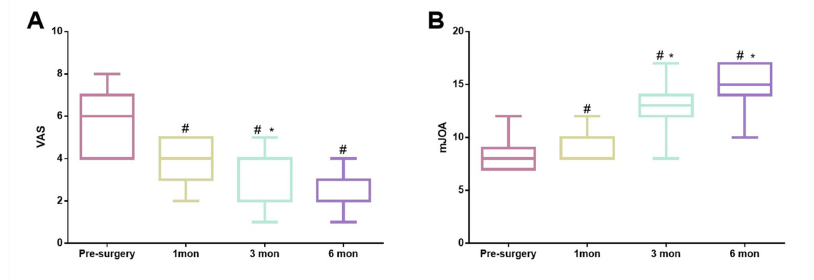
Total efficacy rate
To assess the overall effect of EACCD for treating CSM, we introduce the concept of total efficacy rate. We opted to use VAS <3 points and mJOA>14 points as the standard for an effective therapy. The total efficacy rate of the EACCD surgery were 0%, 18.18% and 72.73% at 1 month, 3 months and 6 months timepoints, respectively.
Discussion
Essentially, this is a report on a technical update. He et al. proposed an Anterior Percutaneous Full-Endoscopic Trans- Corporeal Decompression of the Spinal Cord (APFETDSC) technique that can provide more surgical options for patients with CSM, thereby avoiding open surgery. The incision for open surgery is relatively large. And when the surgical field is exposed, there is significant tension on the anterior soft tissues of the neck, increasing the risk of soft tissue damage. APFETDSC surgery greatly reduces the risks of trauma and bleeding and also benefits postoperative recovery for patients. However, it is undeniable that there are several areas for improvement in this endoscopic surgery. Firstly, it is crucial to protect the trachea and esophagus of the patients during anterior cervical spine surgery, especially the esophagus, as this directly relates to the occurrence of postoperative complications. Previous full-endoscopic anterior spinal surgery such as APFETDSC used the position of a gastric tube filled with contrast agent to determine the location of the esophagus. Then use the contralateral side, oriented toward the esophagus, as the surgical approach. However, this method has its own limitation. Since the gastric tube is narrower than the esophagus, relying solely on the contrast agent in the gastric tube may not accurately reflect the position of the esophagus. This still poses a risk of esophageal injury. The working cannula with curved oblique opening proposed in this study can, under direct endoscopic visualization, keep the esophagus outside the bevel, theoretically completely avoiding esophageal injury. In fact, we have not encountered any cases of esophageal or tracheal injury in our clinical practice.
Another unique feature of this study is that the entire EACCD surgical procedure is performed under local anesthesia. Although patients are in an unconscious state during surgery under general anesthesia, this can increase the risk of spinal cord injury, even with neurophysiological monitoring [11]. Patients can provide realtime feedback under local anesthesia on their subjective feelings during the surgery. For instance, the patient’s ability to perform swallowing movements during the procedure can indicate that the esophagus has not been damaged. Additionally, the head and face of patients are covered with sterile drapes during general anesthesia, which increase the difficulty of airway management for the anesthesiologist. There is also an increased risk of accidentally bumping into the endotracheal tube during the procedure, which can lead to kinks or dislodgement. Performing the surgery under local anesthesia not only ensures safety but also reduces the length of hospital stay, allowing patients to ambulation earlier, which is more beneficial for postoperative recovery. More importantly, patients experience minimal pain and fear during the EACCD procedure. However, this surgery also presents several technical challenges. Firstly, establishing a safe puncture zone for the anterior cervical approach is essential. During local anesthesia puncture and skin incision, the “two-finger method” must be used to separate the lateral artery from the esophagus and trachea to avoid damaging surrounding tissues. Secondly, the front-end of the working cannula must contact the bony structure at the time of initial insertion. Moreover, it is crucial to determine under C-arm guidance whether the working cannula and trephine are in contact with the vertebral body. This process requires caution to prevent structural damage during insertion. Thirdly, the bony channel opened by the trephine is from the anteroinferior direction towards the posterosuperior direction. This trans vertebral approach is less likely to compromise stability of internal fracture compared to the trans disc approach. There is no need to proceed with further cervical fusion surgery.
