- Submissions

Full Text
Advancements in Case Studies
Redefining Developmental Potential in Senior Adults with Autism and Intellectual Disability: A Case Study of the CHIPPS Program
Jean Louis Adrien1*, Célia Nézereau1,2, Marie Davia Wardi2, Marion Wolff3, Maria Pilar Gattegno1,4 and Romuald Blanc1,5
1University Paris City, Laboratory of Psychopathology and Health Processes, F-92100 Boulogne Billancourt, France
2Office of Psychology ESPAS-Sup, 97, Avenue Charles de Gaulle, 92200 Neuilly sur Seine, France
3Espace-Tests PEPSS (Platform for Evaluation, Prototyping and Usage Tests), ESTIA-TECH, 97, Allée Théodore Monod-Technopole Izarbel-64 210 BIDART, France
4Office of Psychology ESPAS-Sup, 12, Avenue on May 8 1945, 33110 Bordeaux-Le Bouscat, France
5Université de Tours, INSERM, Imaging Brain & Neuropsychiatry iBraiN U1253, 37032, Tours, France
*Corresponding author:Jean Louis Adrien, Laboratory of Psychopathology and Health Processes (UR4057), Institute of Psychology, University Paris City, France
Submission:July 08, 2025;Published: September 23, 2025

ISSN 2639-0531Volume4 Issue4
Abstract
This brief report presents a powerful case study that challenges prevailing assumptions about stagnation in older adults with Autism Spectrum Disorder (ASD) and severe Intellectual Disability (ID). Drawing on two complementary reports centered on the same 69-year-old woman, it highlights her remarkable progress and significant gains in personal autonomy assessed with Vineland Adaptive Behavior Scales-II (VABS-II), and in cognitive, and socio-emotional domains assessed with Socio-emotional and Cognitive Evaluation Battery for Adults (SCEB-A) made through a two-year individualized intervention using the CHIPPS program. Even though the results are from a single participant, these findings challenge the longstanding assumption that developmental progress is limited or impossible in older adults with severe neurodevelopmental disorders.
Keywords:Senior woman with ASD and severe intellectual disability; Evolution of personal autonomy and cognitive and socio-emotional abilities; Socio-emotional and Cognitive Evaluation Battery for Adults (SCEB-A); Personalised support with CHIPPS program
Introduction
Historically, the developmental potential of adults with Autism Spectrum Disorders (ASD) and severe Intellectual Disability (ID) has been underestimated, and thus this clinical population might be considered as «neglected». In fact, most interventions and research have focused on children [1], leaving a gap in understanding the plasticity and responsiveness of older individuals. Some relative to adults with ASD and ID focused on adaptive abilities generally concerned adults with normal intelligence or mild intellectual disability [2]. More recently, Fusar-Poli et al. (2017) carried out a pilot prospective study on socio-adaptive longterm outcome during 10 years of a cohort of 22 adults with moderate ID (age range: 16- 41 years). These adults lived in a farm-community and benefited from a TEACCH-oriented rehabilitation program. Focused on adaptive behavior development assessed with Vineland Scales [3], the authors show that raw scores remained stable and that standard scores improved over time, attesting the existence of increasing and no deterioration in this group.
Regarding adult with ASD and severe ID, emerging evidence suggests that with structured, individualized, and sustained support, meaningful progress is possible-even in late adulthood [4-6]. This paper presents the synthesis of both published case reports relative to a 69-year-old woman [5,6]. She benefited from the CHIPPS program (Coaching in Human and Intellectual Potential through Personalized Support) developed by Gattegno [7,8], designed to offer tailored psychoeducational interventions that integrate cognitive remediation, emotional development, and autonomy coaching. The aim is to highlight the potential for growth and learning in adults with severe neurodevelopmental disorders, such as autism and profound intellectual disability.
Participant profile and clinical background
The participant of both case reports is a 69-year-old woman with a complex clinical history, diagnosed with “psychotic disorders, schizophrenic reactionsˮ at the age of 13, later reclassified as severe ASD and ID [9]. She presented with epilepsy of unknown etiology at 66 years of age. Residing in a Specialized Reception Home (SRH) for adults with severe handicaps, she received 15 hours/ week of individualized support over 24 months by a psychologist supervised (third author) by an expert psychologist (second author) specialized in the CHIPPS program [10]. This profile reflects a population often excluded from developmental research due to the severity of impairments and age-related biases.
