- Submissions

Full Text
Trends in Telemedicine & E-health
Development of Cognitive Intervention Program (CIP) in Young Adults with Symptoms of Depression and Neurocognitive Impairments
Neethu George* and Rosalito De Guzman
University of Santo Tomas, Philippines
*Corresponding author:Neethu George, The Graduate School, University of Santo Tomas, Manila, Philippines
Submission: November 03, 2023; Published: November 28, 2023

ISSN: 2689-2707 Volume 4 Issue 4
Abstract
Depression is a significant issue among young adults, with a noticeable rise in depressive symptoms. This study aims to outline the creation and application of the Cognitive Intervention Program (CIP) for young adults, designed to diminish depression and improve cognitive functions. This innovative psychotherapy combines Rational Emotive Behavior Therapy (REBT) to address irrational beliefs and teach healthier emotional and cognitive management, along with Cognitive Remediation Therapy (CRT) which involves repeated practice in cognitive skills through computer or paper exercises. The research used qualitative (interviews), quantitative (surveys), and mixed methods to gain a comprehensive understanding. The program, developed by combining empirical findings, theoretical models, and existing facts, consists of seven detailed modules. After implementation and evaluation, the Cognitive Intervention Program proved successful in reducing depression and enhancing cognitive functions in young adults.
Keywords: Depression; CIP; REBT; CRT; Young adults
Introduction
Depression is a significant public health issue with broad negative effects on various aspects of life, and its prevalence is extensive. The incidence of these conditions rose among adults in the years preceding the COVID era, with young adults exhibiting the highest rates among all age groups and experiencing a greater increase compared to older adults [1,2]. In 2019, approximately 21% displayed symptoms of depression. The well-established repercussions of untreated mental health conditions on overall health and well-being are documented in both the short and long term [3]. Neurocognitive impairments are a fundamental characteristic of depression in adults. Recently, there has been growing acknowledgment of neurocognitive deficits in young adults grappling with depression [4]. Other disorders have exhibited distinctive functional outcomes with varying predictors, delving into cognition as encompassing thoughts’ content, dysfunctional attitudes and beliefs about oneself, and cognitive processes, including neurocognitive abilities in areas such as memory, attention, and executive functioning [5].
Moreover, cognitive impairments are not an artifact of motivation or other depressive symptoms; they endure even during remission, with as many as half of remitted depressed patients displaying ongoing cognitive deficits [6]. Despite achieving clinical remission, individuals with mental disorders often fall short of reaching their anticipated or pre-illness levels of social and occupational functioning, indicating the presence of persistent factors hindering functional recovery. Neurocognitive impairment is one such factor, manifesting early in the course of depressive disorder [7]. Due to resource constraints, the wait times for psychotherapy are frequently lengthy, posing a challenge for those in need of treatment and the healthcare system. To bridge the gap between initial contact and the commencement of psychotherapy, web-based interventions can be employed. The introduction of a web based intervention for depression during waiting periods has the potential to alleviate depressive symptoms and improve neurocognitive functions in individuals awaiting psychotherapy [8]. There is currently a lack of evidence-based online interventions during public health crises [9].
Method
Design
This research adhered to Conklin’s (1997) model for program development, encompassing planning, design, implementation, and evaluation stages. By adopting Conklin’s program development model, the study enhanced program relevance, enabling a focused allocation of resources to address the most pressing and current needs of a large population. The initial phase involved planning, which included establishing program goals, conducting a needs assessment, prioritizing program elements, identifying target audiences, formulating program objectives based on an extensive review of relevant literature, and analyzing data from surveys, interviews, and focus group discussions with the target populations. The subsequent phase centered on designing and implementing the CIP Intervention Program, involving the selection and development of content, choosing or creating delivery methods and resource materials, and establishing an implementation timeline. The final phase encompassed the evaluation and validation of the program’s effectiveness in targeting the selected young adults exposed to the CIP [10].
Participants
The study randomly chose college students who met specific criteria, including symptoms of depression, moderate rumination scores, memory failures, and moderate scores on the Attentional Network Test reaction time. Selection was based on the following inclusion criteria: 1. Being young college students aged between 18 and 25, 2. Proficiency in understanding the English language, 3.
Willingness to participate in the study, 4. Not currently undergoing psychotherapy or using relaxation techniques, and 5. Absence of other chronic physical or mental health issues. Additionally, participants were required to not have Major Depressive Disorder (MDD).
Instruments
A. Information Sheet: The researcher created a demographic questionnaire as a personal data sheet, serving as a crucial tool for obtaining sociodemographic information from respondents. These datasheets played a vital role in gathering relevant data, guiding the inclusion and exclusion criteria for participants.
B. The Beck Depression Inventory (BDI-II): A 21-item self-report scale developed by Lee & Colleagues [11], was utilized to assess the severity of depression symptoms.
