- Submissions

Full Text
COJ Nursing & Healthcare
Polycystic Ovary Syndrome in Women: A Cross-sectional Study to Investigate the Prevalence, Psychophysiological Manifestations, Risk Factors and Treatment
Rehan Rustam1, Aqsa Qaisar1*, Wajahat Ashraf2, Ayesha Usmani2, Muhammad Awais Bin Abdul Malik3, Maryam Sikandar1, Muhammad Adnan1 and Sameen Abbas1
1Department of Pharmacy, Quaid-I-Azam University, Pakistan
2Baqai Medical University, Pakistan
3Sheikh Zayed Medical College, Pakistan
*Corresponding author: Aqsa Qaisar, Department of Pharmacy, Quaid-I-Azam University, Pakistan
Submission: September 11, 2024;Published: October 21, 2024

ISSN: 2577-2007Volume9 Issue2
Abstract
Background: Polycystic Ovary Syndrome (PCOS) is a prevalent endocrine disorder that has significant implications for women. Despite its impact, the specific characteristics of PCOS remains understudied. Our cross-sectional study aimed to investigate the prevalence, psychophysiological symptoms, risk factors, and treatment associated with PCOS women.
Methods: Data were collected through an online questionnaire form, which yielded 88 responses, of which 49 (55.68%) were clinically diagnosed with PCOS, and 39 (44.32%) weren’t diagnosed but were symptomatic.
Results: Our study found the highest prevalence (46.9%) in the 20-30 years age group. Psychophysiological symptoms were prominent, with severe hirsutism (53.06%), difficulty in maintaining ideal weight (63.25%), menstrual irregularity (61.22%), and mood changes/depression (79.59%). Genetic predisposition (32.65%) and dietary habits (52.07%). Our results proved diet as a significant risk factor, with 63.26% of PCOS women reporting frequent chicken consumption, showing the need of further research to find a potential link between chicken consumption and PCOS development. Complications, specifically infertility (34.69%), were prevalent among diagnosed participants. Treatment strategies primarily focused on lifestyle modifications including dietary improvement (10.20%), weight loss (14.28%), and pharmacotherapy (73.46%), underscoring the multifaceted management approach required for PCOS.
Conclusion: Our study highlights the importance of awareness, early diagnosis, dietary control, and lifestyle modifications in effectively managing symptoms, treating PCOS, and reducing the overall disease burden.
Keywords:PCOS; Epidemiology; Hyperandrogenism; Amenorrhea; Infertility; Chicken
Abbreviations:PCOS: Polycystic Ovary Syndrome; DHEAS: Dehydroepiandrosterone Sulfate; 3β-HSD: 3β-hydroxysteroid dehydrogenase; QOL: Quality of Life; SHBG: Sex Hormone Binding Globulin; FSH: Follicle-Stimulating Hormone; LH: Luteinizing Hormone
Introduction
PCOS is among the most common endocrine disorders in young women [1,2]. It is characterized by delayed anovulation, laboratory and clinical signs of hyperandrogenism, and ultrasound findings showing polycystic microscopic ovaries [3]. Obstetrical problems involve female reproductive organs influenced by estrogen [4]. Some issues specific to women can be resolved, while others are life-threatening or persistent, affecting fertility. Conditions such as amenorrhea, endometriosis, PCOS, fibroids, most ovarian cancers, infertility, miscarriage, ectopic pregnancy, and premature birth are among the frequently observed reproductive and hormonal abnormalities associated with this condition [4].
Prevention, screening, diagnosis, and treatment of illnesses aims to promote the well-being and overall health of women [5,6]. This hyperandrogenic condition is ranked as the most established endocrinologic disorder affecting girls, with an envisioned occurrence of 8% to 13% among women during their reproductive age [5,7]. While remarkably common, this complex condition poses challenges in diagnosis and treatment, often because primary symptoms can vary with age, requiring personalized therapeutic approaches for patient health needs [6,7]. However, PCOS patients can also exhibit reproductive, endocrine, metabolic, and psychological symptoms and are often associated with multiple conditions [8,9].
