- Submissions

Full Text
Trends in Telemedicine & E-health
Investigating Factors of Interoperability of Electronic Medical Record Systems in Hospitals: A Narrative Literature Review
Mercy Mbise, Neema Mkayula* and Masoud Mahundi
Department of Computer Science and Engineering, University of Dares Salaam, Tanzania
*Corresponding author:Neema Mkayula, Department of Computer Science and Engineering, College of Information and Communication Technologies, University of Dares Salaam, Tanzania
Submission: February 13, 2024; Published: May 02, 2024

ISSN: 2689-2707 Volume 5 Issue 1
Abstract
Background:Interoperable Electronic Medical Record (EMR) supports health information exchange
from different service systems and provide convenient access to healthcare services. Despite these
undisputable benefits, achieving interoperability between EMR systems has always been challenging.
This study attempted to investigate factors that influence interoperability of EMR systems in hospitals.
Methods:The study employed a narrative review which involved a systematic search of articles from
January 2010 to November 2020. Five electronic databases were searched, which are Science Direct,
PubMed, Jstor, IEEE and Google Scholar. Data were analyzed using principles of thematic analysis.
Results:Using keyword search terms, 22609 articles were identified from database searching, whereby
565 articles were retrieved from databases after applying advanced search; the final review comprised of
17 articles which were then used for the study. Eight factors emerged (i) adherence to medical standards,
(ii) the existence of medical terminologies and controlled vocabularies, (iii) the use of standardized data
types, (iv) adherence to communication channels or protocols, (v) the influence of political supremacy
(vi) existence of diverse social background, (vii) legal aspects, and (viii) availability of resources.
Conclusion:This review found that interoperability is possible given that actors will address these
factors, which are both organizational and technical.
Keywords:Interoperability; Electronic medical records; Narrative review; Health information system inclusion and exclusion criteria
Introduction
Health Information System (HIS) is a system that manages health information on a national or sub- national scale. With the advent of technology, HIS uses computers to support the various processes involved in managing healthcare service delivery [1] including improved processing of data to deliver information useful for decision-making in the healthcare environments [2]. The major advantage of HIS, therefore, is to contribute to efficient and high-quality healthcare services [3]. In hospital settings, HIS are coordinated through Electronic Medical Record (EMR) systems [4]. These are HIS through which patient detailed information such as demographic, medical health history, and laboratory results are recorded by healthcare service providers [5,6]. EMR systems assist healthcare providers to streamline the flow of patients’ information and its accessibility [7]. Hospitals which manage medical records electronically use different EMR systems [8]. These differences in EMR can be within one hospital where different sections like the outpatient department, reproductive health, pharmacy, and laboratory, all have different systems. Or it can be between hospitals, where one hospital has one system and a higher referral hospital has another. One of the key challenges standing in the way of reaping the benefits of EMRs is poor interoperability among different systems forming EMRs within a particular hospital or across related hospital units. Many attempts towards interoperability have ended up in futility despite the agreed benefits of interoperability. Several researchers have therefore differently engaged the interoperability question. The field has therefore been under the attention of research over many years. For instance, [9] conducted a study on breaking the healthcare interoperability barrier in the healthcare system in Canada, and [10] did the study on technical interoperability solutions among electronic health record systems for public health organizations in Brazil.
Although these studies have given light upon factors that influence interoperability, there still lacks a comprehensive understanding of factors which influence the achievement of interoperable HIS, especially in the hospital settings. This study contends that there is a need to have a comprehensive understanding of what influences interoperability, both positively and negatively. The research question that is addressed is: “what factors influence the achievement of interoperability of electronic medical record systems?” The study engages this question through a narrative literature review to understand these factors. The study contributes to the discourses on interoperability by enhancing clarity on the relating components of interoperability, generally, and identifying factors for interoperability, in particular.
Literature Review
Interoperability and EMR systems
Several definitions exist on the term “Interoperability” depending on different contexts in different studies. Interoperability is the ability of different information systems, devices, or applications to cooperatively use and exchange health information and services that ensures continuity of care within and across organizations [9,11,12]. Further, Braa and Sahay define interoperability as the ability to exchange information between two or more systems [13]. In 1990, however, the IEEE defined interoperability as “the ability of two or more systems or components to exchange information and to use the information that has been exchanged” [14].
Interoperable EMR systems are systems that allow information sharing, providing continuous workflow of service, integrated information flow, and enabling healthcare decision making, hence promoting wellness and improving health outcomes [15,16]. Interoperability, in the hospital settings, is the ability of heterogeneous EMR systems and computer applications to communicate and exchange information accurately, effectively, consistently, and use the exchanged information [3]. It is a key feature in the hospital HIS because in order to accomplish effectiveness, efficient, and coordinated care, information must be shared between healthcare organizations, doctors, pharmacists, nurses, and patients [17,18].
