- Submissions

Full Text
COJ Nursing & Healthcare
Survey-Guided Initiatives in Improving Nurses’ Attitudes, Perceptions and Practices of Antimicrobial Stewardship
Fritzie S Albarillo1*, Maressa Santarossa1, Christina Bley2 and Cara Joyce3
1Department of Medicine, Division of Infectious Diseases, Loyola University Medical Center, USA
2Department of Nursing, Loyola University Medical Center, USA
3Department of Medicine, Stritch School of Medicine, Loyola University Chicago, USA
*Corresponding author: Fritzie S Albarillo, Department of Medicine, Division of Infectious Diseases, Loyola University Medical Center, USA
Submission: June 13, 2024;Published: July 09, 2024

ISSN: 2577-2007Volume9 Issue1
Abstract
Background: Antimicrobial stewardship programs involve a multidisciplinary team which have shown to result in favorable patient outcomes, decreased healthcare costs, and reduction in Antimicrobial Resistance (AR). Nurses have been shown to be a vital part of Antimicrobial Stewardship (AS); however, their specific role and involvement in AS should require further investigation and delineation.
Methods: In February 2018, a voluntary online survey was disseminated to all Registered Nurses (RNs) at Loyola University Medical Center to assess their knowledge and perception of AS and AR, as well as to evaluate their AS-related activities. The results of the survey lead to an implementation of a multi-faceted program focused on education. In March 2019, a second survey was disseminated to all RNs investigating any changes in the knowledge and perception of AS and AR post implementation of our educational efforts, as well as to obtain feedback on how to further engage RNs in AS.
Results: 179 and 117 RNs completed the first and second surveys respectively. A significant percentage of the RNs in both surveys agreed that they play critical roles in AS, and that AS can lead to reduction in AR and complications of antimicrobials. However, more than half of the RNs report that they are not familiar with AS practices at our facility.
Conclusion: Local surveys on RNs knowledge, perception and practices on AS and AR can be utilized to improve stewardship efforts. Our team implemented strategies focused on education using pre-intervention and post-intervention surveys.
Keywords:Antimicrobial stewardship; Antimicrobial resistance; Nursing education; Surveys
Introduction
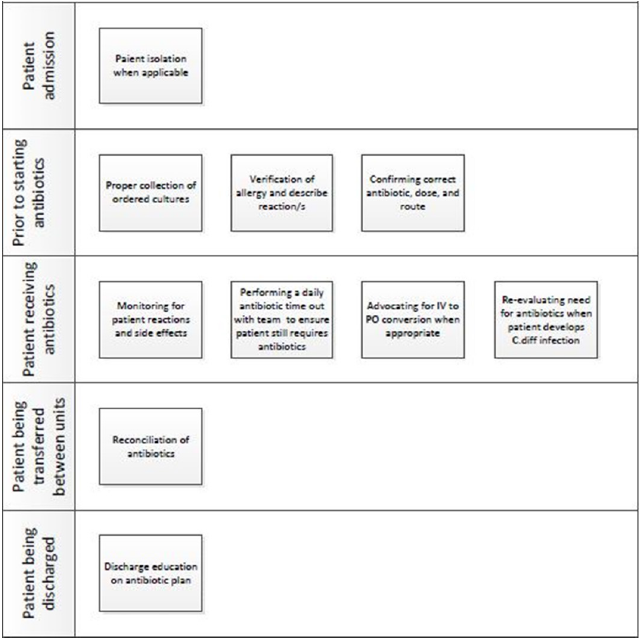
Antimicrobial resistance is now considered a global health threat by the US Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) [1-2]. This global phenomenon has been accelerated by overuse and misuse of antibiotics [3]. Up to 60% of hospitalized patients receive antibiotics, and 30% of these antibiotics are deemed unnecessary [4,5]. In order to combat this growing threat, acute care hospitals are required to form Antimicrobial Stewardship Programs (ASP). ASPs have been shown to improve antimicrobial utilization, patient outcomes, cost, and antimicrobial resistance [6-10]. The CDC recommends that all ASPs should meet the seven core elements in a multidisciplinary approach, and this has been enforced by The Joint Commission and Centers for Medicare and Medicaid Services [11-13]. Previous guidelines did not include roles of nursing in antimicrobial stewardship (AS). However, increasing nursing contributions to AS have been published in the literature [14-16]. In July 2016, the CDC in partnership with the American Nurses Association (ANA) held a joint conference in Maryland to discuss nurses’ roles in AS, and to specifically identify nursing-focused antimicrobial stewardship activities. A report of the conference was published detailing these activities in a white paper [17]. The nurses’ perspective and active engagement are critical to the success of AS. Nurses make up the largest segment of healthcare workers. They are directly involved in patient care providing consistency, continuity, and coordination of care for patients. Several publications have described nursing-driven AS activities [14,15,18]. Nurses perform AS-related activities from patients’ admission through discharge (Figure 1).
