- Submissions

Full Text
Advances in Complementary & Alternative medicine
Non-Pharmacological Intervention Modulates Self-Referential Brain Function: A Contemplative Approach
Dwivedi Krishna*
Department of Yoga and Life Sciences, Swami Vivekananda Yoga Anusandhana Samsthana (S-VYASA), India
*Corresponding author:Dwivedi Krishna, Assistant Professor, Cognitive Neuroscience Laboratory, Department of Yoga and Life Sciences, Swami Vivekananda Yoga Anusandhana Samsthana (S-VYASA), Bengaluru, India
Submission: August 18, 2025;Published: September 12, 2025

ISSN: 2637-7802 Volume 8 Issue 5
Abstract
Non-pharmacological therapies play a crucial role in managing non-communicable diseases, providing alternatives to conventional medical treatments. Non-pharmacological therapies include Yoga, which combines physical postures, breath control and meditation to promote both physical and mental wellbeing. However, the neurocognitive mechanisms underlying the therapeutic effects of yoga, particularly its influence on Self-Referential Processing (SRP), remain poorly understood. SRP is fundamental for self-awareness, emotional regulation and decision-making, with key brain regions including the medial prefrontal cortex, posterior cingulate cortex and precuneus. Yoga practice has been linked to structural changes in these areas, including enhanced gray matter volume and improved connectivity within the Default Mode Network (DMN), both of which are important for SRP. These neuroplastic effects, including increased cortical thickness and neurogenesis, suggest that yoga fosters cognitive flexibility and emotional resilience. Functional neuroimaging studies show altered DMN connectivity in yoga practitioners, indicating improved modulation of self-referential thoughts and reduced rumination, which is commonly seen in mood disorders. However, direct research on yoga’s impact on SRP through neuroimaging is limited. This study aims to investigate the neural mechanisms through which Yoga practice influences SRP, potentially offering insights for therapeutic interventions targeting cognitive distortions related to mental health conditions. We also highlight peripheral biomarkers that warrant investigation to link contemplative practices with neuroprotective mechanisms and to inform future translational studies.
Keywords:Yoga; Self-referential processing; Neurocognitive mechanisms; Default mode network; Emotional regulation
Introduction
Non-pharmacological therapies, such as yoga, have gained widespread recognition for their multifaceted benefits on physical, mental and emotional well-being. Yoga, an ancient practice originating from India, initially served as a spiritual and philosophical discipline but has evolved into a modern therapeutic modality that integrates āsanas (physical postures), prāṇāyāma (breathing Practices) and dhyāna (meditation). Extensive research over the past few decades has elucidated the positive effects of yoga on various psychological conditions, including depression, anxiety and stress [1,2]. Yoga promotes a state of mind-body integration, enhancing mindfulness and self-regulation, which may contribute to its therapeutic efficacy. Although the benefits of yoga are widely accepted, the neurocognitive mechanisms underlying these effects remain an area of growing interest, particularly its influence on SRP. Selfreferential processing is central to the cognitive framework that allows individuals to engage with self-relevant stimuli. It plays a crucial role in memory retrieval, emotional regulation and decision-making [3]. The capacity to process information from a self-relevant perspective is essential for maintaining a coherent self-concept and navigating complex social and emotional experiences. Neuroimaging research has identified several brain regions critical for SRP, including the Medial Pre Frontal Cortex (mPFC), Posterior Cingulate Cortex (PCC), and the precuneus [4]. These structures are integral components of the DMN, a set of interconnected brain areas that exhibit heightened activity during introspective and self-referential tasks [5]. Disruptions in DMN activity and SRP have been implicated in a variety of psychiatric disorders, particularly mood disorders, such as depression and anxiety, where individuals demonstrate heightened self-focus and negative self-evaluation [6].
Recent studies have indicated that yoga practice may induce structural and functional alterations in brain regions associated with SRP, suggesting a potential therapeutic avenue for enhancing self-regulation and alleviating symptoms of psychological distress [7]. Yoga practitioners have been shown to exhibit increased gray matter volume in areas such as the mPFC and PCC [8]. These structural changes may facilitate improved cognitive functions related to self-awareness, emotional regulation and introspection. Furthermore, Functional Magnetic Resonance Imaging (fMRI) studies have revealed that yoga practitioners demonstrate altered connectivity within the DMN, with increased functional coupling between the DMN and executive control networks [9]. This altered connectivity pattern may indicate a more efficient modulation of self-referential thought processes, potentially reducing maladaptive cognitive patterns such as rumination. By uniting physical postures, conscious breathing, and mindful awareness, yoga engages the brain through both top-down and bottom-up neural mechanisms. Prāṇāyāma has been linked to modulation of the autonomic nervous system, reducing sympathetic activation and enhancing parasympathetic activity, which in turn impacts brain regions involved in emotional regulation [10]. Meditative practices further activate prefrontal regions that are responsible for monitoring and managing self-related thoughts. This dual influence of bodily awareness and cognitive control offers a comprehensive framework through which yoga may influence SRP and related neural circuits. Through consistent practice, individuals may develop an enhanced capacity for self-reflection and emotion regulation, which could be beneficial in managing conditions characterized by dysfunctional SRP, such as depression and anxiety.
Despite the growing body of evidence supporting the neurocognitive benefits of yoga, research specifically addressing its influence on SRP is limited. Most studies have primarily focused on general cognitive improvements or emotional regulation, without isolating SRP as a distinct cognitive function. Furthermore, while neuroimaging studies have demonstrated structural and functional changes in brain regions involved in self-referential thought, few have directly linked these changes to yoga practice. There is also a significant gap in understanding the differential effects of various components of yoga, such as āsanas, prāṇāyāma, and dhyāna on self-related cognitive functions. Moreover, longitudinal studies investigating yoga practice and its neurocognitive impact remain sparse, with most research limited to short-term interventions or cross-sectional designs. Thus, a detailed exploration of the impact of yoga on SRP, particularly in long-term practitioners, is needed to better understand the mechanisms through which yoga may modulate self-related cognitive functions and improve mental wellbeing.