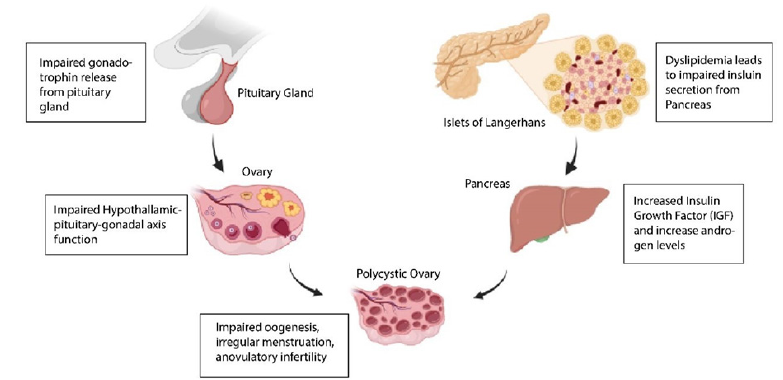
Excess Luteinizing Hormone (LH), irregular ovulation cycles, hyperandrogenism, abnormal follicular production, reduced fertility, and an increased risk of miscarriage are problematic hormonal and reproductive characteristics [7]. Global research on the regional differences in PCOS prevalence has been conducted recently. PCOS prevalence figures ranges from 2% to 26% [10]. Regional variations in incidences can be attributed to several key factors including diagnostic standards, pattern range, socioeconomic reputation, access to healthcare, occurrence of applicable chance factors, and degrees of fitness schooling and recognition inside communities [11]. PCOS is a complex and multifaceted circumstance that entails genetic, environmental, and intergeneration elements [12]. The main Underlying factors include Insulin resistance, hyperandrogenism, and hormonal imbalance as in Figure 1. The disruption in signaling in the hypothalamus pituitary ovarian axis, causes hyperandrogenism within the ovaries and adrenal glands. Additionally, disorders of adipose tissue associated with hyperandrogenism, mainly lipotoxicity and oxidative stress, further exacerbate insulin resistance as shown in Figure 2. Therefore, the syndrome includes abnormalities related to metabolism, reproduction, and psychology [7]. Women recognized with PCOS are significantly vulnerable to experiencing depressive issues and a dwindled satisfaction of life [13].
Figure 1:Contributors of PCOS.
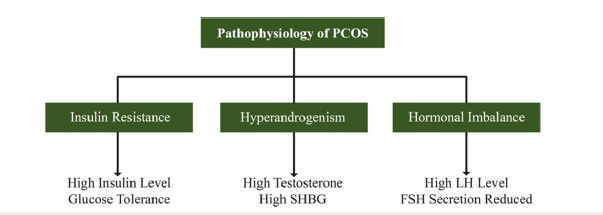
Figure 2:Overview of the pathophysiology of PCOS.
As heightened androgen stages stay the maximum consistent symptom of PCOS, hyperandrogenism is a number one characteristic, with about 60% of sufferers showing this trait as consistent with the Rotterdam definition [7]. In women identified with hyperandrogenic PCOS, the serum tiers of several androgens, inclusive of testosterone, androstenedione, Dehydroepiandrosterone Sulfate (DHEAS), and the enzyme 3β-Hydroxysteroid Dehydrogenase (3β-HSD), important for the seasoned androgens conversion to bioactive androgens, are extended [7]. Insulin resistance and hyperinsulinemia can lower sex hormone binding globulin which results in an elevation in unfastened androgens and unfavorable metabolic profiles, leading to hyperandrogenism [10]. PCOS is influenced by the environment and have genetic links [14]. In those who are vulnerable, obesity exacerbates PCOS, which is further worsened by poor food choices (Diet) and physical inactivity [15].
Women recognized with PCOS might also manifest different metabolic and cardiovascular irregularities, alongside psychological conditions like despair, tension, demanding situations in relationships, and sexual dysfunction [14]. Moreover, irregular menstruation, hirsutism, and infertility, will be present in affected women [16,17]. PCOS also affects the Quality of Life (QoL) due to mood problems, weight gain, hair loss, acne, infertility, and irregular menstruation [18].
Furthermore, studies have shown that modifying lifestyle factors can improve the quality of life [19]. PCOS requires personalized treatment. For teens, goals are normalizing weight, menstruation, and reducing hyperandrogenism. Collaboration among doctors, dietician, and psychologist may aid in management of weight. Promoting a healthy lifestyle helps maintain a normal body mass index. Medical therapy depends on clinical presentation [20]. Additionally, treating PCOS symptoms such as acne and hair development with birth control pills and other medications can help manage the menstrual cycle [21]. Oral contraceptives, metformin (off-label use), eflornithine (topical cream for hirsutism), and spironolactone are medications used to treat PCOS [16]. Adolescents who exhibit isolated irregularities in their cycles could be prescribed a cyclical progestin prescription in order to cause withdrawal symptoms [22].
Metformin relieves several hormonal imbalances and restores menstruation in a significant percentage of patients by reducing insulin resistance [18]. Combining progestin and oral contraceptives having estrogen increases Sex Hormone Binding Globulin (SHBG) degrees, leading to a decrease in unfastened testosterone, also helps in hirsutism and acne. In addition, these contraceptives also decrease the ranges of LH and Follicle Stimulating Hormone (FSH) [21]. This results in the return of menstrual cycles and a reduction in hirsutism by restoring endometrial cyclic exposure to estrogen-progestin. On the other hand, using oral contraceptives can raise your risk of thrombosis and metabolic problems. It is recommended to opt for an oral contraceptive comprising ethinyl estradiol and a progestin with minimal androgenic results, consisting of desogestrel and norethindrone [21]. When coupled with diprospirenone (Yasmin), diprospirenone-ethinyl estradiol possesses a progestin that functions as an antiandrogen and thus can have additional antiandrogenic effects [21]. The aims and objectives of our study are to assess the prevalence of PCOS, including both diagnosed cases and those with symptoms but not yet diagnosed, to evaluate psychophysiological symptoms and their severity, assess the risk factors and its association with PCOS, to identify further complications, treatment strategies and to make recommendations for future research areas to support findings and improve the PCOS healthcare programs.