Figure 1:Nurses perform several AS-related activities from the patient’s admission through discharge.
Loyola University Medical Center (LUMC) is a quaternary caresystem in Maywood, IL, USA, with an existing multidisciplinary ASP that includes representation from the nursing department. LUMC has received Magnet® designation from the American Nurses Credentialing Center. This designation is given to facilities that provide an optimal environment for nurses to deliver the highest standard of care to their patients. Since there are now increasing efforts towards engaging nurses in AS, more information is warranted regarding gaps in nurses’ knowledge and perceptions of AS. Our team sought to assess RNs’ knowledge and perceptions of AS and AR, as well as their current engagement in AS-related activities. In the United States, a RN is an individual with a nursing diploma who has passed the National Council Licensure Examination (NCLEX-RN) examination.
Methods
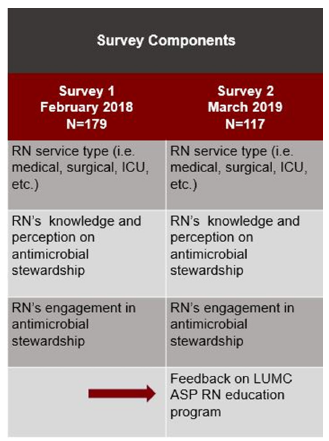
In February 2018, a voluntary anonymous online survey was developed using an online tool, Survey Monkey® (SurveyMonkey Inc.® Palo Alto, California, USA), and disseminated electronically to all RNs at LUMC. The first survey was composed of 20 questions categorized into 3 components: service type, knowledge and perception of AS and AR, and nurse engagement in AS. Likert-type questions were utilized for the second and third components. The instrument was developed by infectious diseases physicians and infectious diseases pharmacists. The questions were reviewed by the antimicrobial stewardship committee at LUMC. The goal of the first survey was to assess RNs’ knowledge and perception in AS and AR, as well as their practices in AS at LUMC. After approval of the study by the institutional review board, an electronic message was disseminated to all employed RNs at LUMC with an invitation to participate and a link to the survey. Participation was voluntary and no incentive was provided for participation. Paper surveys were also available and were distributed to RNs during a hospital-wide meeting. The answers of the paper survey were manually entered by the investigators. Based on the outcomes of the survey, our team implemented multi-faceted strategies focused on education that included PowerPoint slides that were electronically disseminated to all RNs, as well as live sessions during nurses’ huddles in Intensive Care and floor units discussing different roles of RNs in AS. In March 2019, a second survey was sent to all RNs with the primary focus of evaluating any changes in their knowledge and perception of AS and AR post implementation of our educational strategies. The questions on the second survey were identical to the first survey but with the addition of a fourth component in order to obtain feedback regarding our educational methods. Figure 2 describes the components of the surveys. Responses to questions on knowledge and learning preferences were presented as counts and percentages (Figure 2).
Figure 2:Components of Survey 1 and Survey 2.