The rationale for this study stems from the need to fill the gaps in current research by investigating the neurocognitive effects of yoga practice on SRP. This study aims to provide empirical evidence on how sustained yoga practice modulates neural activity and structural changes in regions involved in SRP, including the mPFC, PCC, and precuneus. Using a combination of neuroimaging techniques and behavioral assessments, the study explored the specific neural mechanisms underlying the effects of yoga on selfreferential processing. This research is crucial for understanding how yoga may function as a therapeutic tool for mental health conditions that involve dysfunctional SRP, such as depression and anxiety. By exploring the neurocognitive pathways through which yoga influences SRP, the study will also provide valuable insights into the broader effects of contemplative practices on cognition and emotional regulation.
Through this investigation, we aim to contribute to the growing field of contemplative neuroscience by offering a deeper understanding of the neural mechanisms through which yoga influences self-referential processing. Ultimately, this research may further our understanding of the neurocognitive effects of yoga practice and inform clinical applications aimed at treating self-related cognitive distortions and enhancing psychological well-being. This study may not only advance scientific knowledge in the field of yoga neuroscience but also inform the development of more targeted and effective interventions for mental health disorders that are rooted in negative self-perceptions and selffocused rumination. As yoga continues to gain global popularity, understanding its neurocognitive effects becomes increasingly relevant for both clinical and therapeutic purposes. By focusing specifically on the neurocognitive influence of yoga practice on SRP, this study aims to contribute valuable insights to the fields of neuroscience and psychology, offering new perspectives on how mind-body practices can optimize mental health interventions and promote emotional resilience across diverse populations. An important complementary line of inquiry is the assessment of peripheral biomarkers that may reflect the systemic and neuroprotective effects of contemplative practices. Emerging work suggests lifestyle and mind-body interventions can modulate neurotrophic, metabolic, and inflammatory markers, measures including Brain-Derived Neurotrophic Factor (BDNF), cortisol, inflammatory cytokines (e.g., IL-6, CRP), and Sirtuin-1 (SIRT1), a NAD⁺-dependent deacetylase implicated in cellular stress resistance and neuroprotection. Including biomarker assessments alongside neuroimaging would help link peripheral physiology with central changes in self-referential networks and offer translational endpoints for studies targeting brain aging and neurodegeneration.
Neurocognitive Effects of Yoga Practice
Structural brain changes
Structural brain changes induced by yoga practice are critical to understanding its impact on SRP. Research indicates that yoga practitioners show increased gray matter volume in areas associated with SRP, including the mPFC and PCC. These brain regions are crucial for self-reflection, autobiographical memory and emotional regulation [11], all of which are fundamental components of SRP. Gray matter is composed of neuronal cell bodies and is involved in processing and transmitting information. Increases in gray matter volume suggest that yoga can stimulate neuroplasticity [12], which may enhance cognitive functions related to self-awareness and emotional regulation. This neuroplasticity is likely a result of regular yoga practice, which enhances mindfulness, attention control and introspection, cognitive processes known to stimulate the capacity of the brain for adaptation and reorganization [13]. Increased gray matter volume in the mPFC and PCC, areas heavily involved in SRP, suggests that yoga practice may enhance the ability to process self-relevant information more effectively [14]. The influence of Yoga on brain structure may also be due to the practice’s ability to increase neurogenesis, the process through which new neurons are generated. Neurogenesis has been shown to be particularly active in regions like the hippocampus and the mPFC, which are involved in emotional regulation and memory processing [15].
Yoga is an integration of physical movement and mindful awareness that may stimulate neurogenesis by promoting BDNF, a protein that supports neuron growth and survival [16]. Enhanced neurogenesis in the mPFC and PCC may therefore contribute to improved self-regulation and more adaptive SRP. Moreover, the practice of yoga is associated with increased cortical thickness in areas involved in self-regulation [17]. Cortical thickness is an important indicator of brain health and cognitive functioning. Thicker cortices in the mPFC and PCC suggest that yoga practitioners may have enhanced cognitive resources for managing self-referential thoughts [18]. This increase in cortical thickness is thought to reflect the capacity of the brain to process and regulate self-related information more efficiently, leading to improved SRP.
Functional connectivity alterations
The ability to process self-referential information effectively relies heavily on the functional connectivity of the brain regions associated with self-reflection and emotion regulation. Yoga practice has been shown to alter the functional connectivity of brain regions involved in SRP, particularly those within the DMN [19]. The DMN, which includes the mPFC, PCC and precuneus, is responsible for internally directed cognition such as self-reflection and autobiographical memory retrieval. Studies using Functional Magnetic Resonance Imaging (fMRI) have demonstrated that yoga practitioners exhibit increased connectivity between regions of the DMN [19]. This enhanced connectivity is thought to contribute to improved self-regulation of self-referential thoughts. Specifically, yoga appears to enhance the coupling between the mPFC and PCC, which are key regions involved in managing emotional responses and processing self-relevant information [19]. Enhanced coupling within the DMN suggests that yoga practitioners may experience more efficient modulation of SRP, potentially reducing the intensity and frequency of negative self-focused thoughts, including rumination. Yoga also impacts the inter-network connectivity between the DMN and executive control networks [20], which are responsible for higher-order cognitive functions such as cognitive flexibility and attention regulation. Increased connectivity between the DMN and these cognitive networks suggests that yoga practitioners may have better control over self-referential thought processes, allowing them to shift between self-reflection and external focus more effectively [21]. This enhanced connectivity between internally and externally directed networks likely contributes to better emotional regulation and cognitive flexibility, which are essential for adaptive SRP. Moreover, functional connectivity changes in yoga practitioners have been linked to reduced activity in maladaptive neural pathways associated with excessive selffocus. Research indicates that yoga can lead to decreased activation of regions associated with rumination and negative self-evaluation [22], helping individuals manage self-referential thoughts more effectively. By reducing the neural activity associated with negative self-referential processing, yoga may promote a healthier and more balanced self-concept.