Methods
Study overview
We conducted a cross-sectional study to investigate the epidemiology of PCOS, focusing on different age groups, prevalence of psychophysiological manifestations, associated risk factors, and treatment approaches. Data was collected from Pakistan at a single point in time between March 2024 and June 2024, providing a snapshot of PCOS prevalence rates and demographic distributions.
Ethical consideration
Our study was performed under ethical consideration. Informed consent was taken from all participants of the study. The participation was done on voluntary basis. Complete confidentiality was ensured throughout the research.
Study population
All women aged 15 to 60 years, either diagnosed or undiagnosed still symptomatic with Polycystic Ovary Syndrome (PCOS) were considered for study between specified study time period. We got data from 88 participants; out of them 49 women were diagnosed with PCOS and 39 women were symptomatic but never went for diagnosis.
Sampling technique
We employed snowball sampling technique. We began with small group of women who meet our selection criteria in gynae ward of Polyclinic Hospital Islamabad, and these initial participants then referred others who also meet the criteria. Our inclusion criteria includes (1) women diagnosed with PCOS, (2) women not diagnosed with PCOS still have symptoms, (3) Collected data from Pakistan, (4) Time period between March, 2024 and June, 2024, and our exclusion criteria includes (1) women with other reproductive diseases other than PCOS, (2) Data from Other countries.
Study procedure
For the development of our questionnaire, we adhere to principles ensuring clarity, relevance, and inclusively. We crafted questions using straightforward language, accessible to our target population, aiming to avoid any leading or biased inquiries that might skew responses. Each question is meticulously designed to align with our research objectives, covering all pertinent topics related to the epidemiology of PCOS. Our questionnaire included closed-ended and open-ended questions. This included demographic information, physiological manifestations such as hirsutism, challenges in maintaining ideal weight, and menstrual issues, as well as psychological manifestations including mood changes and depression. We also explored the association of risk factors such as genetic predisposition and diabetes. Potential complications, such as infertility, endometrial thickness, and fibroids, were also assessed. Additionally, common dietary habits were evaluated. Before finalizing the questionnaire, we conducted a pilot test with a small group resembling our target population to identify any potential issues such as confusing wording or missing questions, ensuring the instrument’s comprehensibility and efficacy.
Assessments & statistical analysis
We performed data analysis by using python and associated libraries on Google Collab. First we done Data manipulation by using Numpy and Pandas then we draw plots of by using Matplotlib and Seaborn libraries. We formulated Contingency Table of Age, Physiological and Psychological manifestation, Genetics, Diabetes, Diet, Complications, and Treatment relative to the PCOS Diagnosis data separately by using Pandas library and we applied Chi-square test by using scipy stat module to each contingency table which has given p-value. On the basis of p-value we interpreted results.
Results
Our cross-sectional study included data from 88 participants. We screened 49 women with clinically diagnosed PCOS and 39 symptomatic women who were not yet diagnosed. The data on prevalence, psychophysical symptoms, and risk factors are presented in Table 1.
Table 1:Characteristics and specifics of diagnosed and undiagnosed individuals with PCOS.
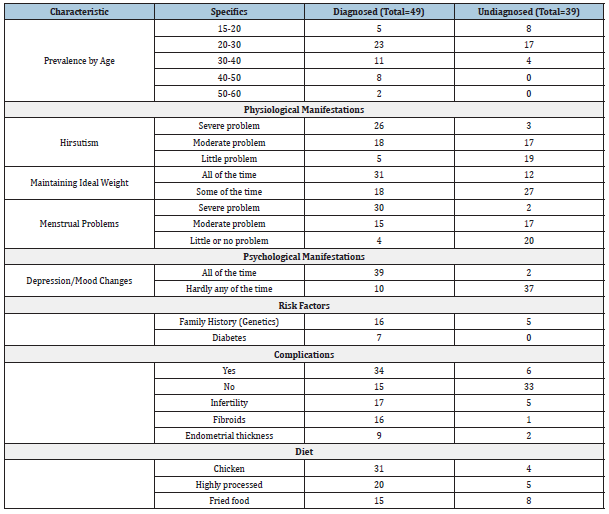
Prevalence
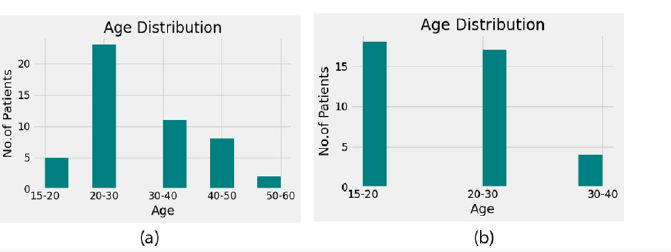
Of the 88 participants in our study, 49 women (55.68%) had PCOS while 39 individuals (44.32%) had PCOS symptoms but were not diagnosed. This showed the variability in the diagnosis of PCOS within the study cohort, which highlights the significance of thorough clinical examinations, hormone testing, and imaging modalities in ensuring accurate diagnosis and providing pathways emphasizing appropriate management customized to meet the needs of individual patients (Figure 3).