In the health sector generally and the EMRs in particular, interoperability is a significant endeavor because the sector is relatively more complex and highly politicized [19]. This complexity and politicisation mean several electronic systems serving related purposes [20]. Interoperable systems, therefore, provide a common view of important information for a patient to any healthcare provider involved in the circle of care [9]. Interoperable EMR systems lead to the provision of high-quality health information as they cover information across a wide range of systems, and provide fast and convenient access to healthcare services and cost reduction [21,22]. Interoperability of EMR has many advantages such as contributing to appropriate decision-making that in turn improve the health of clients [18,20,23]. Additionally, there is saving of time, reduction of costs, increased transparency and improved quality of the service offered [3,24,25]. This also includes better compilation of a patients’ information such that an overall health status of the patients is observed [21,26], hence enabling different EMR systems from different providers to communicate and share resources [26].
Narrative literature review
A narrative literature review is a research strategy in which previous research is systematically gathered and synthesized [27,28]. The narrative review reports the author’s findings in a condensed manner that summarizes the contents of the reviewed articles, with the goal of objectively presenting the current state of knowledge on a topic, based on previously published research [29]. The integration of findings and viewpoints from various empirical discoveries results in a more efficient manner of answering research issues, which is accomplished through already published publications. The advantage of a narrative review is that it enables a researcher to save time when examining or seeking information [28,30,31]. In narrative review, a researcher has the advantage to read the reviewed articles rather than wasting time going through a large volume of literature. It also provides information for decisionmakers and researchers who utilize narrative reviews of literature to find, justify, and develop ideas, as well as recognize and avoid previous research pitfalls. Additionally, a narrative literature review can be used to validate assumptions, get insight into the dynamics that underpin other studies’ conclusions, and provide more conclusive results than a single primary research study.
A typical narrative literature review comprises the following structure [28]: (1) Literature search, (2) Search terms, (3) Selection criteria (4) Critical assessment and (5) Writing the review. The literature search phase specifies search databases to employ in the search and defines the selection bias. Appropriate search terms are identified in such a way that they allow selection of all relevant articles while also excluding those that are not. Inclusion and exclusion criteria for literature selection can support in focusing on the research relevance to the topic during the selection criteria phase. The exclusion criteria are determined based on the relevance of the search target, whereas the inclusion criteria establish the key elements of the review. Critical assessment evaluates the articles according to key results, limitations, suitability of the methods used to test the initial hypothesis, quality of the results obtained, interpretation of the results, and impact of the conclusion in the field [28]. This article’s Materials and Methods section explains how each of these processes was accomplished.
Materials and Methods
Literature search
To investigate what influences interoperability of EMR in hospitals, a literature search was carried out from August to November 2020. The last search was done on 26th November 2020. The search was performed from the following electronic databases: Google Scholar, PubMed, Jstor, Science Direct and IEEE as indicated in Table 1. These electronic databases were chosen because they provide health informatics databases including EMR systems, and offer a set of search options for enhancing reference retrieval. The search used the terms (“electronic medical records” OR “electronic health records” OR “patient health records” OR “Hospital Information System” OR “Health Information System”) AND (interoperability OR interoperable) and advanced search was such that the article title should include the term/keyword (“Interoperability”).
Table 1:Literature search factors influencing interoperability of EMR.

Inclusion/exclusion criteria
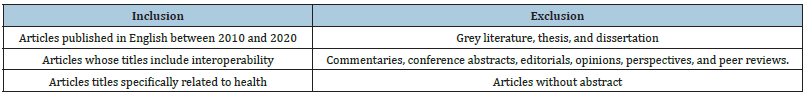
Search terms were identified to formulate the most inclusive search. The retrieved literature was screened for eligibility according to pre-specified inclusion and exclusion criteria as shown in Table 2.
Table 2:Inclusion and exclusion criteria.
Search results and study selection strategy
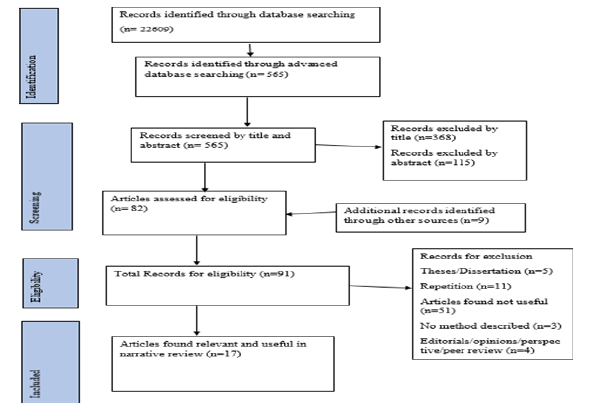
The initial search yielded 22609 articles from database search. The statistics of the search from the databases was based on the search criteria used. However, these results needed to be screened to remove all articles that were irrelevant to the study. By applying advanced search criteria, a total 565 articles were retrieved from databases. Out of those, 368 articles were excluded by the title criterion, while 115 articles were excluded by the abstract criterion. The remaining 82 articles were considered for the study, and 9 articles were added from other sources, hence making a total of 91 articles. From the 91 articles, 5 articles were theses/dissertations, 4 articles were editorials/opinions/perspective/peer review, and 3 articles had no method defined; 11 articles were duplicates and 51 articles were found not to be relevant to the study. Thus, 17 articles were included in the analysis. Figure 1 depicts the search process.