Results
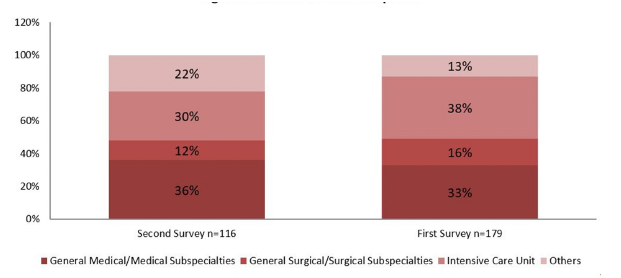
There were 179 RNs who completed the first survey, and 117 RNs who completed the second survey (Figure 3). The majority of respondents were from general medical and medical subspecialties.
Figure 3:Distribution of respondents for each survey.
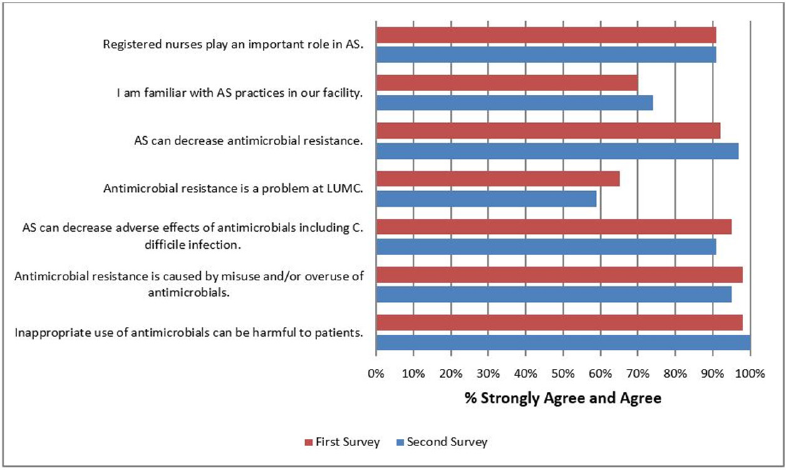
RNs’ knowledge and perception of AS and AR
Both surveys showed that majority of RNs agreed that they play important roles in AS, AS can lead to reduction in AR and adverse effects of antimicrobials, AR can be caused by inappropriate use of antimicrobials that can lead to harm for patients. Only 65% of RNs strongly agree/agree that AR is a problem at LUMC, which further decreased to 59% in the second survey. A majority of RNs were not familiar with AS practices in both surveys (Figure 4).
Figure 4:Nurses’ Knowledge and Perception of AS and AR.
RNs’ engagement in AS
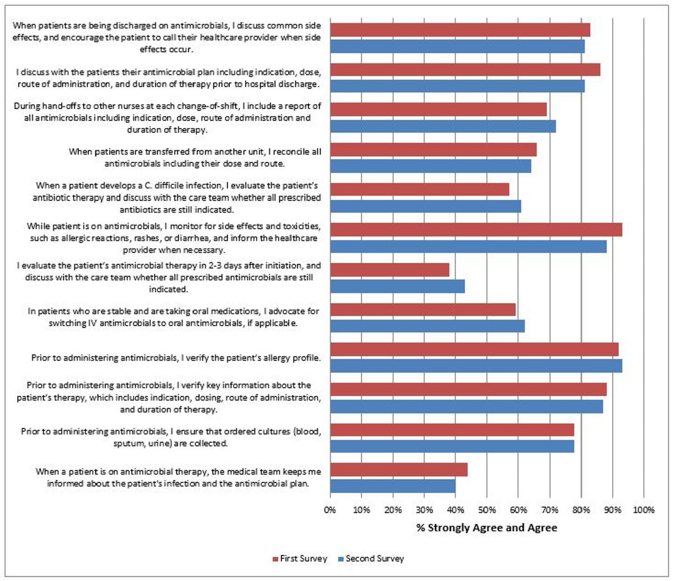
Overall, nurse related AS activities are encouraging in both surveys. More than 75% of the respondents for both surveys indicated that culture collection was ensured prior to administration of antimicrobials, while more than 80% indicated that they verify antimicrobial indication/dose/route/duration of therapy and antimicrobial allergies prior to administering antimicrobials, and that they monitor for side effects and toxicities while patients are receiving antimicrobials. In both surveys, more than 80% of respondents discuss the antimicrobial plan including side effects with patients upon discharge. Approximately 60-70% of the RNs include an antimicrobial report on shift changes and perform antimicrobial reconciliation when patients are transferred from units. RNs’ perception of their involvement in the antimicrobial plan appears to be subdued. Fifty-seven percent of RNs question the antimicrobial plan when patients develop Clostridioides difficile Infection (CDI), however, this slightly improved to 61% in the second survey. Fifty-nine percent of RNs indicate that they advocate for IV to PO switch in stable patients, and this rate slightly increased to 62% in the second survey. Only 44% of respondents affirmed their involvement in the patient’s antimicrobial plan, which decreased to 40% in the second survey. Finally, only 38% of the respondents evaluate the need for continuing antimicrobials, but this increased to 43% in the second survey (Figure 5).