Behavioral and cognitive outcomes
Neurocognitive benefits of Yoga extend to behavioral and cognitive outcomes, particularly those related to self-regulation and SRP. Yoga practitioners tend to show improvements in emotional regulation, cognitive flexibility and working memory, all of which are essential for adaptive SRP [23,24]. These cognitive enhancements are thought to arise from the integrated nature of yoga, which combines physical movement, breath control, and meditative awareness. Yoga practitioners demonstrate a greater capacity for self-reflection and improved self-compassion [25], which may contribute to more positive SRP. By fostering a balanced and accurate self-concept, yoga practitioners may experience better emotional regulation and a healthier relationship with their self-referential thoughts. Yoga has been linked to reduced rumination, a cognitive pattern characterized by repetitive negative thinking about oneself, which is often associated with depression and anxiety [26].
The integration of mindfulness practices in yoga also leads to increased cognitive flexibility, which enhances the ability to shift between different self-referential perspectives. This increased flexibility is crucial for adapting self-related thoughts, such as managing negative emotions or adjusting self-evaluations in light of new information. As a result, yoga may help practitioners adopt more adaptive and constructive patterns of SRP, which are associated with better mental health outcomes [27]. Moreover, yoga’s focus on breath control and meditation promotes a state of mindfulness that enhances attention regulation and emotional awareness. By focusing attention on the present moment and observing self-referential thoughts non-judgmentally, yoga practitioners may experience a greater sense of psychological equanimity. This enhanced mindful awareness helps reduce the tendency to over-identify with negative self-referential thoughts, fostering a more balanced and objective self-concept.
Mindfulness and emotional regulation
Yoga practice has shown significant benefits in enhancing emotional regulation, which refers to the ability to manage and respond to emotional experiences in a balanced and adaptive manner [22]. The core components of yoga, mindfulness, breathing exercises (pranayama) and physical postures, have been linked to both neuroplastic changes in brain structures and functional improvements in emotional control. Research suggests that mindfulness meditation within yoga enhances self-awareness, enabling practitioners to observe and regulate their emotional responses [28]. This increased mindfulness leads to better attention control, which helps individuals reduce impulsivity and become more aware of their emotional states. Moreover, yoga practice has been shown to reduce rumination, a form of maladaptive emotional processing, by fostering an equanimous mindset that improves emotional resilience. This is particularly important for managing stress, anxiety and negative emotional responses. Yoga’s impact on emotion regulation is rooted in its ability to influence the autonomic nervous system, increasing parasympathetic activity and reducing the sympathetic nervous system’s response to stress [29].
This helps regulate heart rate, blood pressure and cortisol levels (a stress hormone), promoting a calm state. Brain imaging studies show that yoga increases gray matter in areas related to emotional control, such as the Pre Frontal Cortex (PFC), which plays a pivotal role in self-regulation and decision-making [8]. The hippocampus is involved in memory and emotional processing and has shown increased activity, suggesting that yoga can improve emotional memory processing and resilience to emotional stress [30]. Furthermore, the Anterior Cingulate Cortex (ACC), which helps in error detection and emotional regulation, shows enhanced connectivity, facilitating better emotional responses to conflicts and stress. The amygdala, the brain’s center for fear and threat detection, becomes less reactive, indicating that yoga helps reduce overactivation of this region, which is often associated with anxiety and stress [31]. Thus, yoga practice impacts a variety of brain regions that collectively contribute to enhanced emotional regulation, promoting adaptive responses to emotional challenges. The combination of structural and functional changes in these areas enables practitioners to better manage emotions, improve coping strategies, and increase overall emotional well-being.
Yoga and impulsivity
Impulsivity is generally considered a dimension of selfregulation, which is a broader psychological concept that encompasses both emotion regulation and cognitive control. From this standpoint, impulsivity is viewed as a failure of selfregulation, where individuals may act out of immediate emotional urges rather than using cognitive control to guide their actions more thoughtfully or adaptively. This psychological view suggests that individuals with high impulsivity often experience challenges with delayed gratification, self-restraint and goal-directed behavior [32]. Self-referential brain functions, which are responsible for selfawareness, self-reflection and emotional regulation, play a pivotal role in modulating impulsive behaviors. These functions involve brain regions such as the mPFC, the PCC and the DMN, all of which are involved in processing thoughts about the self, introspection and emotional responses. When the functioning of these areas is dysregulated, individuals can struggle with impulsive tendencies. Specifically, the PFC is responsible for higher-order cognitive functions, such as inhibition, decision-making and planning, functions essential for regulating emotions and controlling impulsive behavior [33].
Impairments or decreased activation in the PFC are frequently observed in individuals with high impulsivity, making it difficult for them to manage immediate emotional reactions or engage in cognitive control when faced with stressful situations or tempting cues. In contrast, when these brain regions function optimally, they enable individuals to engage in self-regulation, which helps them resist the urge to act impulsively. Psychologically, self-referential processing involves the capacity for self-awareness, which allows individuals to monitor their internal states and behavior and make decisions accordingly. Self-reflection enables people to evaluate their actions, identify maladaptive patterns and shift behavior when necessary. Self-referential processing can act as a double-edged sword. On one hand, it allows them to reflect on the consequences of their actions, fostering greater self-control. On the other hand, excessive self-criticism or rumination, an overactive form of self-referential processing, can exacerbate impulsivity [34]. This is because rumination often leads to emotional dysregulation, causing individuals to act impulsively as a way to manage negative emotional states. Thus, the balance between self-reflection and self-criticism is crucial in determining whether self-referential processing leads to adaptive emotional regulation or to heightened impulsivity [35].