Figure 1:Flowchart of the literature search process.
Result
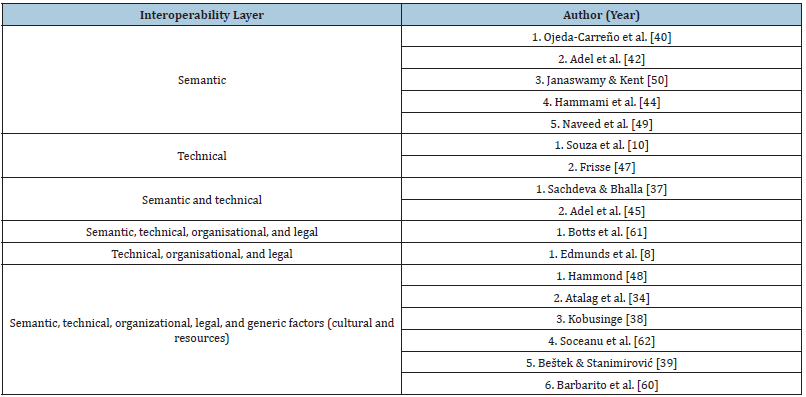
Seventeen (17) articles were found to be relevant to the study, in which eight (8) were empirical studies and nine (9) were nonempirical studies. Hence, factors that influence interoperability were derived from these 17 articles from the reviewed literature. Initial results show that authors have categorized interoperability based on different layers: technical, semantic, organizational, and legal layers. Hence, from the identified articles, two (2) considered the technical layer; five (5) considered the semantic layer; and only two (2) focused on semantic and technical layers. However, one (1) article considered semantic, technical, organizational, and legal layers, while six (6) articles combined semantic, technical, organizational, and legal layers, including other generic factors such as cultural and resources. Table 3 presents the matrix of the different interoperability layers reported by respective authors. The different interoperability layers are hence described in Section 4.1.
Table 3:Identified interoperability layers by authors.
Layers of interoperability
Health organizations and researchers have defined interoperability layers in different ways. Kuziemsky [32] and Benson [33] report three layers of interoperability: technical, semantic, and process interoperability. European Interoperability Framework (EIF) breaks down interoperability into four layers; semantic (information and service sharing), technical (data and message exchange), organizational (business unit), and legal layer, which ensures that organizations operating under different legal frameworks, policies, and strategies can work together [18]. The Healthcare Information and Management Systems Society (HIMSS) defines “interoperability as the ability of health information systems to work together within and across organizational boundaries to advance the health status of, and the effective delivery of healthcare for, individuals and communities” [34,35]. HIMSS defines three layers of health information technology interoperability; foundational, structural, and semantic interoperability [36].
Although these layers can slightly be different across definitions, they generally follow a distinction between lower-layer technical components and higher-layer organizational components. In line with this conceptualization, [25] defines four layers of interoperability which are technical, syntactic, semantic, and organizational aspects of interoperability. Thus, the identification of factors that influence interoperability in this study mainly adopts EIF because it covers all layers addressed by other health organizations and researchers. Layers of interoperability defined include; technical layer, semantic layer (which covers both semantic and syntactic aspects), organizational layer, and legal layer.
Critical analysis of results
It was found from the articles that interoperability of EMR
systems can be based on different layers. While one author may
place a factor under a certain layer, another author places the
same factor under a different layer of interoperability. Moreover,
other scholars have grouped such factors like medical standards,
medical terminologies and controlled vocabularies, data types,
communication channels, and communication protocols as
standards [34,37], standards which further subdivided into:
i. Message or interface standards: Health Level 7(HL7)
[HL7 2010]; Electronic Data Interchange for Administration,
Commerce and Transport (EDIFACT); and Digital Imaging and
Communications in Medicine (DICOM).
ii. Content-oriented standards: Logical Observation
Identifiers Names and Codes (LOINC); The International
Statistical Classification of Diseases and Related Health
Problems 10th Revision (ICD-10); International Classification
of Procedures in Medicine (ICPM).
iii. Hybrid standards: CEN 13606 and open EHR.