Age: There was a notable variation in the prevalence of PCOS across different age groups, with the age range of 20-30 years (46.9%) exhibiting the highest frequency. The distribution among other age groups is as follows: 15-20 years (10.20%), 30-40 years (22.44%), 40-50 years (16.32%), and 50-60 years (4.08%). Statistical evaluation revealed a significant association between age and the development of PCOS (P=0.05). We considered demographic factors including age, 50% of women married, belonged to Punjabi ethnicity background, and all were educated. In a similar way, our findings revealed a small number of symptomatic individuals, but without a PCOS diagnosis. The majority of this undiagnosed population (46.15%) was in the 15–20 age range as shown in Figure 3.
Figure 3:Age distribution of diagnosed (A) and Undiagnosed (B) Individuals with PCOS.
Physiological manifestation:
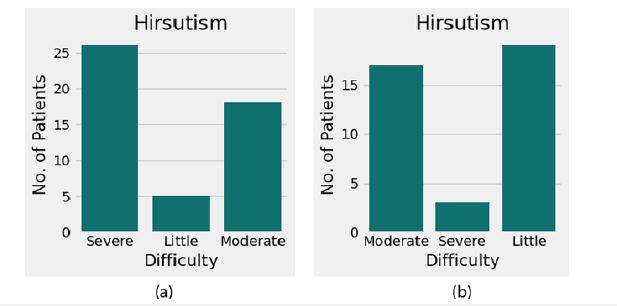
A. Hirsutism: The most prevalent indication of PCOS, hirsutism, we used ordinal scale to find severity of hirsutism. It was found to be severely distributed across 26 women (53.06%) in our study. Five of the women (10.20%) have a little problem, while eighteen have significant symptoms. A significant correlation between PCOS and hirsutism was found by the statistical testing (P=0.05). Similarly, other women who have reported experiencing hair growth on their faces, chins, or upper lips but have not received a PCOS diagnosis. Among them, three women (7.69%) had severe hirsutism, 17 women (43.8%) had moderate, and 19 women (48.71%) had mild hirsutism as shown in Figure 4.
Figure 4:Severity of hirsutism in diagnosed (A) and Undiagnosed (B) Individuals with PCOS.
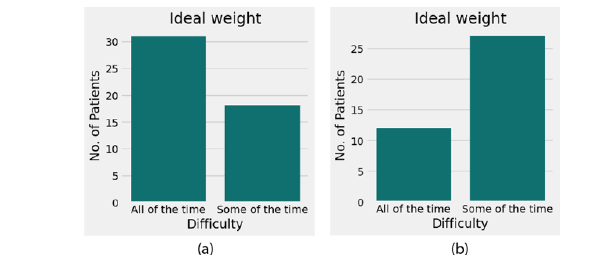
B. Body weight: PCOS symptoms can appear in overweight women and can have increased risk of various long-term health issues. 63.25% of the women in our survey reported that it was difficult for them to maintain their optimum weight. While 36.73% occasionally had difficulties. Likewise, 30.07% of the women in our undiagnosed PCOS group have reported severe difficulty in maintaining the ideal weight(p=0), and 69.23% of them struggled to stay that way sometimes as shown in Figure 5.
Figure 5:Distribution of ideal weight maintenance among diagnosed (A) and Undiagnosed (B) Individuals with PCOS.
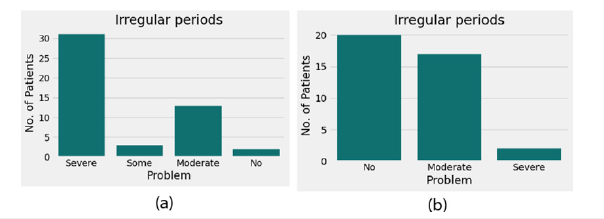
C. Menstural problems: According to our study, 30 women (61.22%) had a very noticeable incidence of severe irregular menstrual periods, whereas 15 women (30.61%) had moderate irregular periods and 4 women (8.16%) had little to no abnormal menstrual flow. The statistical testing revealed a significant association (P=0.05) between menstrual cycle and PCOS. In the same way, among the women in our undiagnosed group, 2 (5.12%) had severe irregularities in their menstruation yet symptomatic; 17 (43.58%) had moderate irregularities; and 20 (51.28%) had little to no irregularities in their menstruation as shown in Figure 6.