Mindfulness practices have been shown to improve emotional regulation and impulse control by promoting a balanced and aware state of mind [36]. Yoga’s mindfulness-based techniques foster self-awareness by encouraging practitioners to focus on the present moment, observe their emotions without judgment and cultivate a non-reactive response to stress or emotional triggers. This practice strengthens the PFC by increasing cognitive flexibility and promoting the inhibition of impulsive urges [37]. Studies have demonstrated that yoga practitioners show increased gray matter volume in the PFC, which is linked to improved executive functions, including cognitive control and emotional regulation [14,38]. The combination of physical movement, breath control and mindfulness in yoga encourages the functional coordination between the PFC and other brain regions involved in emotion regulation, such as the amygdala and ACC. This improved neural coordination helps to reduce impulsivity by enhancing the brain’s ability to regulate emotional responses and prioritize long-term goals over immediate gratification [39].
Furthermore, yoga’s emphasis on prāṇāyāma regulates the autonomic nervous system, reducing physiological markers of stress such as heart rate and blood pressure. By enhancing parasympathetic nervous system activity, yoga helps practitioners maintain a calm, focused state, which mitigates the emotional reactivity associated with impulsive behaviors [40]. Through these neurobiological mechanisms, yoga provides a psychological framework for improving impulsivity and enhancing self-regulation. Impulsivity can be understood from a psychological perspective as a failure of self-regulation, which is influenced by both cognitive and emotional factors. Self-referential brain functions, including those involving the PFC, play a critical role in regulating impulsive behaviors. Mindfulness-based practices such as yoga can improve emotional regulation by enhancing self-awareness, cognitive flexibility and neural coordination between brain regions involved in self-regulation. Yoga thus represents a potent tool for reducing impulsivity and promoting adaptive, thoughtful behaviors.
Peripheral biomarkers and self-referential processing
Contemplative interventions such as yoga, meditation and related mind-body practices have increasingly been recognized for their potential to influence brain function through neuroplastic and neuroprotective pathways. In recent years, the study of peripheral biomarkers has gained attention as they provide a valuable lens into systemic mechanisms that may underpin cognitive and emotional benefits. Peripheral biomarkers, measurable in blood, saliva, or other body fluids, reflect processes such as neurotrophin activity, stress-axis regulation, inflammation and cellular aging. Their integration with neuroimaging and behavioral data could therefore elucidate the link between contemplative practices and cognitive functions. Among the most well-studied markers, BDNF plays a central role [41]. BDNF is vital for synaptic plasticity, memory consolidation, and mood regulation and importantly, it can cross the blood-brain barrier, allowing peripheral measures to act as a proxy for central effects. Several studies have reported that yoga and meditation retreats demonstrate elevated plasma BDNF alongside reductions in anxiety and depression and improvements in mindfulness [42].
These findings suggest that increased peripheral BDNF may parallel neural changes in brain networks involved in self-awareness and cognitive resilience, thereby linking contemplative practices to enhanced neuroplasticity. Cortisol, a primary stress hormone, is another important biomarker reflecting Hypothalamic-Pituitary- Adrenal (HPA) axis activity, which is associated with attention, memory and executive function. Dysregulated cortisol dynamics, such as blunted diurnal rhythms, are associated with cognitive decline and risky decision making [43]. Mind-body interventions have been shown to modulate cortisol levels, stabilizing stress reactivity [44]. Evidence indicates both reductions in basal cortisol and improvements in the cortisol awakening response following sustained yoga and meditation practices [42]. These changes may contribute to enhanced working memory, emotional regulation and resilience under stress, suggesting that cortisol is a sensitive marker of the stress-buffering effects of contemplative practices.
Inflammatory cytokines such as Interleukin-6 (IL-6), Tumor Necrosis Factor alpha (TNF-α) and CRP represent another important class of biomarkers linking systemic physiology with cognitive outcomes. Chronic inflammation accelerates brain aging, impairs synaptic function and increases vulnerability to neurodegenerative disorders. A growing body of evidence shows that yoga and meditation practices reduce circulating pro-inflammatory markers while enhancing anti-inflammatory pathways [45]. Numerous studies comparing yoga interventions with control conditions have observed decreases in IL-6 and CRP alongside improvements in depressive symptoms, indicating that anti-inflammatory effects may partly mediate the mental health benefits of yoga. By mitigating systemic inflammation, contemplative practices may protect against cognitive decline and improve higher-order executive functions. Beyond stress and inflammation, markers of cellular aging and mitochondrial resilience emerge as relevant endpoints. Among these, Sirtuin-1 (SIRT1) has attracted attention for its role in mitochondrial regulation, DNA repair and anti-aging processes [46].
Although direct evidence linking yoga to SIRT1 modulation remains preliminary, mechanistic parallels with exercise and calorie restriction suggest its potential relevance. SIRT1 promotes neuroprotection by enhancing stress resistance and metabolic homeostasis, and its upregulation could, in theory, mediate the neuroprotective benefits of contemplative practices. Additionally, yoga has been associated with improved mitochondrial function and reduced markers of cellular aging in chronic conditions such as rheumatoid arthritis, further supporting its role in systemic resilience [47]. Integrating SIRT1 and related mitochondrial biomarkers into contemplative neuroscience would open novel avenues for linking systemic longevity pathways with brain aging and cognitive health. Together, these biomarkers form a mechanistic bridge between contemplative practices and cognitive function. BDNF supports neuroplasticity required for learning and memory; stabilized cortisol dynamics and reduced inflammation enhance executive control and mood regulation; and SIRT1-related pathways contribute to cellular resilience against age-related cognitive decline [48]. By mapping biomarker trajectories alongside brain network changes, such as default mode network modulation, and behavioral outcomes, such as self-referential processing and working memory performance, researchers can delineate pathways from systemic physiology to neural plasticity and cognition.