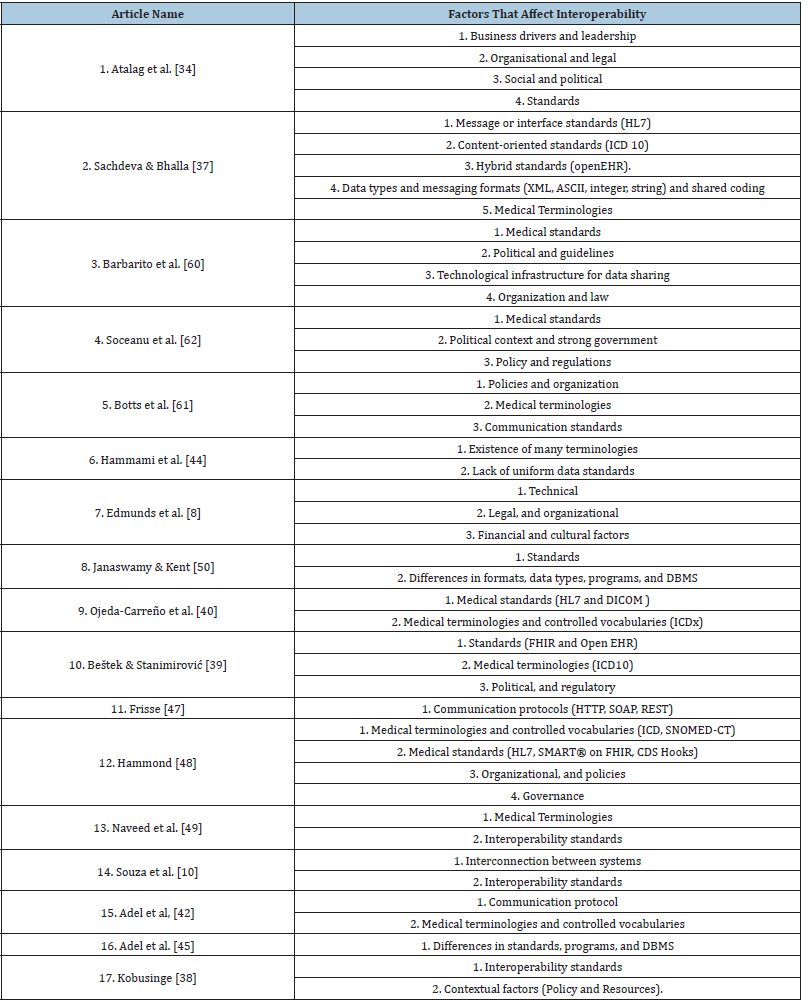
It was also found from the study that some scholars have identified factors that influence interoperability without addressing the layers of interoperability [8,38,39]. These factors are referred as general factors or generic factors that influence interoperability. Hence, this study revealed that factors that influence interoperability may be associated with both the layer concept as well as with generic factors. From the reviewed literature, the study takes on the combination of findings in terms of layers of interoperability and generic factors. Factors that influence interoperability from the identified articles are presented in Table 4.
Table 4:Factors that influence interoperability from articles reviewed.
Findings
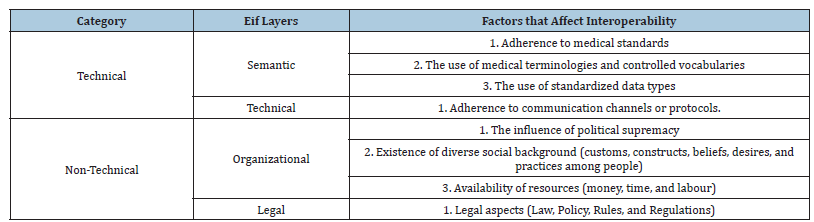
The study identified eight (8) factors in the category of technical and non-technical factors as per summarized in Table 5. These factors are: adherence to medical standards, the existence of medical terminologies and controlled vocabularies, the use of standardized data types, adherence to communication channels or protocols, political contexts, the existence of diverse social background, legal aspects (law, policy, rules, and regulations) and availability of resources. Table 6 shows the linkage between the Categories, EIF layers and factors that influence interoperability.
Table 5:Technical and non-technical factors that influence interoperability.
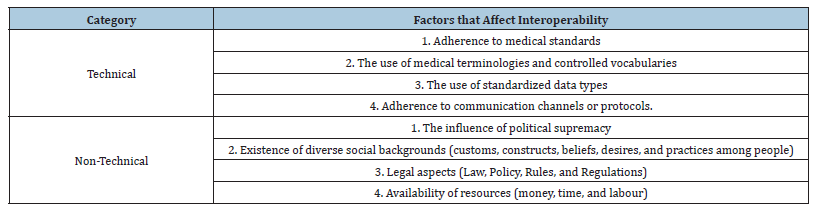
Table 6:Categories, EIF layers and factors that influence interoperability.