Vineland Adaptive Behavior Scales-II (VABS-II)
The Vineland Adaptive Behavior Scales-II [11] was used to assess only personal autonomy in self-care domains (eating, dressing, hygiene). The VABS-II is a gold-standard tool for measuring adaptive behavior in individuals with developmental disabilities [12]. It was used in a recent study implying adults with ASD and severe ID [13].
Observation Grid for Autonomous Skills (OGAS)
The Observation Grid for Autonomous Skills (OGAS), a behavioral tracking tool was developed to monitor daily routines and the level of assistance required [6].
Social Cognitive Evaluation Battery for Adults (SCEB-A)
This tool evaluates 7 cognitive and 9 socio-emotional domains, including object permanence, spatial relations, joint attention, and receptive language. Each domain comprised items hierarchized in developmental levels from 1 to 4 corresponding to period of age 4-24 months [14]. Level 0 was indicated when no behavior from level 1 was noted. It has been recently adapted for adults with ASD and severe ID [15]. Achieved (item’ behavior was succeeded by adult with help and demonstration) and consolidated levels (items ‘behavior was succeeded by adult without help and demonstration) scores were calculated at the beginning (Time 1) and the end (Time 2) of the CHIPPS program and were compared to show evidence of eventual progress.
Data analysis
To assess the adult progress in all evaluated domains, a Single Case Research (SCR) procedure [16,17] was implemented for the analysis of individual effects; this procedure is particularly suitable for small-sample studies. The principle is based on the measurement of “Nonoverlapping data” collected in two distinct phases-Time 1 Level and Time 2 Level-which were combined to give the trend for the latter.
Result
Personal autonomy
Figure 1:Raw scores (from 0 to 20) in «Eating and Drinking» and «Dressing» categories in VABS-II obtained by the senior with ASD and severe ID at Times 1 and 2 (duration=24 months), and category’ maximum score (=20).

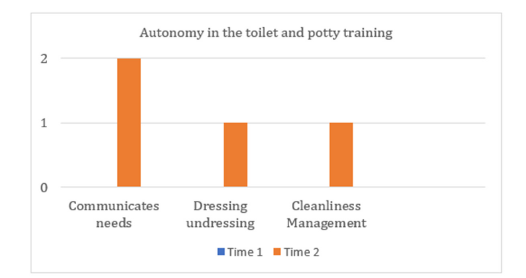
Developmental age in self-care assessed with VABS-II increased from 13 to 27 months. There were differences and variations in both initial acquisitions and progresses made by the adult according to categories of self-care. For example, in «Eating and Drinking», the initial acquisition was better than in dressing (no acquisition) meaning that the carrying out of actions during the meal by the adult senior was better than during the dressing, However, the increasing in these two domains was almost equal, respectively 4 and 3 points (Figure 1). Assessment of behaviors with OGAS show evidence of marked increase, for example in Autonomy in the toilet and potty training» (Figure 2). Comparative statistical analysis indicated an effect size: Nonoverlap of All Pairs (NAP) reached 100% in some domains, indicating a strong intervention effect.
Figure 2:Scores (0, 1 or 2) of the behaviors exhibited by the senior with ASD and severe ID in Communication Needs, dressing undressing and Cleanliness Management assessed with the Observation Grid for Autonomous Scale (OGAS) at Times 1 and 2 (Interval duration=24 months).
Cognitive development
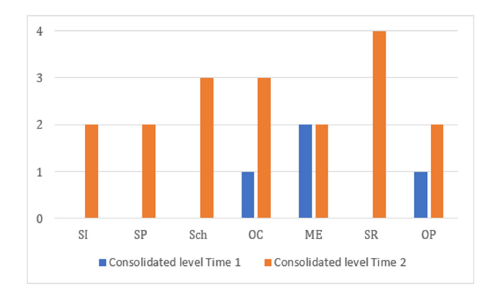
In cognitive area, gains were observed in 6 out of 7 cognitive domains attested by increasing of consolidated levels scores. The most significant improvements were noted in Spatial Relations (+4 consolidated levels) and Object Schemata (+3 consolidated levels) (Figure 3). Comparative analysis show evidence of a statistical significance: Nonoverlap of All Pairs (NAP=96%, p=0.004).