A Possible Mechanism of Yoga on Self-Referential Processing (SRP)
Yoga practice exerts a profound influence on SRP through an integrated set of neuroplastic, functional, physiological and molecular mechanisms that reshape the brain’s architecture, optimize network connectivity, regulate bodily systems, and modulate peripheral biomarkers, collectively enhancing selfawareness, emotional regulation and cognitive flexibility illustrated in Figure 1. Structural neuroimaging studies consistently reveal increased gray matter volume in key SRP-related hubs such as the mPFC and PCC among experienced yoga practitioners, reflecting neuroplastic changes like dendritic branching, synaptogenesis, and glial proliferation induced by repeated engagement in mindful, introspective mental states during āsanas, prāṇāyāma, and dhyāna practices [8]. These structural adaptations fortify the neural substrates for nuanced self-reflection and emotional appraisal, reducing the likelihood of egocentric or negatively biased selffocus. Complementing these morphological changes, functional MRI investigations demonstrate that yoga enhances resting-state functional connectivity within the DMN, particularly between the mPFC and PCC and strengthens links between the DMN and executive control networks, suggesting that habitual attentional training through yoga fosters more cohesive communication among brain regions responsible for self-awareness, autobiographical memory and emotional regulation [49]. This optimized functional integration supports more adaptive modulation of self-referential thoughts, enabling practitioners to disengage from maladaptive cognitive loops such as rumination and negative self-evaluation while promoting balanced, constructive self-perception.
Figure 1:illustrates the potential benefits of yoga on SRP.
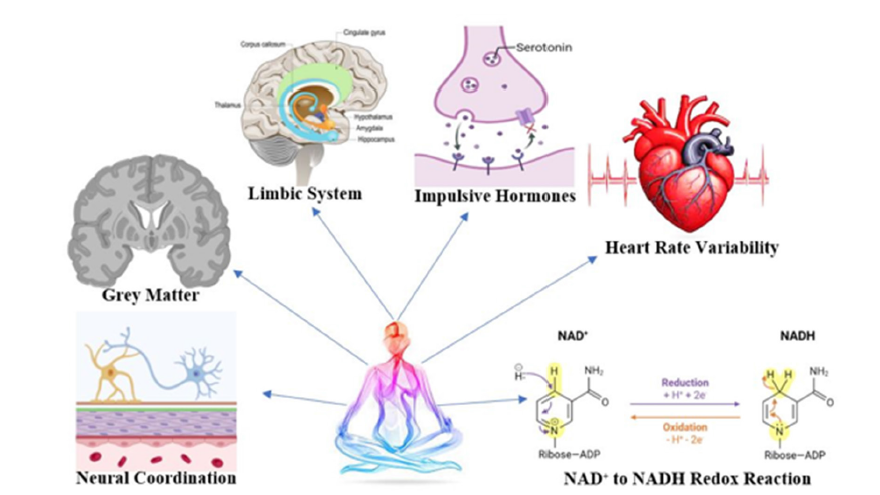
Beyond the central nervous system, yoga deeply influences the ANS, with pranayama and meditation practices eliciting parasympathetic dominance, lowering sympathetic arousal and increasing HRV, a marker of physiological resilience and flexibility [50,51]. These shifts are accompanied by reductions in cortisol and blood pressure, creating a calmer physiological baseline that buffers against stress-induced distortions of self-referential thought. In addition to these central and autonomic changes, yoga modulates peripheral biomarkers that provide systemic support for SRP-related brain functions. Elevated BDNF following yoga enhances synaptic plasticity and hippocampal-prefrontal connectivity, directly reinforcing the neural circuits underlying self-reflection, autobiographical memory, and emotional regulation [42]. Normalization of cortisol rhythms through regulation of the HPA axis reduces stress reactivity and stabilizes introspective processes, supporting balanced self-awareness. Reductions in inflammatory cytokines such as IL-6, TNF-α, and CRP protect neural tissue from inflammation-driven decline, thereby preserving the structural and functional integrity of SRP-related networks. Emerging evidence suggests that Sirtuin-1 (SIRT1), a NAD⁺-dependent deacetylase involved in mitochondrial function and neuroprotection, as a biomarker that may mediate long-term resilience of SRP during aging. These biomarker pathways converge with neural and autonomic adaptations to create a comprehensive psychophysiological platform for adaptive SRP.
The convergence of these neural, physiological, and molecular changes yields a powerful integrated mechanism: enhanced gray matter supports refined introspective processing, improved DMN connectivity fosters efficient self-monitoring and regulation, balanced autonomic activity underpins emotional stability, and biomarker modulation strengthens systemic resilience that sustains SRP across time. Behaviorally, these mechanisms manifest as heightened mindfulness, reduced reactivity to self-related emotional triggers, diminished negativity bias, and greater selfcompassion, outcomes consistently observed in psychological assessments of long-term yoga practitioners [8,49-51].
Mechanistically, yoga may be conceptualized as repeatedly engaging SRP, attentional control, autonomic regulation, and molecular pathways in a way that progressively strengthens their structural and functional integrity while recalibrating stress physiology and systemic biomarkers. Over time, this leads to a more resilient and adaptable self-referential system that can flexibly shift perspectives, integrate experiences nonjudgmentally, and respond adaptively to internal and external challenges. Moreover, the combination of yoga postures, controlled breathing, and meditative focus likely produces synergistic effects: āsana prepares the body and improves circulation, prāṇāyāma refines physiological and endocrine regulation, and dhyāna deepens attentional and emotional control, and biomarker modulation sustains neural and systemic resilience [52]. Together, these processes foster an optimal state for adaptive SRP. Overall, yoga acts as a multi-level intervention, simultaneously shaping brain structure, enhancing functional connectivity, recalibrating autonomic regulation, and modulating peripheral biomarkers to cultivate a stable yet flexible self-referential framework that supports mental clarity, emotional equanimity, resilience against stress and aging, and overall psychological flourishing.