Description of factors that influence interoperability
Adherence to medical standards: Medical standards provide a common language and a common set of expectations that allow interoperability between systems and/or devices [33]. Medical standards are defined as standards used in the medical industry to store or communicate information to other systems [12]. Medical standards are approved by a recognized body, which contains repeated practice, rules, and guidelines in a medical setting [4,40]. Adherence to medical standards ensures the communication is faultless and uniform as medical information is shared from doctors and nurses, laboratories, pharmacies, billing departments, insurance companies, and from one hospital to another hospital [12,33,41]. Also, the implementation of common standards has been suggested to facilitate different levels of interoperability within or across health care settings [22]. On the other hand, failure to adhere to medical standards results in a lack of interoperability of EMRs since EMRs rely greatly on medical standards [9,42]. Examples of medical standards are Health Seven Level (HL7) and DICOM.
The existence of medical terminologies and controlled
vocabularies: Medical terminology and controlled vocabulary play
a major role in the interoperability of EMRs between hospitals and
hence facilitate sharing of medical information. Shared medical
terminologies refer to establishing a shared vocabulary for the
interchange of medical information [37,43]. Medical terminologies
allow for representing medical statements in a formalized way
and are vital for implementing automated search and medical
processing; for example, drug interaction check, medical/workflow
controlling, reporting, payment, search/index/query [43]. Medical
terminology is defined as a set of classes each representing a concept
in the medical arena. A class may also be called a term or vocabulary
(sets of terms and meanings) [43]. According to Hammond, lack
of medical terminologies and controlled vocabularies may result
in ineffective communication between EMR since communication
between EMR relies on medical terminologies and controlled
vocabularies. Therefore, failure to adhere to medical terminologies
results in poor interoperability between EMR systems [22,44]. Some
common vocabulary standards currently used in the marketplace
include SNOMED-CT, LOINC, and ICDx, where x can be version 9 or
10 [45]. The definitions of these common vocabulary standards are:
i. ICD-10 and ICD-11: The International Statistical
Classification of Diseases and Related Health Problems (ICD) is
a medical classification list by the World Health Organization
(WHO). It contains codes for diseases, signs and symptoms,
abnormal findings, health management, complaints, social
circumstances, and external causes of injury or diseases [12].
According to the WHO, the 11th revision will replace the ICD-10
in January 2022 [46].
ii. Logical Observation Identifiers Names and Codes
(LOINC®): A universal code system for identifying health
measurements, laboratory observations, and documents [12].
These codes represent the “question” for a test or measurement
[47]. LOINC codes can be grouped into laboratory and clinical
tests, measurements, and observations [48].
iii. Systematized Nomenclature of Medicine-Clinical Terms
(SNOMED-CT): A comprehensive clinical health terminology
product. It enables a consistent and processable representation
of clinical content in electronic health records (EHRs) [12].
These codes often represent the “answer” for a test or
measurement to the LOINC “question” code [47,49].
The use of standardized data types: Data types refer to the categories of data exchanged by EMR systems. Interoperability requires EMR systems to share data types on different messaging formats, for example XML and ASCII; programming languages, for example integer and string, and different database management systems [37,42,50]. The use of standardized data types supports interoperability of EMR systems, hence enables sharing of medical information, while unstandardized data type leads to a lack of interoperability, hence transferring of medical information from one system to another becomes a challenge [51]. Information stored in an EMR system may be either medical or non- medical data, hence EMR systems must have the ability to contain both structured and non- structured data [42,52].
Adherence to communication channels or protocols: Adherence to communication channels or protocols enables EMR interoperability [47]. According to Lehne M et al. [25] moving health information from one point to another requires communication channels and protocol for health information transmission. Emerging and widely used standards for the communication of health information include HL7’s Fast Healthcare Interoperability Resources (FHIR) and Open EHR for the structured exchange of health information [53]. Open EHR defines medical content using the so-called architecture or models and specifications of clinical concepts based on an underlying reference model. Interoperability architectures are models which make use of different technologies and standards. Failure to adhere to architectures that provide a communication channel for health information leads to lack of interoperability among EMR systems [10].
There are communication standards outside the healthcare space that are also useful [12], for example, Application Programming Interfaces (APIs) which allow users to enable data transfer and workflows. Many web-based applications support APIs for information transfer and interoperability. Fast Healthcare Interoperability Resources is an API for exchanging health- related information. Different types of API styles that can use to integrate digital health information include SOAP (Simple Object Access Protocol), REST (Representational State Transfer) and GraphQL [12,36].