Figure 6:Severity of irregular periods in diagnosed (A) and Undiagnosed (B) Individuals with PCOS.
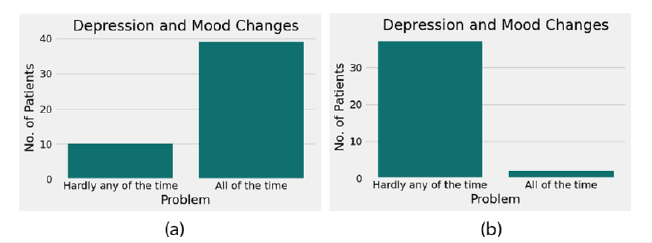
Psychological manifestation: Women with PCOS often have reported mood changes and depression in different phases of the disease. Our survey reported 39 of the women (79.59%) have had severe changes in their mood that eventually resulted in anxiety and depression. While remaining 10 women (20.40%) have barely experienced depression. The statistical testing revealed a significant association (P=0.05) between depression and PCOS. Of the women in our undiagnosed group, 37 (94.87%) showed very little symptoms of depression, while 2 (5.12%) had experienced severe symptoms represented in Figure 7.
Figure 7:Frequency of depression and mood changes in diagnosed (A) and Undiagnosed (B) Individuals with PCOS.
Risk factors
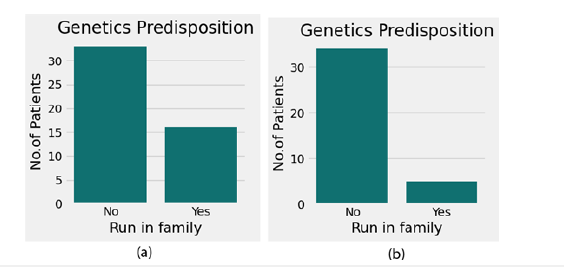
Genetic predisposition: Of the individuals, 32.65% (16 out of 49) identified genetic factors as the prime diagnosis of PCOS, whereas 12.82% (5 out of 39) of the undiagnosed group claimed having PCOS symptoms because the condition ran in their family. Despite experiencing the symptoms, they did not receive a diagnosis of the PCOS as shown in Figure 8.
Figure 8:Genetic predisposition to PCOS in diagnosed (A) and Undiagnosed (B) Individuals.
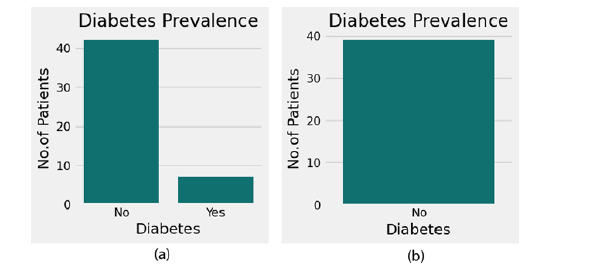
Diabetes: Among the participants, 7 out of 49 women (14.28%) claimed that their diabetes was a contributing reason to their PCOS, but none of the 39 women in our undiagnosed PCOS group had diabetes which could aggravate the symptoms of PCOS. A statistical investigation revealed a strong correlation between the PCOS and diabetes (P=0.05) as shown in Figure 9.
Figure 9:Prevalence of diabetes in diagnosed (A) and Undiagnosed (B) Individuals with PCOS.
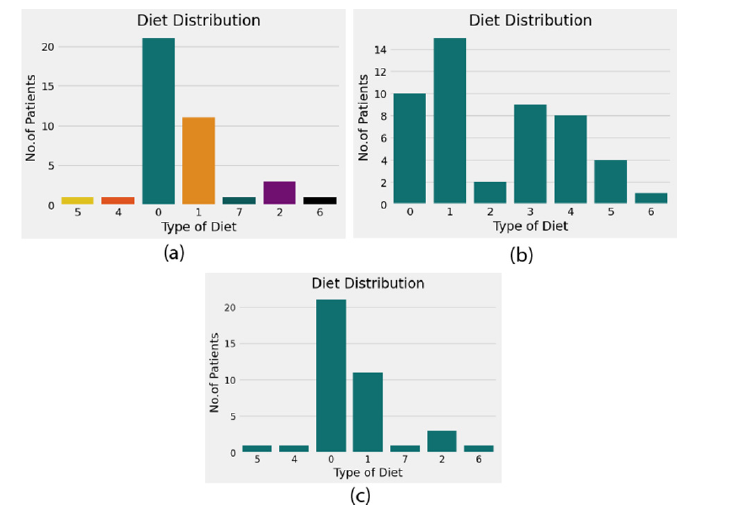
Diet: One of the causes of PCOS is a diet rich in fried foods and refined carbs. In our study, 52.07% of the diagnosed women claimed that it could be related to their dietary habits. Eating a diet heavy in processed foods, fried foods, and chicken was the main reason why women with PCOS had this condition. Women who ate chicken had a 63.26% incidence, those who consumed highly processed food had a 40.81% incidence, and those who consumed more fried food had a 30.61% incidence of PCOS. The study revealed a significant association between diet and the development of PCOS (P=0.05). 4 of the 39 women (10.25%) in our undiagnosed PCOS group, having symptoms, ate chicken, five (12.82%) consumed highly processed meals, and eight (20.51%) consumed fried food. Diet contains one or more food mixtures respective to their numbers which include Fried food, Chicken, Refined Wheat, Cold Drinks, Highly processed carbohydrates like pasta, margarine, Dairy foods such as creams or cheese, red or processed meat represented in Figure 10.