Figure 5:Nurses’ Engagement in AS.
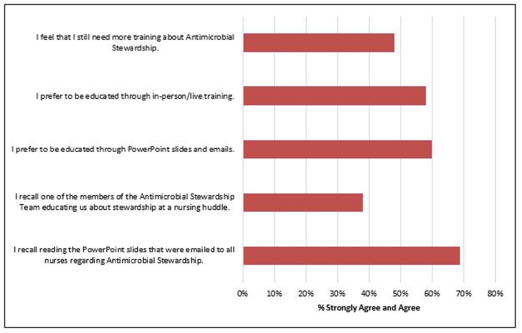
RNs’ feedback on education
More than half of respondents read the PowerPoint education slides, but only 38% recollected being educated during nursing huddles by our AS team. Majority of the RNs prefer live over electronic education (Figure 6).
Figure 6:RN’s Feedback on Education.
Discussion
Several surveys on knowledge and perceptions on AS and AR have been utilized to understand the drivers of antibiotic prescription and to further AS efforts [19-22]. It has been widely accepted that infectious diseases physicians and pharmacists are the leaders of ASPs. However, there is an urgent call to include other members of the healthcare workforce in AS involvement [23,24]. Nurses are integral members of the healthcare team and their engagement in AS is critical. Nurses are known to be involved in infection control measures and prevention [25-28]. Moreover, nurses have played essential roles in quality improvement initiatives in infection prevention [29-31]. However, much is unknown about nurses’ optimal roles in AS. Understanding the knowledge and perceptions of nurses is a fundamental initial step in delineating their roles in AS. Similar surveys have also aimed to evaluate nurses’ knowledge and perception on AS and AR [32-36].
Our study demonstrated that the respondents had a favorable understanding of AS and AR, however, most are not familiar with our institution’s AS activities which is also reflected in surveys at other institutions [33-35]. A study by Merrill et al. evaluated nurses’ knowledge of antimicrobial utilization and resistance, as well as assessed their attitudes in AS involvement. This survey demonstrated that 52% of the respondents were not familiar with AS, however, 95% agreed that they should be involved in AS [33]. Similarly, the majority in our study’s RNs did not believe that AR is a problem at our institution. This discrepancy was also observed in a recent study by Perez et al. where 92% of their surveyed nurses agreed that antimicrobial resistance is a significant problem nationally, but only 35% agreed that this was a problem in their institution [35]. This gap can likely be overcome by sharing facility antibiograms and rates of resistant organisms [33]. Currently, our RNs are familiar with their unit’s infection control-related metrics, such as Catheter-Associated Urinary Tract Infection (CAUTI) and Central Line-Associated Blood Stream Infection (CLABSI) rates as shared by our Infection Control Committee. However, current reporting of AS-related metrics is only limited to medical staff and the pharmacy department. This challenge has also been demonstrated by Abera et al. where a larger proportion of RNs reported they have not received information on antimicrobial resistance compared to physicians [36,37].