The influence of political supremacy: Political contexts play a major role in influencing interoperability since it is necessary for successful planning and interoperability implementation [12]. Without considering political supremacy as a factor that influences interoperability will lead to difficulty in approval of interoperability medical standards and communication standards [12]. Also, political contexts include the need for EMR systems to be designed in accordance with national directives and manners that drive HIS initiatives [32]. Political participation involves individuals or parties who have authority in an organization, hence they determine policy decisions on EMR interoperability, the direction and strategies of the organization [54].
Existence of diverse social background: The existence of diverse social mores, customs, constructs, beliefs, desires, and practices among people in a certain community affect the ability of hospitals to achieve complete interoperability [55,56]. Social aspects have a great influence on EMR systems interoperability [9,33,57]. Social aspects include the underlying cultural issues about hospital-to-hospital and hospital-patient health information sharing [8,20]. Social aspects influence how information is acquired and used in a healthcare setting [32], building relationships and agreement across stakeholder groups about which health information should be collected and what formats should be used [58]. However, social aspects behaviors can be regulated using law [34].
Legal aspects (law, policy, rules and regulations): Legal factors have a great influence on interoperability and can become an obstacle in any interoperability initiative [54]. Organisations are subjected to certain laws, rules and regulations that govern them. These laws could be in the form of policies since a policy, regardless of its scope, expresses a clear rule of law [59]. Policies concern with systems development, system integration and interoperability, health information sharing, and privacy of sensitive health data, among others [60]. Such policies, once established, could help direct EMR interoperability implementations within a country [38]. Discussions on legal structures for a standard are arguably as important as discussions about the appropriate choice of a standard [61]. A governing body that builds interoperability standards must ensure that it complies with the regulations and privacy requirements [9,62]. Interoperability standards need to be managed and legally enforced by the governing body or leadership responsible for the healthcare system. It is believed that strong leadership results in better standards with complete applicability [34].
Availability of resources: Resources that influence EMRs interoperability include money, labour (skilled human resources), and time, among others [63]. Availability of these resources greatly influences interoperability and lack of such resources leads to difficulty in achieving EMR interoperability [38]. According to Edmunds M et al. [8], implementation of interoperable EMRs between hospitals should be aligned with financial incentives because they have to invest in systems that will make it easier for others to achieve cost savings. EMR interoperability reduces duplicative tests and procedures and thereby reduces healthcare costs; hospitals would likely lose revenue when duplicative tests or procedures were avoided [8].
Conclusion
This narrative review of literature has sought, retrieved and described factors that influence interoperability of EMR systems in hospitals. Interoperability of EMR systems support the flow of health information which greatly contribute to appropriate decisionmaking that will in turn improve the health of citizens. Based on the findings of the review, factors that influence interoperability are necessary to be considered to support interoperability efforts and contributions to their success. These factors are: adherence to medical standards, the existence of medical terminologies and controlled vocabularies, the use of standardized data types, adherence to communication channels or protocols, political contexts, the existence of diverse social backgrounds, legal aspects (law, policy, rules, and regulations) and availability of resources. The findings of this study add to the literature, and contribute to the body of knowledge on interoperability of EMR systems.
References
- Akintunde O, Nzechukwu O, Adetunji O (2019) Health information exchange model for Nigerian health information systems. Int J Comput Sci Inf Secur 17(2): 181-203.
- Almunawar MN, Anshari M (2012) Health information systems (HIS): concept and technology. Other Computer Science.
- Jardim SVB (2013) The electronic health record and its contribution to healthcare information systems interoperability. Procedia Technology 9: 940-948.
- Kang’a S, Puttkammer N, Wanyee S, Kimanga D, Madrano J, et al. (2016) A National standards-based assessment on functionality of electronic medical records systems used in Kenyan public-sector health facilities. Int J Med Inform 97: 68-75.
- Ludwick DA, Doucette J, Park S, County S, Care P, et al. (2009) Adopting electronic medical records in primary care: Lessons learned from health information systems implementation experience in seven countries. Int J Med Inform 78(1): 22-31.
- Ranganathan C, Afnan A (2012) Effective implementation of electronic medical record systems: insights from a longitudinal case study.
- Esfahani AA, Ahmadi H, Nilashi M, Alizadeh M, Bashiri A, et al. (2018) An evaluation model for the implementation of hospital information system in public hospitals using multi-criteria-decision-making (MCDM) approaches. Int J Eng Technol 7(1): 1-18.
- Edmunds M, Peddicord D, Frisse ME (2016) Ten reasons why interoperability is difficult. Healthcare Information Management Systems, pp. 127-137.