Figure 10:Diet distribution among diagnosed (A, B) and Undiagnosed (C) Individuals with PCOS.
Complications
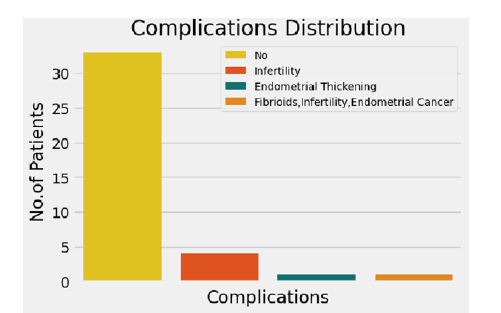
Regarding complications, 15 women (30.61%) reported having no other PCOS-related complication, whereas 34 participants (69.38%) reported having additional health concerns associated to PCOS. 9 (26.4%) of the women diagnosed with PCOS experienced problems related to endometrial thickness, 16 (32.65%) experienced fibroids as a consequence, and 17 (34.69%) experienced infertility. Statistical evaluation revealed a significant association between developing complications and the PCOS (P = 0.05) Among undiagnosed yet symptomatic women, 2 women (5.12%) suffered from endometrial thickness, 1 women (2.56%) experienced fibroids and 5 women (12.82%) became infertile as shown in Figure 11 & 12.
Figure 11:Complications among diagnosed individuals with PCOS.
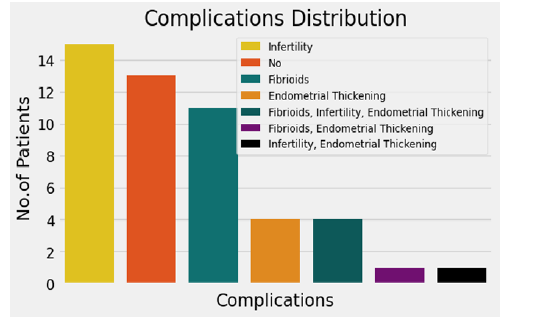
Figure 12:Complications among undiagnosed individuals with PCOS.
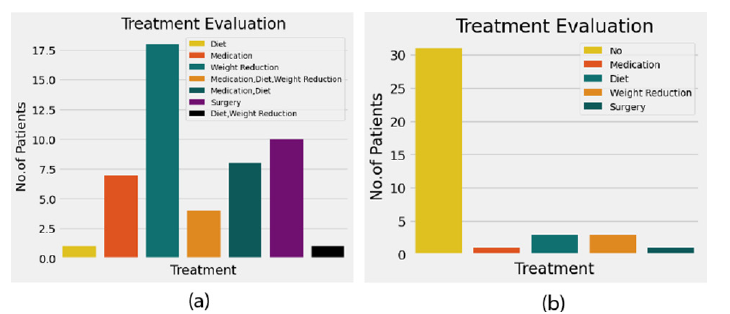
Treatment
The study revealed a variety of treatment strategies for managing PCOS. Lifestyle changes, including dietary improvements (10.20%) and weight loss (14.28%), were recommended most frequently. 73.46% of participants reported medication therapy. Surgery was the least common treatment, reported by 2.04% of participants as shown in Figure 13. Our study of 88 women revealed that 49(55.68%) were diagnosed with PCOS, with the highest prevalence in the 20-30 age group (46.9%). Key symptoms included severe hirsutism (53.06%), menstrual irregularities (61.22%), and mood changes (79.59%). Genetic predisposition (32.65%), diet (52.07%), and diabetes (14.28%) were significant risk factors, with complications such as infertility (34.69%) and fibroids (32.65%) being common. Treatment primarily involved lifestyle changes and medication (73.46%), emphasizing the need for personalized management.
Figure 13:Treatment evaluation for diagnosed (A) and Undiagnosed (B) Individuals with PCOS.