Our surveys showed that the most common AS-related activities RNs are engaged in are monitoring for side effects and toxicities of antimicrobials, verifying allergies, discharge education on antimicrobial plan, verifying antimicrobial details prior to administration, and obtaining cultures prior to administration of antimicrobials. Assessment of the need to continue antimicrobials and discussion with the treating team is an area RNs report they rarely perform. This has also been demonstrated in other studies and may be attributed to a lack of understanding of their roles in AS [36,38,39]. Moreover, nurses perceive that physicians are solely responsible for antimicrobial de-escalation, and that questioning the doctors’ medical decisions may lead to conflict and disregard of their authority [36,40]. This area of concern provides an opportunity to implement strategies that can empower nurses in their roles in AS and patient safety. Gillespie et al. evaluated nurses’ knowledge and attitudes on AS with pre-and post-education involvement, focusing on questioning medical staff about the antibiotic plan. Post intervention, the percentage of nurses questioning the medical staff regarding antibiotic order increased from 71% to 91% [41]. Involving nurses during ward rounds can also improve their involvement in the patient’s antibiotic plan [18]. Several studies have demonstrated that multidisciplinary rounding involving nurses led to improved patient satisfaction and outcomes [42-44].
Education on AS is critical not only for physicians but for every member of the healthcare team, including nurses. Our survey showed that less than 50% of the respondents indicated they need more education on AS, reflecting increased confidence in their knowledge of AS. In contrast, other surveys revealed that nurses identified lack of education as a barrier in AS [34,36,39]. Most nurses in a survey by Padigos et al, indicated that lectures and continuing education modules are the preferred tool of education [34]. In comparison, RNs in our survey preferred PowerPoint slides and emails.
We have identified several limitations in our study. Aside from having a small sample size, our surveys were answered anonymously and voluntarily which did not allow for direct comparisons of pre- to post-test change nor assessment of survey OF non-responders. Moreover, since the PowerPoint slides were disseminated electronically, we lacked reliable ways of measuring compliance. Finally, since we were not able to attend all nursing huddles, a significant portion of nursing staff may not have been captured with this educational strategy.
Conclusion
The nurses’ perspective and active engagement are critical in the success of AS, as they make up the largest segment of healthcare workers and are directly involved in patient care. Roles of nurses in AS is not well defined. Our ASP at LUMC implemented multi-faceted interventions to expand nursing education and engagement in AS. We then evaluated this strategy by utilizing pre and post surveys. Our surveys show that LUMC RNs have a superior understanding of AS and AR, however, most are not familiar with our AS activities. Our surveys also demonstrated notable AS engagement among LUMC RNs. However, more education is needed to re-enforce their engagement. Surveys will continue to be utilized in assessing AS interventions and educational efforts at LUMC.
References
- Antibiotic/antimicrobial resistance. Center for Disease Control and Prevention (CDC), Georgia, USA.
- Antimicrobial resistance. World Health Organization (WHO), Geneva, Switzerland.
- Llor C, Bjerrum L (2014) Antimicrobial resistance: Risk associated with antibiotic overuse and initiatives to reduce the problem. Therapeutic Advances in Drug Safety 5(6): 229-241.
- Baggs J, Fridkin SK, Pollack LA, Srinivasan A, Jernigan JA (2016) Estimating national trends in inpatient antibiotic use among US hospitals from 2006 to 2012. JAMA Internal Medicine 176(11): 1639-1648.
- Hecker MT, Aron DC, Patel NP, Lehmann MK, Donskey CJ (2003) Unnecessary use of antimicrobials in hospitalized patients: Current patterns of misuse with an emphasis on the antianaerobic spectrum of activity. Archives of Internal Medicine 163(8): 972-978.
- Carling P, Fung T, Killion A, Terrin N, Barza M (2003) Favorable impact of a multidisciplinary antibiotic management program conducted during 7 years. Infection Control & Hospital Epidemiology 24(9): 699-706.
- Kaki R, Elligsen M, Walker S, Simor A, Palmay L, et al. (2011) Impact of antimicrobial stewardship in critical care: A systematic review. Journal of Antimicrobial Chemotherapy 66(6): 1223-1230.
- Huebner C, Flessa S, Huebner NO (2019) The economic impact of antimicrobial stewardship programmes in hospitals: A systematic literature review. Journal of Hospital Infection 102(4): 369-376.
- Schuts EC, Hulscher ME, Mouton JW, Verduin CM, Stuart JW, et al. (2016) Current evidence on hospital antimicrobial stewardship objectives: A systematic review and meta-analysis. The Lancet Infectious Diseases 16(7): 847-856.