Limitations of the Published Work
Although this study contributes to understanding the neurocognitive effects of yoga on SRP, several limitations should be acknowledged. A significant challenge in this field is the reliance on relatively small and heterogeneous samples. Yoga practitioners differ widely in terms of style, frequency, intensity and duration of practice, which introduces variability and limits the generalizability of findings. The lack of homogeneity across samples makes it difficult to draw firm conclusions about the specific neurocognitive effects of yoga, as observed changes may not represent the broader population of practitioners. Another limitation lies in the study design. Much of the existing research is cross-sectional, which restricts the ability to establish causal relationships between yoga practice and SRP-related brain changes. Without longitudinal or randomized controlled designs, it is difficult to determine whether structural and functional brain differences result directly from yoga or are linked to pre-existing cognitive or emotional traits. Furthermore, neuroimaging techniques such as fMRI, while powerful, measure activity indirectly through blood flow changes and may not fully capture the complexity of dynamic SRP processes. The absence of well-designed control groups in many studies presents another challenge. Without comparison to other physical, cognitive, or contemplative practices, it is unclear whether the effects observed are unique to yoga. Self-selection bias also remains a concern, as individuals drawn to yoga may already possess higher levels of mindfulness, emotional regulation, or stress resilience that influence outcomes. Finally, many studies lack integration of peripheral biomarkers such as BDNF, cortisol, inflammatory cytokines, and NAD⁺/Sirtuin pathways. These biomarkers are critical for understanding the systemic and mechanistic underpinnings of yoga’s impact on SRP but remain underexplored. In addition, reliance on self-reported practice frequency and intensity introduces recall and social desirability biases, highlighting the need for objective measures to strengthen future findings.
Implications of the Study
Despite certain methodological limitations, the implications of this study are far-reaching, particularly within contemplative neuroscience, clinical psychology and integrative medicine. By exploring how yoga influences SRP, this work sheds light not only on the neural mechanisms of self-awareness and emotional regulation but also on the peripheral physiological pathways that may sustain these changes. At the neural level, yoga appears to strengthen SRP-related hubs such as the mPFC and PCC, regions central to self-reflection, autobiographical memory and emotion regulation. Dysfunctions in these networks are strongly linked to psychiatric conditions, including depression, anxiety and posttraumatic stress disorder, which are characterized by maladaptive self-focus and impaired emotional control. By reinforcing these circuits, yoga may reduce negative rumination, foster balanced selfappraisal, and enhance emotional resilience. These insights carry important clinical implications, suggesting that yoga can serve as a complementary intervention alongside psychotherapeutic approaches such as cognitive behavioral therapy and mindfulnessbased therapies, improving outcomes in disorders with SRP dysfunction.
Equally significant are the systemic and molecular mechanisms revealed through peripheral biomarkers. Yoga has been shown to elevate BDNF, supporting neuroplasticity in SRP-related brain regions. Normalization of cortisol rhythms through HPA axis regulation reduces stress-induced distortions of self-processing. The downregulation of inflammatory cytokines such as IL-6, TNF-α and CRP provides further resilience by protecting against inflammationdriven neural decline, while emerging evidence suggests that yoga may modulate NAD⁺-dependent Sirtuin-1 (SIRT1) pathways, supporting mitochondrial function, DNA repair, and healthy brain aging. These biomarker pathways not only validate yoga’s influence beyond the brain but also provide measurable physiological targets that can be tracked in future intervention studies. Clinically, the convergence of neural and biomarker evidence underscores yoga’s potential role in treatment and prevention. For patients with mood and trauma-related disorders, biomarker modulation may complement neural changes, accelerating recovery and reducing relapse. Reductions in cortisol and inflammation could directly mediate symptom improvement in stress-related conditions, while increases in BDNF may support cognitive flexibility and attentional control. This integrative approach suggests yoga could be prescribed as part of personalized, multi-modal treatment strategies in psychiatry and psychology.
Beyond clinical contexts, the implications extend to preventive and community-based applications. Incorporating yoga into schools may promote self-regulation, emotional balance and academic performance by shaping both neural pathways and stress biomarkers during formative years. In workplace settings, yogabased programs may reduce burnout by regulating stress hormones and inflammatory markers while enhancing attentional stability. Among older adults, biomarker modulation, particularly involving BDNF and SIRT1, may slow age-related cognitive decline, strengthen cognitive reserve and reduce vulnerability to neurodegenerative processes such as Alzheimer’s disease. At a societal level, these findings emphasize yoga’s potential as a cost-effective, accessible intervention that bridges mental and physical health. By highlighting both neural adaptations and biomarker modulation, this study encourages the integration of yoga into public health frameworks, community programs and preventive strategies. Ultimately, yoga represents a multidimensional intervention that simultaneously targets brain structure, functional connectivity, autonomic balance and peripheral physiology to cultivate adaptive SRP, psychological well-being and resilience across the lifespan.