- Azarm M, Backman C, Kuziemsky C, Peyton L (2017) Breaking the healthcare interoperability barrier by empowering and engaging actors in the healthcare system. Procedia Comput Sci 113: 326-333.
- Souza ADCR, Medeiros AP de, Martins CB (2019) Technical interoperability between electronic health record systems in Brazilian public health organizations. Rev Bras Comput Apl 11(2): 42-55.
- Cresswell KM, Mozaffar H, Lee L, Williams R, Sheikh A (2017) Safety risks associated with the lack of integration and interfacing of hospital health information technologies: A qualitative study of hospital electronic prescribing systems in England. BMJ Qual Saf 26(7): 530-541.
- Aziz SUA, Askari M, Shah SN (2020) Standards for digital health. Diabetes Digital Health. pp: 231-242.
- Braa J, Sahay S (2012) Integration and interoperability-standardization is the key. Integr Heal Inf Archit Power to User, pp. 58-82.
- IEEE (1990) Standard Computer Dictionary: A Compilation of IEEE Standard Computer Glossaries.
- Bhartiya S, Mehrotra D, Girdhar A (2016) Issues in achieving complete interoperability while sharing electronic health records. Phys Procedia 78: 192-198.
- Gaucher H (2017) Integrated health care. J Am Dent Assoc 148(3): 145.
- Bhartiya S, Mehrotra D (2014) Challenges and recommendations to healthcare data exchange in an interoperable environment. Electron J Heal Informatics 8(2): e16.
- Kouroubali A, Katehakis DG (2019) The new European interoperability framework as a facilitator of digital transformation for citizen empowerment. J Biomed Inform 94: 103166.
- Sahay S, Nielsen P, Aanestad M (2019) Institutionalizing information systems for universal health coverage in primary healthcare and the need for new forms of institutional work. Commun Assoc Inf Syst 44(1): 62-80.
- Upadhyay S, Hu H (2022) A qualitative analysis of the impact of electronic health records (EHR) on healthcare quality and safety : clinicians lived experiences. Health Serv Insights 15: 1-7.
- Shahmoradi L, Habibi-Koolaee M (2016) Integration of health information systems to promote health. Iran J Public Health 45(8): 1096-1097.
- Li E, Clarke J, Ashrafian H, Darzi A, Neves AN (2022) The impact of electronic health record interoperability on safety and quality of care in high-income countries : Systematic review. J Med Internet Res 24(9):
- Leon N, Schneider H, Daviaud E (2012) Applying a framework for assessing the health system challenges to scaling up mHealth in South Africa. BMC Med Inform Decis Mak 12: 123.
- Thompson MP, Graetz I (2019) Hospital adoption of interoperability functions. Healthcare 7(3): 100347.
- Lehne M, Sass J, Essenwanger A, Schepers J, Thun S (2019) Why digital medicine depends on interoperability. NPJ Digit Med 2(1): 79.
- Cilliers L, Katurura M (2017) A review of the implementation of electronic health record systems on the African continent. African Conf Inf Syst Technol-Cape Town, South Africa.
- Snyder H (2019) Literature review as a research methodology: An overview and guidelines. J Bus Res 104: 333-339.
- Ferrari R (2015) Writing narrative style literature reviews. Med Writ 24(4): 230-235.
- Green BN, Johnson CD, Adams A (2006) Writing narrative literature reviews for peer-reviewed journals: secrets of the trade. J Chiropr Med 5(3): 101-117.
- Baethge C, Goldbeck-Wood S, Mertens S (2009) SANRA-A scale for the quality assessment of narrative review articles. Res Integr Peer Rev 4: 5.
- O’Brien GL, Sinnott SJ, Walshe V, Mulcahy M, Byrne S (2020) Health policy triangle framework: Narrative review of the recent literature. Heal Policy OPEN 1: 100016.
- Kuziemsky C (2013) A multi-tiered perspective on healthcare interoperability. Interoperability Health Inf Syst Stand Manag Technol, pp. 1-18.
- Benson T (2010) Why interoperability is hard. London Springer, London, pp. 25-34.
- Atalag K, Kingsford D, Paton C, Warren J (2010) Putting health record interoperability standards to work. Electron J Heal Informatics 5(1): 1-17.
- (2013) HIMSS Become a Champion for Interoperability Adopt HIMSS Definition of Interoperability.
- (2017) HIMSS. HIMSS Dictionary of Health Information Technology Terms, Acronyms, and Organizations. Angewandte Chemie International Edition 6(11): 951-952.
- Sachdeva S, Bhalla S (2012) Semantic interoperability in standardized electronic health record databases. J Data Inf Qual 3(1): 1-37.
- Kobusinge G (2020) Contextual Factors influencing the design and management of health information systems’. Interoperability pp: 15-27.
