- Submissions

Full Text
Advancements in Case Studies
Low Phospholipid Associated Cholelithiasis (LPAC) Syndrome: A Case Report
Ali Hannachi*, Mariem Boumediene and Mariem Jrad
Department of Radiology, Faculty of medicine of Tunis, Charles Nicolles Hospital, Tunisia
*Corresponding author:Ali Hannachi, Department of Radiology, Faculty of medicine of Tunis, Charles Nicolles Hospital, Tunisia
Submission:October 03, 2024;Published: November 11, 2024

ISSN 2639-0531Volume4 Issue3
Abstract
Low phospholipid associated cholelithiasis (LPAC) syndrome is a rare disease described for the first time in 2011 by Rosmorduc et al. [1] . It is one of the syndromes associated with ABCB4 gene mutation, which codes for the MDR3 protein, a biliary carrier. Characteristics of this syndrome include intrahepatic lithiasis, symptomatic cholesterol stones with early onset (<40 years), recurrent symptoms post cholecystectomy and symptom resolution with ursodeoxycholic acid (UDCA). We present a case of middle-aged female patient who presented with epigastric pain one year after cholecystectomy. The diagnosis of LPAC syndrome was suspected on clinical and radiological presentation. The patient was treated with ursodeoxycholic acid with a good outcome.
Keywords:LPAC syndrome; Low phospholipid associated cholelithiasis; Intrahepatic lithiasis; ABCB4/ MDR3 mutation
Introduction
Low Phospholipid-Associated Cholelithiasis (LPAC) syndrome is a rare genetic disorder characterized by the formation of gallstones due to a mutation in the ABCB4 gene, which encodes the multidrug resistance protein 3 (MDR3). This protein is crucial for the transport of phospholipids into bile, and its deficiency leads to impaired cholesterol solubilization, resulting in the precipitation of cholesterol and the formation of gallstones.
LPAC syndrome typically presents with biliary symptoms before the age of 40 and is often marked by the recurrence of symptoms even after cholecystectomy. Patients may experience intense intermittent abdominal pain, particularly in the hepatic region, due to the presence and migration of gallstones. Unlike common gallstones, those associated with LPAC are not primarily composed of cholesterol and do not necessitate the removal of the gallbladder [1].
The diagnosis of LPAC syndrome is based on clinical criteria, including the early onset of symptoms, recurrence post-cholecystectomy, and a family history of intrahepatic lithiasis. Genetic testing can confirm the presence of ABCB4 mutations. The management of LPAC syndrome involves the long-term administration of ursodeoxycholic acid to prevent the formation of new stones and alleviate symptoms.
This case report aims to highlight the clinical presentation, diagnostic challenges, and management strategies of LPAC syndrome through the detailed examination of a patient case.
Case Report
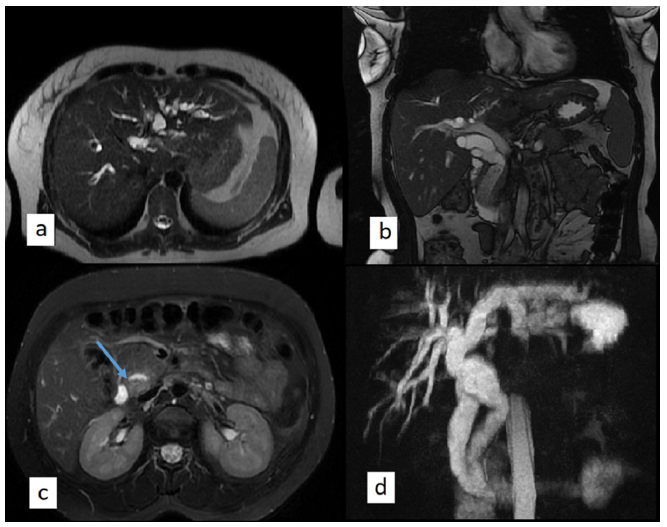
A 39-year-old woman with a past history of cholecystectomy presented to our institution with a 24-hour of epigastric and right upper quadrant abdominal pain, nausea and vomiting. The patient reported biliary colics for the last year. The clinical examination revealed a body-mass index of 25kg/m2, epigastric tenderness on palpation with no fever or jaundice. Hepatic tests revealed acute hepatic cytolisis and icteric cholestasis. Ultrasonography was performed in first intention. It revealed a dilatation of intra and extra-hepatic bile ducts, multiple intrahepatic hyperechoic foci with posterior acoustic shadowing disseminated in both hepatic lobes corresponding to intrahepatic cholelithiasis and multiple choledocolithiasis. The patient underwent magnetic resonance cholangiopancreatography (MRCP), which showed diffuse dilatation of intrahepatic and extrahepatic biliary ducts with multiple biliary stones. The patient underwent an endoscopic sphincterotomy and was then treated with ursodeoxycholic acid (UDCA). She remained asymptomatic (Figures 1&2).