Figure 3:Profiles of consolidated development levels at Times 1 and 2 for the cognitive domains: Self-Image (SI), Symbolic Play (SP), Object Relation schemata (Sch), Operational Causality (OC), Means-End (ME), Spatial Relations (SR), and Object Permanence (OP).
Socio-emotional development
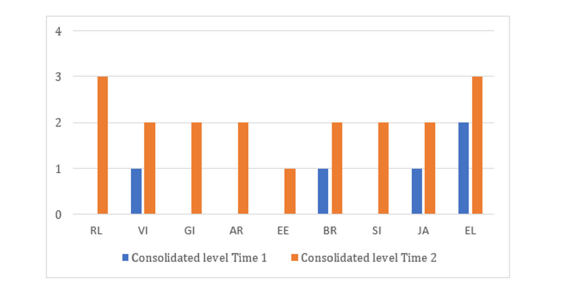
In socio-emotional area, all 9 domains showed improvement, attested by increasing of consolidated levels scores. There was a notable gain in receptive language (+3 levels) (Figure 4). Comparative analysis show evidence of a statistical significance: Nonoverlap of All Pairs, NAP=93%, p=0.012.
Figure 4:Profiles of consolidated development levels at Times 1 and 2 for the socio-emotional domains: Receptive Language (RL), Vocal Imitation (VI), Gestural Imitation (GI), Affective Relation (AR), Emotional Expression (E), Behaviour Regulation (BR), Social Interaction (SI), Joint Attention (JA), Expressive Language (EL). Increase was particularly noted in Receptive Language (RL).
Discussion
These findings provide compelling evidence that developmental plasticity persists into late adulthood, even in individuals with severe neurodevelopmental conditions. The CHIPPS program’s structured, individualized approach appears to activate latent abilities that are often overlooked in traditional care models. So, the main learnings made by the senior were concerned with the visuospatial coordination using of objects and the receptive language abilities, that were essential for greater autonomy in daily life. And this one was noted in several domains such as eating, drinking, dressing and in the toilet and potty training. This challenges the prevailing notion of “developmental stagnation” in older adults with ASD and ID, aligning with recent calls for lifespan-oriented interventions [4-6]. Moreover, the use of tools like the SCEB-A [5] and VABS-II [18,19] allows for nuanced tracking of progress, reinforcing the importance of standardized, developmentally sensitive assessments.
Conclusion
The dual case study illustrates that meaningful developmental gains are achievable in elderly individuals with ASD and severe ID when provided with consistent, personalized support. Even though these results relative to only one patient cannot be generalized, they advocate for a paradigm shift in how we approach aging and disability, emphasizing the need for long-term, individualized interventions that respect the potential for growth at any age. Moreover, in order to validate the effectiveness of the CHIPPS program for this clinical population, results from several patients will need to be presented and compared with the findings from this individual case.
Acknowledgement
We thank the patient, a senior female adult with autism and severe intellectual disability and her sister. Moreover, we thank all the members of her medico-social service team who have a convention partnership with Université Paris Cité. We thank the Foundation Perce-Neige for its logistic and financial support.
Funding
Funds from Foundation Perce-Neige (Number H03R4057-P5 Psycho-EA4057-LPPS and from Faculty “Societies and Humanities” of the Université Paris Cité (Budget Restreint, Impact Optimal » ATRIUM S&H).
Conflict of interest
The authors declare that the submitted work was carried out in the absence of any personal, professional or financial relationships and so, does not have any conflict of interest.
References
- Edwards TL, Watkins EE, Lotfizadeh AD, Poling A (2012) Intervention research to benefit people with autism: How old are the participants? Research in Autism Spectrum Disorders 6(3): 996-999.