Discussion
In our cross-sectional study, we considered prevalence, psychophysiological impact, risk factors, and treatment together. Our study found overall prevalence to be 55.7% with p=0 showing significant association. The prevalence is high (46.9%) in 20- 30 aged women. Various studies were performed to assess the prevalence psychological symptoms in PCOS women. A Case Study was performed to assess the Psychophysiological Impact of PCOS and its Management in Women of Pakistan [23].
Psychophysiological manifestations showed in our study that all of them faced hirsutism 52.06% (p = 0.05), menstrual irregularities 61.22% (p=0.05), and difficulty in maintaining ideal weight 63.25% (p = 0.05). One cross-sectional study performed found depression symptoms in 13 (17.6%) cases [24]. Our study shows a reduced 79.59% (p=0.05) prevalence of psychological manifestation in diagnosed PCOS women. One comparative crosssectional study was performed at one hospital and found high Insulin resistance in PCOS females than in non-PCOS females. Body mass index also led to high insulin resistance [25]. Our study differs because it showed a reduced association of risk factors with PCOS; diabetes (14.28%) and genetic predisposition (32.65%) with PCOS development as compared to previous studies. One study revealed that lifestyle factors, specifically nutrition and physical exercise, exerted an impact on insulin sensitivity, weight regulation, and reproductive health among women diagnosed with PCOS [26]. Major contributing risk factor found in our study is diet (53.07%). specifically, chicken (63.26%), high processed carbohydrates like pasta (40.81%), and fried food (30.61%). The reason is lavish dietary habits of women and it led to further complications with fibroids (32.65%), endometrial thickness (26.4%), and infertility (34.69%). Infertility appeared highest in our results. Treatment administered to the PCOS women was varied, with most of the women being given medication therapy to counteract the symptoms of the disease. Others were prescribed changes in lifestyle habits and reducing excessive weight.
Our study showed that risk factors including genetic predisposition, diabetes, and diet are involved in the development of PCOS. PCOS does run in the family and insulin resistance in diabetic women also leads to PCOS development. Diet is the main contributing risk factor. This is due to the lavish dietary habits and sedentary lifestyle of the women now-a-days. The most common foods among them were chicken, highly processed carbohydrates like pasta and fried food. So, our study gives future recommendations to do research on poultry chicken to identify mechanisms involved in development of PCOS. There should be a prohibition on chicken at the public level to improve women’s health. It is also proved in our study that dietary modification with medication therapy resulted in better management of PCOS. Physicians should consider dietary modification first to manage symptoms and treat PCOS. Our study considered community women having symptoms of PCOS but weren’t diagnosed with PCOS showing unawareness of PCOS in women. So, there should be public awareness programs to increase the knowledge of women regarding PCOS development and to effectively reduce the burden of PCOS in women.
Conclusion
Based on our study, PCOS is a significant health challenge among women, particularly prevalent in the 20-30 age group. Key risk factors include genetic predisposition, diabetes, and poor dietary habits, with major symptoms including cardiovascular issues, menstrual irregularities, and psychological problems. While dietary modifications and medications are the primary treatments, surgery is rarely needed. The study underscores the importance of early diagnosis and personalized treatment plans. To transform PCOS management, we recommend launching community-driven health tech initiatives, such as mobile apps for symptom tracking and personalized dietary guidance. Pairing these tools with interactive workshops on lifestyle modifications and diet can foster proactive management. Additionally, creating local support networks and leveraging telemedicine for continuous care can significantly enhance access and engagement. Public awareness programs should focus on the impact of dietary pat- terns—particularly the consumption of fried foods, chicken, and high-carbohydrate diets. Due to limitations such as time constraints, limited resources, and lack of funding, the findings cannot be generalized to a broader population.
References
- Jabeen A, Yamini V, Amberina AR, Eshwar MD, Vadakedath S, et al. (2022) Polycystic ovarian syndrome: Prevalence, predisposing factors, and awareness among adolescent and young girls of South India. Cureus 14(8): e27943.
- Singh V, Mahra K, Jung D, Shin JH (2024) Gut microbes in polycystic ovary syndrome and associated comorbidities; type 2 diabetes, Non-Alcoholic Fatty Liver Disease (NAFLD), Cardiovascular Disease (CVD), and the potential of microbial therapeutics. Probiotics and Antimicrobial Proteins 16(5): 1744-1761.
- Azziz R, Carmina E, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale HF, et al. (2009) The androgen excess and PCOS society criteria for the polycystic ovary syndrome: The complete task force report. Fertility and Sterility 91(2): 456-488.
- Patel S (2018) Polycystic Ovary Syndrome (PCOS), an inflammatory, systemic, lifestyle endocrinopathy. The Journal of Steroid Biochemistry and Molecular Biology 182: 27-36.
