- Submissions

Full Text
Research in Medical & Engineering Sciences
Increasing Collaboration and Reducing Problem Behaviors Through Tele-Rehabilitation Using a Remote System
Paola Chilà1,2†, Chiara Failla1,3†, Ileana Scarcella1,2, Roberta Minutoli1,2, Noemi Vetrano1,4, Germana Doria1,2, Antonio Cerasa1,5,6, Flavia Marino1* and Giovanni Pioggia1
1Institute for Biomedical Research and Innovation (IRIB), National Research Council of Italy (CNR), 98164 Messina, Italy
2International Telematic University Uninettuno, Corso Vittorio Emanuele II, 39, 00186, Roma
3Classical Linguistic Studies and Education Department, Kore University of Enna, 94100 Enna, Italy
4Department of cognitive, psychological and pedagogical sciences, and cultural studies, University of Messina, Via Concezione, 6/8, 98121 Messina
5S’Anna Institute, 88900 Crotone, Italy
6Pharmacotechnology Documentation and Transfer Unit, Preclinical and Translational Pharmacology, Department of Pharmacy, Health Science and Nutrition, University of Calabria, 87036 Arcavacata, Italy
††These authors contributed equally to the study
*Corresponding author:Flavia Marino, Institute for Biomedical Research and Innovation (IRIB), National Research Council of Italy (CNR), 98164 Messina, Italy
Submission: March 17, 2023Published: March 27, 2023