Conclusion
Yoga represents a multidimensional intervention that influences Self-Referential Processing (SRP) through coordinated changes in neural activity and peripheral physiology. Structural and functional brain adaptations, particularly enhanced connectivity within the medial prefrontal cortex and posterior cingulate cortex, support improved self-awareness, emotion regulation and cognitive flexibility. Concurrently, modulation of the autonomic nervous system fosters parasympathetic balance, creating physiological conditions conducive to introspection and resilience. At the molecular level, yoga elevates BDNF, stabilizes cortisol rhythms, downregulates pro-inflammatory cytokines (IL-6, TNF-α, CRP), and shows potential for activating Sirtuin-1 pathways, collectively enhancing neuroplasticity, stress resilience and systemic health. The convergence of these neural and biomarker effects underscores yoga’s potential as both a therapeutic and preventive tool, with implications for managing mood disorders, reducing cognitive decline and promoting psychological well-being. Future multimodal, longitudinal studies are warranted to validate these pathways and establish yoga as a scientifically grounded intervention for mental health and brain aging.
References
- Saeed SA, Cunningham K, Bloch RM (2019) Depression and anxiety disorders: Benefits of exercise, yoga, and meditation. Am Fam Physician 99(10): 620-627.
- Shohani M, Badfar G, Nasirkandy MP, Kaikhavani S, Rahmati S, et al. (2018) The effect of yoga on stress, anxiety, and depression in women. Int J Prev Med 9: 21.
- Glisky EL, Marquine MJ (2009) Semantic and self-referential processing of positive and negative trait adjectives in older adults. Memory 17(2): 144-157.
- Yoon HJ, Seo EH, Kim JJ, Choo IH (2019) Neural correlates of self-referential processing and their clinical implications in social anxiety disorder. Clin Psychopharmacol Neurosci 17(1): 12-24.
- Raichle ME (2015) The brain’s default mode network. Annu Rev Neurosci 38: 433-447.
- Hamilton JP, Farmer M, Fogelman P, Gotlib IH (2015) Depressive rumination, the default-mode network, and the dark matter of clinical neuroscience. Biol Psychiatry 78(4): 224-230.
- Nourollahimoghadam E, Gorji S, Gorji A, Khaleghi GM (2021) Therapeutic role of yoga in neuropsychological disorders. World J psychiatry 11(10): 754-773.
- Froeliger B, Garland EL, Mcclernon FJ (2012) Yoga meditation practitioners exhibit greater gray matter volume and fewer reported cognitive failures: Results of a preliminary voxel-based morphometric analysis. Evidence-Based Complement Altern Med 2012: 821307.
- Rathore M, Verma M, Nirwan M, Trivedi S, Pai V, et al. (2022) Functional connectivity of prefrontal cortex in various meditation techniques-A mini-review. Int J Yoga 15: 187-194.
- Brown RP, Gerbarg PL (2005) Sudarshan kriya yogic breathing in the treatment of stress, anxiety, and depression. Part II--clinical applications and guidelines. J Altern Complement Med 11(4): 711-717.
- Si X, Huang D, Sun Y, Huang S, Huang H, et al. (2023) Transformer-based ensemble deep learning model for EEG-based emotion recognition. Brain Science Advances 9: 210-223.
- Tolahunase MR, Sagar R, Faiq M, Dada R (2018) Yoga-and meditation-based lifestyle intervention increases neuroplasticity and reduces severity of major depressive disorder: A randomized controlled trial. Restor Neurol Neurosci 36(3): 423-442.
- Villemure C, ÄŒeko M, Cotton VA, Bushnell MC (2015) Neuroprotective effects of yoga practice: Age-, experience-, and frequency-dependent plasticity. Front Hum Neurosci 9: 281.
- Hernández SE, Suero J, Barros A, González MJL, Rubia K, et al. (2016) Increased grey matter associated with long-term sahaja yoga meditation: A voxel-based morphometry study. PLoS One 11(3): e0150757.
- Flores BA, Millón C, Gago B, García DL, Cantero GN, et al. (2019) Galanin (1-15)-fluoxetine interaction in the novel object recognition test. Involvement of 5-HT1A receptors in the prefrontal cortex of the rats. Neuropharmacology 155: 104-112.
- Cai H, Fields MA, Hoshino R, Priore LV (2012) Effects of aging and anatomic location on gene expression in human retina. Front Aging Neurosci 4: 8.
- Yuan JP, Connolly CG, Henje E, Sugrue LP, Yang TT, et al. (2020) Gray matter changes in adolescents participating in a meditation training. Front Hum Neurosci 14: 319.
- Raja R, Na X, Glasier CM, Badger TM, Bellando J, et al. (2021) Associations between cortical asymmetry and domain specific cognitive functions in healthy children. 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), IEEE, pp. 3127-3132.
- Santaella DF, Balardin JB, Afonso RF, Giorjiani GM, Sato JR, et al. (2019) Greater anteroposterior default mode network functional connectivity in long-term elderly yoga practitioners. Front Aging Neurosci 11: 158.
- Bremer B, Wu Q, Mora Álvarez MG, Hölzel BK, Wilhelm M, et al. (2022) Mindfulness meditation increases default mode, salience and central executive network connectivity. Sci Rep 12(1): 13219.
- Creswell JD (2017) Mindfulness interventions. Annu Rev Psychol 68: 491-516.
- Kanthi A, Deepeshwar S, Kaligal C, Chidananda, Mahadevappa V, et al. (2022) Efficacy of yoga practices on emotion regulation and mindfulness in type 2 diabetes mellitus patients. Yoga Mimamsa 54(1): 12-17.
- Kamath K, Shruthi P, Sukumar S, Vaishali K, Shivashankar KN, et al. (2025) Impact of yoga on the cognitive function among desk‐based workers. A single-centered trial study F1000Res 13: 277.
- Namratha HG, George VM, Bajaj G, Mridula J, Bhat JS, et al. (2017) Effect of yoga and working memory training on cognitive communicative abilities among middle aged adults. Complement Ther Clin Pract 28: 92-100.
- Miyoshi T, Ida H, Nishimura Y, Ako S, Otsuka F, et al. (2022) Effects of yoga and mindfulness programs on self-compassion in medical professionals during the covid-19 pandemic: An intervention study. Int J Environ Res Public Health 19(19): 12523.