- Hwang H, Kim B (2018) Impact of an infectious diseases specialist-led antimicrobial stewardship programmes on antibiotic use and antimicrobial resistance in a large Korean hospital. Scientific Reports 8(1): 14757.
- Core elements of hospital antimicrobial stewardship programs, US Department of Health and Human Services, CDC, Georgia, USA.
- Joint Commission (2016) Prepublication requirements. New antimicrobial stewardship standard. Joint Comm Perspect. 2016 Jun 22.
- Centers for Medicare and Medicaid Services (2016) Medicare and Medicaid programs; hospital and Critical Access Hospital (CAH) changes to promote innovation, flexibility, and improvement in patient care. Federal Register 81: 116.
- Olans RN, Olans RD, DeMaria Jr A (2016) The critical role of the staff nurse in antimicrobial stewardship-unrecognized, but already there. Clinical Infectious Diseases 62(1): 84-89.
- Ladenheim D, Rosembert D, Hallam C, Micallef C (2013) Antimicrobial stewardship: The role of the nurse. Nursing Standard 28(6): 46.
- Castro-Sánchez E, Gilchrist M, Ahmad R, Courtenay M, Bosanquet J, et al. (2019) Nurse roles in antimicrobial stewardship: Lessons from public sectors models of acute care service delivery in the United Kingdom. Antimicrobial Resistance & Infection Control 8(1): 1-8.
- (2017) Centers for Disease Control and Prevention. Redefining the Antimicrobial Stewardship Team: Centers for Disease Control and Prevention Recommendations from the American RNs Association/Centers for Disease Control and Prevention Workgroup on the Role of Registered RNs in Hospital Antimicrobial Stewardship Practices, American Nurses Association, Maryland, USA.
- Edwards R, Drumright LN, Kiernan M, Holmes A (2011) Covering more territory to fight resistance: Considering nurses’ role in antimicrobial stewardship. Journal of Infection Prevention 12(1): 6-10.
- Albarillo FS, Joyce CJ, Santarossa M (2020) The use of survey-driven feedback to improve antimicrobial stewardship efforts at a single center. Infection Control & Hospital Epidemiology 41(2): 252-253.
- Venugopalan V, Trustman N, Manning N, Hashem N, Berkowitz L, et al. (2016) Administration of a survey to evaluate the attitudes of house staff physicians towards antimicrobial resistance and the antimicrobial stewardship programme at a community teaching hospital. Journal of Global Antimicrobial Resistance 4: 21-27.
- Srinivasan A, Song X, Richards A, Sinkowitz-Cochran R, Cardo D, et al. (2004) A survey of knowledge, attitudes, and beliefs of house staff physicians from various specialties concerning antimicrobial use and resistance. Archives of Internal Medicine 164(13): 1451-1456.
- Rusic D, Bozic J, Bukic J, Vilovic M, Tomicic M, et al. (2021) Antimicrobial resistance: Physicians' and pharmacists' perspective. Microbial Drug Resistance 27(5): 670-677.
- Charani E, Castro-Sanchéz E, Bradley S, Nathwani D, Holmes AH, et al. (2019) Implementation of antibiotic stewardship in different settings-results of an international survey. Antimicrobial Resistance & Infection Control 8(1): 1-6.
- Charani E, Smith I, Skodvin B, Perozziello A, Lucet JC, et al. (2019) Investigating the cultural and contextual determinants of antimicrobial stewardship programmes across low-, middle-and high-income countries-A qualitative study. PloS one 14(1): e0209847.
- Benson S, Powers J (2011) Your role in infection prevention. Nursing Made Incredibly Easy 9(3): 36-41.
- Suliman M, Aloush S, Aljezawi M, AlBashtawy M (2018) Knowledge and practices of isolation precautions among nurses in Jordan. American Journal of Infection Control 46(6): 680-684.
- Salem OA (2019) Knowledge and practices of nurses in infection prevention and control within a tertiary care hospital. Annals of Medical and Health Sciences Research 9(1): 422-425.