- Beštek M, Stanimirović D (2017) Special topic interoperability and EHR: Combining open EHR, SNOMED, IHE, and continua as approaches to interoperability on national ehealth. Appl Clin Inform 8(3): 810-825.
- Ojeda-Carreño D, Cosío-León MA, Nieto-Hipólito JI (2017) Relevant tools for tackling interoperability problems on heterogeneous electronic health record systems: An exploratory research. Rev Mex Ing Biomed 38(1): 25-37.
- Naveed A, Sigwele T, Kamala M, Hu F (2018) Semantic interoperability, privacy and security concerns in electronic health records: survery and model proposal. Researchgate Net.
- Adel E, El-Sappagh S, Barakat S, Elmogy M (2019) Ontology-based electronic health record semantic interoperability: A survey. U-Healthcare Monitoring Systems, pp: 315-352.
- Heidenreich G, Angelidis P (2009) Six steps to electronic health records interoperability. Eur J ePractice.
- Hammami R, Bellaaj H, Kacem AH (2014) Interoperability of healthcare information systems.
- Adel E, El-Sappagh S, Barakat S, Elmogy M (2019) A unified fuzzy ontology for distributed electronic health record semantic interoperability. In: U-Healthcare Monitoring Systems. Elsevier, pp. 353-395.
- Almeida MSC, Filho LF de S, Rabello PM, Santiago BM (2020) International classification of diseases – 11th revision: from design to implementation. Rev Saude Publica 54(104):
- Frisse ME (2017) Chapter 5 - Interoperability. Key Advances in Clinical Informatics, pp. 69-77.
- Hammond WE (2018) How do you know when you have interoperability? Eur J Biomed Informatics 14(3): 13-20.
- Naveed A, Sigwele T, Hu YF, Kamala M, Susanto M (2018) Addressing semantic interoperability, privacy and security concerns in electronic health records. Journal of Engineering and Scientific Research 2(1): 31-38.
- Janaswamy S, Kent RD (2016) Semantic interoperability and data mapping in EHR systems. 2016 IEEE 6th International Conference on Advanced Computing (IACC),
- Legg M (2014) Standardization of test requesting and reporting for the electronic health record. Clin Chim Acta 432: 148-156.
- Adel E, El-Sappagh S, Barakat S, Elmogy M (2018) Distributed electronic health record based on semantic interoperability using fuzzy ontology: A survey. Int J Comput Appl 40(4): 223-241.
- Gomes F, Freitas R, Ribeiro M, Moura C, Andrade O, et al. (2019) GIRLS, a gateway for interoperability of electronic health record in low-cost system: Interoperability beetween FHIR and Open EHR Standards. 2019 IEEE International Conference on E-health Networking, Application & Services (HealthCom), Colombia, South America.
- Othman MH, Razali R (2017) Electronic government systems interoperability model. J Telecommun Electron Comput Eng 9(3-4): 1-9.
- Juzwishin DWM (2009) Political, policy and social barriers to health system interoperability: Emerging opportunities of Web 2.0 and 3.0. Healthc Manag Forum 22(4).
- Udjlü HRQ, Rydþ U, Gdqrylü DYR (2015) Overcoming e-health interoperability obstacles: integrating PHR and EHR using HL7 CCD pp. 28-30.
- Azarm-Daigle M, Kuziemsky C, Peyton L (2015) A review of cross organizational healthcare data sharing. Procedia Comput Sci 63: 425-32.
- Balka E, Whitehouse S, Coates ST, Andrusiek D (2012) Ski hill injuries and ghost charts: Socio- technical issues in achieving e-Health interoperability across jurisdictions. Inf Syst Front 14(1): 19-42.
- Lowi TJ (1972) Four systems of policy, politics, and choice public administration review. American Society for Public Administration. Public Adm Rev 32(4): 298-310.
- Barbarito F, Pinciroli F, Mason J, Marceglia S, Mazzola L, et al. (2012) Implementing standards for the interoperability among healthcare providers in the public regionalized healthcare information system of the Lombardy region. J Biomed Inform 45(4): 736-745.
- Botts N, Bouhaddou O, Bennett J, Pan E, Byrne C, et al. (2014) Data quality and interoperability challenges for ehealth exchange participants: observations from the department of veterans affairs’ virtual lifetime electronic record health pilot phase. AMIA Annu Symp Proc pp. 307-314.
- Soceanu A, Egner A, Moldoveanu F (2013) Towards interoperability of ehealth system networked components. pp. 147-154.
- Tao C, Bouamrane MM (2012) Managing interoperability and complexity in health systems - MIXHS’12. Proc 21st ACM Int Conf Inf Knowl Manag - CIKM’12 pp. 2758-2759.
© 2024 Neema Mkayula. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