ISSN: 2576-8816Volume10 Issue2
Abstract
Remote healthcare services have emerged as a viable approach to behavior management interventions and provide emotional support to healthcare professionals in various clinical domains. They have been shown to impact the mental well-being of children diagnosed with autism spectrum disorder (ASD) and also their parents. Managing challenging behaviors in children with autism is often one of the frequent challenges parents and caregivers have to face. Our study demonstrates that the online Behavioral Skill Training (BST) program can support clinical Applied Behavior Analysis (ABA) interventions in the management of problem behaviors. In fact, in our case report the use of telemedicine led to effective results including an increase in collaborative behaviors and a reduced frequency of problematic behaviors.
Keywords:Autism; Telehealth; Behavioral skills training program
Abbreviations:ABA: Applied Behavior Analysis; ABC: Antecedent Behavior Consequence; ASD: Autism Spectrum Disorder; BST: Behavioral Skill Training; ABC: Antecedent Behavior Consequence; GMDS-ER: Griffiths Mental Development Scales-Extended Revised
Introduction
Telehealth uses technology to facilitate remote access to healthcare services [1]. With the COVID-19 pandemic, telehealth has become an important tool for healthcare professionals to provide care while minimizing the risk of virus transmission [2]. Telehealth has been found to be particularly helpful for children with Autism Spectrum Disorder (ASD) and their families because it enables parents to access support and guidance from healthcare professionals remotely, without the need for in-person visits and offers more flexibility in scheduling appointments [3]. The delivery of services at a distance is a new and effective way of implementing rehabilitation interventions without compromising the safety of children their families, and operators. Telemedicine offers continuous and ubiquitous access to care for families with children with ASD, directly involving family members in the child’s development [4]. ASD is often characterized by social deficits and problem behaviors, which have a significant impact on the daily life of the child and their family. Early and intensive interventions are therefore crucial for functional outcomes and improvements in developmental trajectories [5]. In recent years, telehealth has emerged as a promising tool for behavior management interventions aimed at children with ASD [6]. Through telehealth, parents can learn strategies for managing problem behaviors, receive coaching on how to implement these strategies, and track progress over time. Remote training for parents of children with ASD can increase their skills in managing problem behaviors and improve their ability to conduct a functional analysis and use functional communication techniques [7,8]. Telemedicine tools are thus effective in managing problem behaviors in family contexts.
This study illustrates how the use of technological tools can assist ABA clinical work in increasing collaboration with requests and reducing problem behaviors. Our online parenting program is centered around the use of Behavioral Skills Training (BST). This approach has been developed to address specific problem behaviors in children with ASD and involves a combination of modeling and prompting techniques [9] and is used within the context of function-based treatments [10] and functional analyses [11]. While the efficacy of the BST method has been extensively demonstrated in various clinical settings, its application in remote health service programs has not been thoroughly examined.
Case Presentation
This case study involved the use of a telematic behavioral skills training program to manage a specific problem behavior of a boy with ASD (G.T.). The patient is a 5 years old child that was diagnosed with ASD through the Autism diagnostic Observation Schedule (ADOS-2). His development quotient evaluated with the Griffiths Mental Development Scales, Extended Revised (GMDS-ER 2-8) was 100. At language level, G.T. was only able to formulate short phrases. G.T. ranked at level 2 of the VB. MAPP [12]. The functional assessment highlights consolidated skills in the area of mands, tacts, visual-perceptual skills, and independent play. Deficiencies are found in the area of social behavior and social play, imitation and echoic.
The case study was conducted through a web platform [G-Suite; Google LLC; Mountain View, CA, USA)] using video conferencing tools. In this parent training program, parents were provided with a tablet for the training and to record their sessions, which were then analyzed. The therapist and parents had a brief video conference or phone call before and after each session to discuss procedures, outcomes, and plan for the next session. Both parents were required to participate in the training. Parents provided informed consent for inclusion prior to their participation in the study. The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Committee of the Research Ethics and Bioethics Committee (http://www.cnr.it/ethics, accessed on 17 December 2021) of the National Research Council of Italy (CNR) (Prot. No. CNR-AMMCEN 54444/2018 01/08/2018) and by the Ethics Committee Palermo 1 (http://www.policlinico. pa.it/, accessed on 17 December 2021) of Azienda Ospedaliera Universitaria Policlinico Paolo Giaccone Palermo (report No. 10/2020- 25/11/2020).
During the COVID-19 pandemic lockdown, G.T. exhibited behavior problems related to the parental management of the word “no”. G.T’s problem behavior was characterized by verbal protests as precursors to more disruptive behavior. Specifically, after emitting the verbal protest, if the parents did not stop giving G.T the instruction, he would throw himself on the ground, pick up and throw objects around, and bang his head against the floor. Before starting the intervention, the therapist organized an online meeting with the family and explained the study methods to the parents. During the first meeting, the therapist collected information about the child’s behavior and discussed it with the parents. Towards the end of the meeting, the therapist provided the parents with an individualized frequency checklist to help them define and track the problem behavior they reported. The therapist and parents then discussed the frequency checklist results and selected the target behavior for the study. The therapist then established a baseline for the problem behavior during the second meeting. The parents were then asked at the end of the meeting to video the target behavior during the following week.