- Alojaimy RS, Nakamura K, Al-Sobaihi S, Tashiro Y, Watanabe N, et al. (2021) Infection prevention and control standards and associated factors: Case study of the level of knowledge and practices among nurses in a Saudi Arabian hospital. Journal of Preventive Medicine and Hygiene 62(2): E501-E507.
- Richardson M, Hines S, Dixon G, Highe L, Brierley J (2010) Establishing nurse-led ventilator-associated pneumonia surveillance in paediatric intensive care. Journal of Hospital Infection 75(3): 220-224.
- Schiessler MM, Darwin LM, Phipps AR, Hegemann LR, Heybrock BS, et al. (2019) Don't have a doubt, get the catheter out: a nurse-driven CAUTI prevention protocol. Pediatric Quality & Safety 4(4): e183.
- Woods-Hill CZ, Papili K, Nelson E, Lipinski K, Shea J, et al. (2021) Harnessing implementation science to optimize harm prevention in critically ill children: A pilot study of bedside nurse CLABSI bundle performance in the pediatric intensive care unit. American Journal of Infection Control 49(3): 345-351.
- Mostaghim M, Snelling T, McMullan B, Konecny P, Bond S, et al. (2017) Nurses are underutilised in antimicrobial stewardship–results of a multisite survey in paediatric and adult hospitals. Infection Disease & Health 22(2): 57-64.
- Merrill K, Hanson SF, Sumner S, Vento T, Veillette J, et al. (2019) Antimicrobial stewardship: Staff nurse knowledge and attitudes. American Journal of Infection Control 47(10): 1219-1224.
- Padigos J, Ritchie S, Lim AG (2020) Enhancing RNs’ future role in antimicrobial stewardship. Collegian 27(5): 487-498.
- Perez R, Hayes JE, Winters AR, Wrenn RH, Moehring RW (2024) Antimicrobial stewardship Knowledge, Attitudes, and Practices (KAP) among nurses. Antimicrobial Stewardship & Healthcare Epidemiology 4(1): e51.
- Zhao W, Xu Y, Liu R, Zhao T, Ning Y, et al. (2023) Knowledge, attitudes, and practices of bedside nurses regarding antimicrobial stewardship in China: An explanatory sequential mixed methods study. Journal of Nursing Management 2023(1): 9059920
- Abera B, Kibret M, Mulu W (2014) Knowledge and beliefs on antimicrobial resistance among physicians and nurses in hospitals in Amhara region, Ethiopia. BMC Pharmacology and Toxicology 15: 26.
- Ren-Zhang L, Chee-Lan L, Hui-Yin Y (2020) The awareness and perception on antimicrobial stewardship among healthcare professionals in a tertiary teaching hospital Malaysia. Archives of Pharmacy Practice 11(2).
- Monsees E, Popejoy L, Jackson MA, Lee B, Goldman J (2018) Integrating staff nurses in antibiotic stewardship: Opportunities and barriers. American Journal of Infection Control 46(7): 737-742.
- Fisher CC, Cox VC, Gorman SK, Lesko N, Holdsworth K, et al. (2018) A theory-informed assessment of the barriers and facilitators to nurse-driven antimicrobial stewardship. American Journal of Infection Control 46(12): 1365-1369.
- Gillespie E, Rodrigues A, Wright L, Williams N, Stuart RL (2013) Improving antibiotic stewardship by involving nurses. American Journal of Infection Control 41(4): 365-367.
- Pritts KE, Hiller LG (2014) Implementation of physician and nurse patient rounding on a 42-bed medical unit. MedSurg Nursing. 23(6): 408.
- Henkin S, Chon TY, Christopherson ML, Halvorsen AJ, Worden LM, et al. (2016) Improving nurse-physician teamwork through interprofessional bedside rounding. Journal of Multidisciplinary Healthcare 9: 201-205.
- Gormley DK, Costanzo AJ, Goetz J, Israel J, Hill-Clark J, et al. (2019) Impact of nurse-led interprofessional rounding on patient experience. Nursing Clinics 54(1): 115-126.
© 2024 Fritzie S Albarillo. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