- Levy A, Perry A (2011) Outcomes in adolescents and adults with autism: A review of the literature. Research in Autism Spectrum Disorders 5(4): 1271-1282.
- Sparrow SS, Balla DA, Cicchetti DV, Harrison PL, Doll EA, et al. (1984) Vineland adaptive behavior scales. American Guidance Service, Circle Pines, Minnesota, USA.
- Sappok T, Diefenbacher A, Gaul I, Bölte S (2013) Emotional development in adults with autism and intellectual disabilities: A retrospective analysis using the SAED. Research in Developmental Disabilities 34(3): 807-813.
- Adrien JL, Nézereau C, Wolff M, Wardi MD, Gattegno MP, et al. (2025) Evolution of cognitive and socio-emotional skills in an older woman with autism spectrum disorders and severe intellectual disability receiving individualized support based on the CHIPPS program: A clinical case report. Journal of Clinical Case Reports and Studies 6(4).
- Nézereau C, Wardi MD, Wolff M, Gattegno MP, Blanc R, et al. (2025) Evolution of personal autonomy behaviours in an elderly woman with autism spectrum disorder and severe intellectual disability receiving individualised support based on the CHIPPS program: A clinical case report. International Journal of Developmental Disabilities pp. 1-9.
- Gattegno MP (2004) Academic and professional support for people with autism, School and professional coaching of people with autism. Approach Neuropsychological of the Learning chez the Child (ANAE) 74-75: 36-38.
- Gattegno MP (2011) The IDDEES Program (CHIPPS Program). In: Adrien JL, Gattegno MP (Eds.), Childhood Autism: Assessments, Interventions and Follow-Up, Mardaga Brussels, Belgium, pp. 167-179.
- American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders: DSM-5. (5th edn), American Psychiatric Association, Washington DC, USA.
- Nézereau C (2017) Study of the cognitive and socio-adaptive developmental trajectories of children and adults with ASD benefiting from the CHIPPS program, including new school learning and communication technologies. Dissertation PhD thesis, Université Paris Descartes, France.
- Sparrow SS, Cicchetti DV, Balla DA (2005) Vineland adaptive behavior scales (Vineland-II). (2nd edn), Pearson Assessments, Oregon, USA.
- Zaghzi C, Moine V, Albuisson E, Kabuth B (2022) The Vineland-II in autism intervention research: A literature review. Child and Adolescent Neuropsychiatry. 7(70): 345-351.
- Adrien JL, Blanc R, Thiébaut É, (2025a) Profile and development of adaptive behavior in adults with autism spectrum disorder and severe intellectual disability. Frontiers in Psychiatry 8:15 1470466.
- Thiébaut É, Paulais MA, Blanc R, Gattegno MP, Adrien JL (2022) Developmental Sensitivity of the Social Cognitive Evaluation Battery (SCEB) for infants and toddlers with typical development. French Psychology. 67(1): 61-76.
- Adrien JL, Thiébaut É, Blanc R (2025) Preliminary psychometric study of Socio-Emotional and Cognitive Evaluations Battery for Adults (SCEB-A) with autism spectrum disorders and severe intellectual disability. Global Journal of Intellectual and Developmental Disabilities 14(3): 1-10.
- Parker RI, Vannest KJ, Davis JL, Sauber SB (2011). Combining nonoverlap and trend for single-case research: Tau-U. Behavior Ther 42(2): 284-299.
- Wolff M, Nézereau C, Gattegno MP, Bernard Paulais MA, Adrien JL (2020) Contribution of Bayesian inference and single case research for validating the effects of support programs intended for children with Autism Spectrum Disorder (ASD). Psychology Research and Applications 2(3): 29-51.
- Chatham CH, Taylor KI, Charman T, Eule E, Fedele A, et al. (2018) Adaptive behavior in autism: Minimal clinically-important differences on the vineland-II. Autism Res 11(2): 270-283.
- Lord C, Charman T, Havdahl A, Carbone P, Anagnostou E, et al. (2022) The lancet commission on the future of care and clinical research in autism. Lancet 399(10321): 271-334.
© 2025 Jean Louis Adrien. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 





.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