- Carmina E, Lobo RA (1999) Polycystic ovary syndrome (PCOS): Arguably the most common endocrinopathy is associated with significant morbidity in women. The Journal of Clinical Endocrinology & Metabolism 84(6): 1897-1899.
- Legro RS, Arslanian SA, Ehrmann DA, Hoeger KM, Murad MH, et al. (2013) Diagnosis and treatment of polycystic ovary syndrome: An endocrine society clinical practice guideline. The Journal of Clinical Endocrinology & Metabolism 98(12): 4565-4592.
- Rodriguez Paris V, Bertoldo MJ (2019) The mechanism of androgen actions in PCOS etiology. Medical Sciences 7(9): 89.
- Palomba S, Santagni S, Falbo A, La Sala GB (2015) Complications and challenges associated with polycystic ovary syndrome: Current perspectives. International Journal of Women’s Health 7: 745-763.
- Parker J, O’brien C, Hawrelak J, Gersh FL (2022) Polycystic ovary syndrome: An evolutionary adaptation to lifestyle and the environment. International Journal of Environmental Research and Public Health 19(3): 1336.
- Hoeger KM, Dokras A, Piltonen T (2021) Update on PCOS: Consequences, challenges, and guiding treatment. The Journal of Clinical Endocrinology & Metabolism 106(3): e1071-e1083.
- Deswal R, Narwal V, Dang A, Pundir CS (2020) The prevalence of polycystic ovary syndrome: A brief systematic review. Journal of Human Reproductive Sciences 13(4): 261-271.
- Kshetrimayum C, Sharma A, Mishra VV, Kumar S (2019) Polycystic ovarian syndrome: Environmental/occupational, lifestyle factors; an overview. Journal of the Turkish German Gynecological Association 20(4): 255-263.
- Asdaq SMB, Jomah S, Hasan R, Al-Baroudi D, Alharbi M, et al. (2020) Impact of polycystic ovary syndrome on eating behavior, depression and health related quality of life: A cross- sectional study in Riyadh. Saudi Journal of Biological Sciences 27(12): 3342-3347.
- Zore T, Joshi NV, Lizneva D, Azziz R (2017) Polycystic ovarian syndrome: long- term health consequences. Seminars in Reproductive Medicine 35(3): 271-281.
- Diamanti-Kandarakis E, Kandarakis H, Legro RS (2006) The role of genes and environment in the etiology of PCOS. Endocrine 30(1): 19-26.
- Khomami MB, Tehrani FR, Hashemi S, Farahmand M, Azizi F (2015) Of PCOS symptoms, hirsutism has the most significant impact on the quality of life of Iranian women. PLoS One 10(4): e0123608.
- Dennett CC, Simon J (2015) The role of polycystic ovary syndrome in reproductive and metabolic health: Overview and approaches for treatment. Diabetes Spectrum 28(2): 116-120.
- Pinto J, Cera N, Pignatelli D (2024) Psychological symptoms and brain activity alterations in women with PCOS and their relation to the reduced quality of life: A narrative review. Journal of Endocrinological Investigation 47(7): 1-22.
- Kim CH, Lee SH (2022) Effectiveness of lifestyle modification in polycystic ovary syndrome patients with obesity: A systematic review and meta-analysis. Life 12(2): 308.
- Goodarzi MO, Dumesic DA, Chazenbalk G, Azziz R (2011) Polycystic ovary syndrome: etiology, pathogenesis and diagnosis. Nature Reviews Endocrinology 7(4): 219-231.
- Mukerjee N (2020) Polycystic Ovary Syndrome (PCOS) symptoms, causes & treatments a review. International Journal of Science and Research 9(7): 1949-1957.
- Franks S (2008) Polycystic ovary syndrome in adolescents. International Journal of Obesity 32(7): 1035-1041.
- Ullah M (2022) A case study: Psychophysiological impact of polycystic ovarian syn- drome and its management in Pakistani women: A case study: Psychophysiological impact of polycystic ovarian syndrome and its management in Pakistani women. Journal of Women Medical and Dental College 1(1): 10-16.
- Khan AYR, Abdullah MA, Gul R, Bhutta HR, Imran M, et al. (2024) Prevalence of anxiety and depression among women with polycystic ovarian syndrome: A cross-sectional study from a tertiary care hospital of Islamabad, Pakistan. Cureus 16(1): e52540.
- Khan SH, Shahid R, Aslam S, Manzoor R, Anwar R, et al. (2024) How significant are insulin resistance parameters in subjects with polycystic ovarian syndrome (PCOS)? a cross-sectional study. Pakistan Armed Forces Medical Journal 74(1): 36-40.
- Memon SI, Shakeel M, Syed H, Amin K, Khalil AA, et al. (2024) Prevalence, risk factors and management of polycystic ovary syndrome: A review with current evidence. Iraq Medical Journal 8(1): 1-5.
© 2024 Aqsa Qaisar. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