This study found that, both the AVS and mJOA scores of patients showed a sustained improvement from one month after surgery to six months postoperatively, indicating that the EACCD surgery has a therapeutic effect similar to that of open surgery for CSM. However, in this study, the total efficacy rate was relatively low in the first month post-surgery, possibly because our criteria were somewhat stringent, although other studies have not compared using this method. It is worth noting that some patients experienced reduced pain after one month but had not yet regained functional recovery, while others experienced the opposite. We attempted to identify the reasons for the differing treatment outcomes, but the small sample size limited our ability to conduct a statistical analysis. We speculate that patients with preoperative positive pathological signs and prolonged compression may have a poorer prognosis [12]. Additionally, patients with diabetes may require a longer recovery time after surgery [13]. However, this requires further large-sample case-control studies.
Undeniably, the current study has many shortcomings. Firstly, the small sample size is a significant limitation and future research could involve large-sample multicenter case-control studies to compare the therapeutic effects and prognostic factors of various anterior cervical spinal surgeries. Secondly, considering the prolonged time the patient lies flat and their feelings of fear, we can only perform a single-segment EACCD surgery. In further exploration, we attempted to conduct a single-incision, dualchannel, double-segment surgery under local anesthesia. Finally, the duration of follow-up is also a deficiency to our study. In conclusion, this research provides a new surgical option for better treating CSM. Compared to surgery under general anesthesia with endotracheal intubation, EACCD under local anesthesia offers patients a more comfortable experience and a safer medical model, further shortening the duration of surgical trauma and hospital stay. Additionally, directly observing the esophagus under the endoscope avoids the extra impacts of the gastric tube and contrast agent on the CSM patients.
References
- Eguchi Y, Suzuki M, Yamanaka H, Tamai H, Kobayashi T, et al. (2020) Myovascular preserving open-door laminoplasty for cervical spondylotic myelopathy with miniplate fixation. Int J Spine Surg 14(4): 476-482.
- Opara J, Odzimek M (2024) Cervical spondylotic myelopathy-diagnostics and clinimetrics. Diagnostics (Basel) 14(5): 556.
- Bram R, Fiore S, Labiak JJ, Davis RP (2017) Combined anterior-posterior decompression and fusion for cervical spondylotic myelopathy. Am J Orthop (Belle Mead NJ) 46(2): E97-E104.
- Nouri A, Tessitore E, Molliqaj G, Meling T, Schaller K, et al. (2022) Degenerative cervical myelopathy: Development and natural history [Ao spine recode-DCM research priority number 2]. Global Spine J 12(1_suppl): 39S-54S.
- Wu JC, Ko CC, Yen YS, Huang WC, Chen YC, et al. (2013) Epidemiology of cervical spondylotic myelopathy and its risk of causing spinal cord injury: A national cohort study. Neurosurg Focus 35(1): E10.
- Aljuboori Z, Boakye M (2019) The natural history of cervical spondylotic myelopathy and ossification of the posterior longitudinal ligament: A review article. Cureus 11(7): e5074.
- Watkins RG, Watkins RG (2021) Cervical disc herniations, radiculopathy and myelopathy. Clin Sports Med 40(3): 513-539.
- Qiu Y, Xie Y, Chen Y, Ye J, Wang F, et al. (2020) Adjacent two-level anterior cervical discectomy and fusion versus one-level corpectomy and fusion in cervical spondylotic myelopathy: Analysis of perioperative parameters and sagittal balance. Clin Neurol Neurosurg 194: 105919.
- Mc Cormick JR, Sama AJ, Schiller NC, Butler AJ, Donnally CJ (2020) Cervical spondylotic myelopathy: A guide to diagnosis and management. J Am Board Fam Med 33(2): 303-313.
- You JY, Zheng Y, Chen M, Fan JR (2017) Anterior versus posterior approach for multilevel cervical spondylotic myelopathy: A meta-analysis. Zhongguo Gu Shang 30(1): 71-78.
- Thirumala PD, Muralidharan A, Loke YK, Habeych M, Crammond D (2016) Value of intraoperative neurophysiological monitoring to reduce neurological complications in patients undergoing anterior cervical spine procedures for cervical spondylotic myelopathy. J Clin Neurosci 25: 27-35.
- Karadimas SK, Gatzounis G, Fehlings MG (2015) Pathobiology of cervical spondylotic myelopathy. Eur Spine J 24 (Suppl 2): 132-138.
- Yu Z, Chen C, Yu T, Ye Y, Zheng X, et al. (2023) Electrophysiological evidence of diabetes' impacts on central conduction recoveries in degenerative cervical myelopathy after surgery. Eur Spine J 32(6): 2101-2109.
© 2025 ianfeng Zhang, Fei Gao. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