- Zeidan F, Johnson SK, Diamond BJ, David Z, Goolkasian P, et al. (2010) Mindfulness meditation improves cognition: Evidence of brief mental training. Conscious Cogn 19(2): 597-605.
- Woodyard C (2011) Exploring the therapeutic effects of yoga and its ability to increase quality of life. Int J Yoga 4(2): 49-54.
- Liu L, Liu C, Tang L, Feng Q, Wang X, et al. (2025) From contemplation to serenity: How yoga meditation improves the mental health of female college students? Front Psychol 16: 1545943.
- Kuppusamy M, Kamaldeen D, Pitani R, Amaldas J, Ramasamy P, et al. (2020) Effects of yoga breathing practice on heart rate variability in healthy adolescents: A randomized controlled trial. Integr Med Res 9(1): 28-32.
- Janjhua Y, Chaudhary R, Sharma N, Kumar K (2020) A study on effect of yoga on emotional regulation, self-esteem, and feelings of adolescents. J Fam Med Prim Care 9(7): 3381-3386.
- Gotink RA, Vernooij MW, Ikram MA, Niessen WJ, Krestin GP, et al. (2018) Meditation and yoga practice are associated with smaller right amygdala volume: The rotterdam study. Brain Imaging Behav 12(16): 1631-1639.
- Kopetz CE, Woerner JI, Briskin JL (2018) Another look at impulsivity: Could impulsive behavior be strategic? Soc Personal Psychol Compass 12(5): e12385.
- Friedman NP, Robbins TW (2022) The role of prefrontal cortex in cognitive control and executive function. Neuropsychopharmacology 47(1): 72-89.
- Marchand WR (2012) Self-referential thinking, suicide, and function of the cortical midline structures and striatum in mood disorders: Possible implications for treatment studies of mindfulness-based interventions for bipolar depression. Depress Res Treat 2012: 246725.
- Dunn NA, Luchner AF (2022) The emotional impact of self‐criticism on self‐reflection and rumination. Psychol Psychother 95(4): 1126-1139.
- Krishna D, Singh D, Prasanna K (2022) A cross-sectional study on impulsiveness, mindfulness, and world health organization quality of life in heartfulness meditators. Yoga Mimamsa 54(1): 24-30.
- Krishna D, Krishna P, Singh D (2025) Neural correlates of impulsivity and frontal electroencephalogram oscillations in heartfulness meditators: A cross-sectional study. Altern Ther Health Med 31(4): 42-47.
- Afonso RF, Kraft I, Aratanha MA, Kozasa EH (2020) Neural correlates of meditation: A review of structural and functional MRI studies. Front Biosci (Schol Ed) 12: 92-115.
- Martin RE, Ochsner KN (2016) The neuroscience of emotion regulation development: Implications for education. Curr Opin Behav Sci 10: 142-148.
- Gonçalves SF, Chaplin TM, López R, Regalario IM, Niehaus CE, et al. (2021) High-frequency heart rate variability and emotion-driven impulse control difficulties during adolescence: Examining experienced and expressed negative emotion as moderators. J Early Adolesc 41(8): 1151-1176.
- Bathina S, Das UN (2015) Brain-derived neurotrophic factor and its clinical implications. Arch Med Sci 11(6): 1164-1178.
- Cahn BR, Goodman MS, Peterson CT, Maturi R, Mills PJ, et al. (2017) Yoga, meditation and mind-body health: Increased BDNF, cortisol awakening response, and altered inflammatory marker expression after a 3-month yoga and meditation retreat. Front Hum Neurosci 11: 315.
- Weller JA, Buchanan TW, Shackleford C, Morganstern A, Hartman JJ, et al. (2014) Diurnal cortisol rhythm is associated with increased risky decision-making in older adults. Psychol Aging 29(2): 271-283.
- Thirthalli J, Naveen G, Rao M (2013) Cortisol and antidepressant effects of yoga. Indian J Psychiatry 55 (Suppl 3): S405-408.
- Djalilova DM, Schulz PS, Berger AM, Case AJ, Kupzyk KA, et al. (2019) Impact of yoga on inflammatory biomarkers: A systematic review. Biol Res Nurs 21(2): 198-209.
- Zhao L, Cao J, Hu K, He X, Yun D, et al. (2020) Sirtuins and their biological relevance in aging and age-related diseases. Aging Dis 11(4): 927-945.
- Gautam S, Kumar U, Kumar M, Rana D, Dada R, et al. (2021) Yoga improves mitochondrial health and reduces severity of autoimmune inflammatory arthritis: A randomized controlled trial. Mitochondrion 58: 147-159.
- Ng F, Wijaya L, Tang BL (2015) SIRT1 in the brain-connections with aging-associated disorders and lifespan. Front Cell Neurosci 9: 64.
- Gard T, Hölzel BK, Lazar SW (2014) The potential effects of meditation on age‐related cognitive decline: A systematic review. Ann NY Acad Sci 1307: 89-103.
- Krishna D, Prasanna K, Angadi B, Singh BK, Anurag S, et al. (2022) Heartfulness meditation alters electroencephalogram oscillations: An electroencephalogram study. Int J Yoga 15(3): 205-214.
- Trivedi GY, Kathirvel S, Sharma K, Saboo B (2023) Effect of various lengths of respiration on heart rate variability during simple bhramari (humming). Int J Yoga 16(2): 123-131.
- Li X, Zhou Y, Zhang C, Wang H, Wang X, et al. (2024) Neural correlates of breath work, mental imagery of yoga postures, and meditation in yoga practitioners: A functional near-infrared spectroscopy study. Front Neurosci 18: 1322071.
© 2025 Dwivedi Krishna. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