Figure 1:B-mode ultrasound imaging: (a) Dilatation of intrahepatic biliary ducts with hyperechoic intrahepatic calculi, (b) Comet-tail image with posterior acoustic shadowing in the right hepatic lobe (arrow).
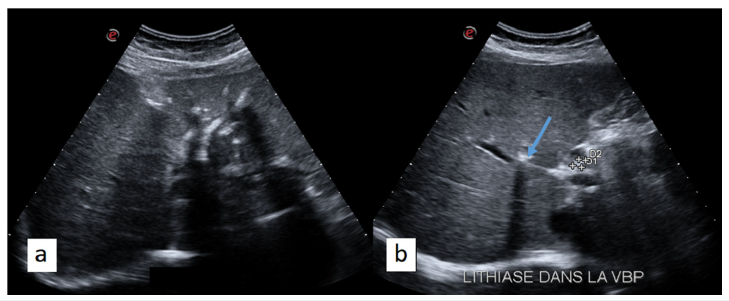
Figure 2:Axial T2 SSFSE (a), coronal T2 SSFSE and MIP reconstruction of a 3D bili-MR sequence (d) revealing intra and extra-hepatic biliary dilatation. Axial T2 FAT SAT (c) showing low signal content of the distal common bile duct which was revealed to be microlithiasis after endoscopic sphincterotomy.
Discussion
Low phospholipid associated cholelithiasis (LPAC) syndrome is one of the diseases associated with ABCB4/MDR3 mutation which include progressive familial intrahepatic cholestasis, intrahepatic cholestasis of pregnancy, transient neonatal cholestasis, primary sclerosing cholangitis, drug induced cholestasis and primary biliary cirrhosis [1]. ABCB4 gene encodes for multi-drug resistance protein 3 (MDR 3) a membrane-associated protein involved in the transportation of phosphatidylcholine into bile. Phosphatidylcholine is a carrier of cholesterol in the bile in association with biliary acids. A deficiency of MDR3 induces a decrease in the secretion of phosphatidylcholine and thus precipitation of cholesterol in bile ducts forming biliary lithiasis [2].
The diagnosis of LPAC syndrome should be suspected when
two of the four following criteria are present:
A. Age at the onset of symptoms less than 40 years.
B. Recurrence of symptoms after cholecystectomy
C. Presence of hyperechogenic intrahepatic foci detected by
ultrasound, sludge or intrahepatic microlithiasis
D. Symptoms resolution with ursodeoxycholic acid [3].
Minor diagnostic criteria include: A family history of biliary lithiasis and past history of gestational lithiasis.
The diagnosis is made based on clinical presentation, imaging criteria, the analysis of the bile collected after catheterization and genetic study.
The management of Low Phospholipid-Associated Cholelithiasis (LPAC) syndrome primarily involves the long-term administration of ursodeoxycholic acid (UDCA). UDCA works by reducing cholesterol saturation in bile, thereby preventing the formation of new gallstones and promoting the dissolution of existing ones. This treatment helps alleviate biliary symptoms and reduces the recurrence of gallstones, even in patients who have undergone cholecystectomy. In addition to UDCA, patients may benefit from regular monitoring through imaging studies to assess the presence of gallstones and liver function tests to ensure optimal management. Genetic counseling is also recommended for affected individuals and their families, given the hereditary nature of the syndrome. In cases where UDCA is insufficient, endoscopic or surgical interventions may be necessary to manage complications such as bile duct obstruction.
Conclusion
LPAC syndrome is associated with ABCB4/MDR3 gene mutation. It should be suspected in a patient presenting with recurrent biliary lithiasis at an age less than 40 years. Radiologists should be alerted because the early diagnosis tranform the outcome of this disease. The treatment is based on ursodeoxycholic acid (UDCA).
Patient Consent Statement
The patient has provided written consent with regards to publication of her case.
Declaration of Interest
The authors have no conflicts of interest to declare.
Funding Sources
No subsidies or grants contributed to this work.
References
- Poupon R, Rosmorduc O, Boëlle PY, Chrétien Y, Corpechot C, et al. (2013) Genotype-phenotype relationships in the low-phospholipid-associated cholelithiasis syndrome: A study of 156 consecutive patients. Hepatology 58(3): 1105-1110.
- Erlinger S (2012) Low phospholipid-associated cholestasis and cholelithiasis. Clinics and Research in Hepatology and Gastroenterology 36: S36-40.
- Rosmorduc O, Poupon R (2007) Low phospholipid associated cholelithiasis: association with mutation in the MDR3/ABCB4 gene. Orphanet J Rare Dis 2: 29.
© 2024 Ali Hannachi. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 





.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