The therapist then held the third meeting with the parents and introduced them to the Antecedent-Behavior-Consequence (ABC) worksheet. The therapist used the recorded videos to fill in the worksheet, helping the parents understand and identify the events that preceded (antecedents) and followed (consequences) the problem behavior. Live coaching was provided to the parents during the session to teach them how to use functional analysis. The therapist then instructed the parents on how to complete the ABC worksheet. Short videos were used to help the parents interpret the problem behavior and complete the worksheet with the therapist’s assistance. Finally, the therapist asked the parents to continue recording videos and also to record data on the ABC worksheet for the following week.
The therapist then focused on analyzing the completed ABC worksheet provided by the parents. The therapist was thus able to determine the function of the behavior which was monitored through the recorded videos. Based on this analysis, the therapist explained to the parents the correct behavioral procedures to follow in order to facilitate a positive change. Behavioral Skills Training (BST) was used during sessions to teach new skills. This approach involves several steps, including instruction, modeling, rehearsal, and feedback. Initially, the therapist explains the skill to the parents and then demonstrates how to perform it. Next, the parents practice the skill with a role-playing exercise during the session. Finally, the therapist provides feedback on the parent’s performance to reinforce positive behavior. As a supplementary measure to the online coaching, parents were provided with written instructions on the procedure as homework at the end of each meeting. The aim of these instructions was to reinforce and clarify the skills that were taught during the session. For G.T, the intervention was based on a functional analysis of the problematic behavior and the manipulation of motivational and consequential variables. For the motivational variable, the high-probability request sequence (high-p) procedure was used, which involved presenting high-probability requests before low-probability ones in order to increase task cooperation. The low probability request in this case was handwashing, which was problematic behavior. Additionally, the therapist suggested using tokens as rewards in order to solicit and then reinforce desired behaviors. A list of backup reinforcers was established which G.T could sometimes choose from, and instructions were provided on how to complete the behavioral chain in order to obtain the generalized conditioned reinforcement represented by the token.
During the final phase of the study, the therapist held a debriefing session with the parents to review the tasks that had been assigned in the previous phases. The goal was to ensure that the parents had a clear understanding of the interventions and the progress made during the study. The parents also gave their feedback regarding their impressions of the intervention.
The intervention yielded positive results, with a significant reduction in problem behavior. Based on the manipulation of motivational variables using the high-probability request sequence (high-p), the child’s compliance with high-probability requests increased, reducing the emission of problem behaviors.
The introduction of a token economy also provided symbolic reinforcement for completing the behavioral chain, further increasing the child’s compliance with parental requests. These results demonstrate the effectiveness of the intervention offered via telemedicine using the BST techniques to decrease problem behavior.
Discussion
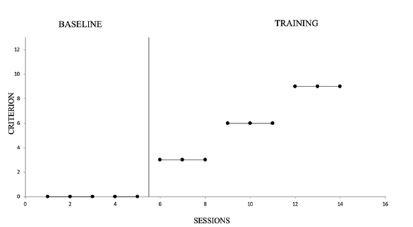
Research findings suggest that a telehealth intervention based on Applied Behavior Analysis (ABA) could be a useful and effective treatment for families with children on the autism spectrum. This study, in fact, tested the effectiveness of BST procedures to reduce problem behaviors and to increase G.T ‘s compliance during the COVID-19 lockdown. In fact, the graphs in Table 1 & 2, show an increase in collaborative behavior with a consequent reduction in “no” answers. The intervention was conducted remotely with the aid of technological tools. The results demonstrate the positive impact on reducing problematic behaviors and increasing children’s compliance by offering support to parents using telemedicine.
Table 1Reduction of problem behaviors.
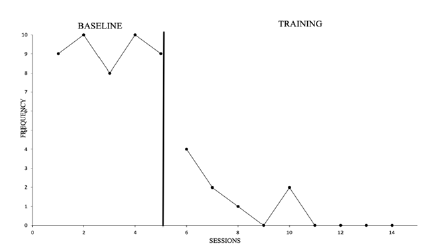
Table 2Collaborative behaviors.
Acknowledgement
The author appreciates the contributions Eleonora Orru who supervised the clinical procedures.
Conflict of Interest
There is no conflict of interest to declare.
<Funding
This research was funded by Project INTER PARES “Inclusione, Tecnologie e Rete: un Progetto per l’Autismo fra Ricerca, E-health e Sociale”-POC Metro 2014-2020, Municipality of Messina, ME 1.3.1.b, CUP F49J18000370006, CIG 7828294093.
References
- Bashshur RL, Doarn CR, Frenk JM, Kvedar JC, Woolliscroft JO (2017) Telemedicine and the COVID-19 pandemic, lessons for the future. Telemed J E Health 26(5): 571-573.
- Monaghesh E, Hajizadeh A (2020) The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health 20(1): 1193.
- Gabellone A, Marzulli L, Matera E, Petruzzelli MG, Margari A, et al., (2022) Expectations and concerns about the use of telemedicine for autism spectrum disorder: A cross-sectional survey of parents and healthcare professionals. J Clin Med 11(12): 3294.
- Solomon D, Soares N (2020) Telehealth approaches to care coordination in autism spectrum disorder. Interprofessional Care Coordination for Pediatric Autism Spectrum Disorder pp: 289-306.
- Marino F, Chilà P, Failla C, Crimi I, Minutoli R, et al. (2020) Tele-assisted behavioral intervention for families with children with autism spectrum disorders: A randomized control trial. Brain Sci 10(9): 649.
- Lord C, Elsabbagh M, Baird G, Veenstra Vanderweele J (2018) Autism spectrum disorder. Lancet 392(10146): 508-520.
- Wacker DP, Lee JF, Dalmau YCP, Kopelman TD, Lindgren SD, et al. (2013) Conducting functional communication training via telehealth to reduce the problem behavior of young children with autism. J Dev Phys Disabil 25(1): 35-48.
- Hao Y, Franco JH, Sundarrajan M, Chen Y (2021) A pilot study comparing tele-therapy and in-person therapy: Perspectives from parent-mediated intervention for children with autism spectrum disorder. J Autism Dev Disord 51(1): 129-143.
- Koegel RL, Glahn TJ, Nieminen GS (1978) Generalization of parent-training results. J Appl Behav Anal 11(1): 95-109.
- Robertson RE, Wehby JH, King SM (2013) Increased parent reinforcement of spontaneous requests in children with autism spectrum disorder: Effects on problem behavior. Res Dev Disabil 34(3): 1069-1082.
- Stokes JV, Luiselli JK (2008) In-home parent training of functional analysis skills. Int J Behav Consult Ther 4(3): 259-263.
- Sundberg ML (2008) VB-MAPP verbal behavior milestones assessment and placement program: A language and social skills assessment program for children with autism or other developmental disabilities: guide. Mark Sundberg.
© 2023 Flavia Marino. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)













.bmp)
.jpg)
.png)
.jpg)














.png)

.png)



.png)