C. Ruminative response Scale (RRS-SF): The Short version of the Ruminative Response Scale (RRS-SF), designed by Treynor and colleagues, is a self-report scale using a four-point Likert scale to assign scores to items, as outlined by [12],
D. The Prospective and Retrospective Memory Questionnaire (PRMQ): Gauged the frequency of memory problems in daily life on a scale from 1 (“never”) to 5 (“very often”), following the design by Sheppard et al. [13].
E. The Attention Network Test (ANT): Employed in this study involved a flanker task with arrows and a cued reaction time task. This investigation explored how cues and targets influenced the alerting, orienting, and executive control networks—crucial components of attention-using a single reaction time task, as described by Fu et al. (2017) [14].
Procedures
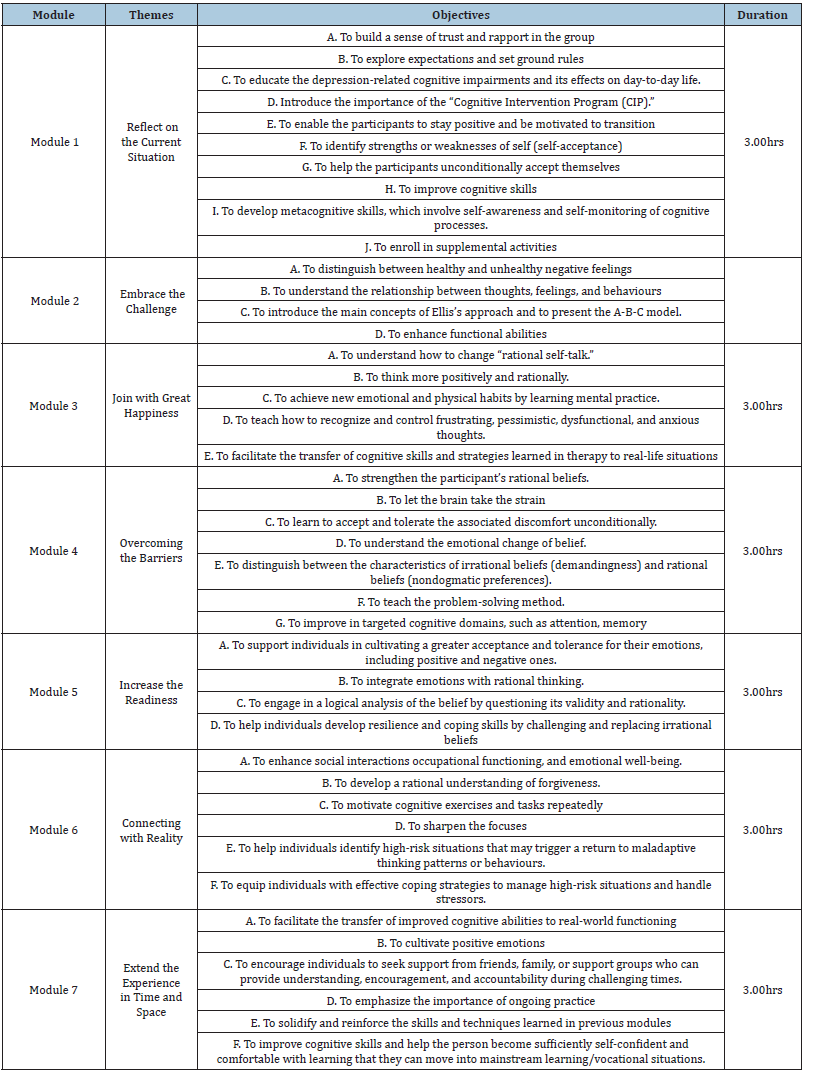
Table 1 shows the outline of the Outline of the Modules of the CIP.
Table 1:Cognitive Intervention Program.
The process of collecting data was structured into three phases: pre-experimental, experimental, and post-experimental.
A. In the pre-experimental phase: The initial step involved developing the Cognitive Intervention Program. This process entailed an extensive review of literature and existing treatment programs in the relevant field. The aim was to contribute uniquely to the field of clinical psychology by integrating elements of neuroscience and principles from Rational Emotive Behavior Therapy, with a primary focus on alleviating symptoms of depression and enhancing neurocognitive functions in young adults. Subsequently, the researcher collaborated with school principals and teachers. Discussions were held with the director to ensure the effective implementation of the study. The researcher then sent a letter explaining the study and the significance of the intervention program to the colleges. Upon obtaining permission, coordination was established with the teachers to ensure the study’s successful execution.
B. Experimental Phase: Adhering to ethical research principles, the researcher ensured equal treatment of both the experimental group and control group. One week following the pre-test, the cognitive intervention program was initiated for the experimental group, while the control group remained unexposed to the program. The intervention spanned seven weeks, comprising seven modules, each lasting 45 minutes. Each module included a session primarily focused on Albert Ellis’s Rational Emotive Behavior Therapy (REBT) theory (Turner, 2016) [15], along with an explanation of Cognitive Remediation Therapy (CRT) principles. CRT involves techniques aimed at teaching thinking skills and can be viewed as a type of cognitive rehabilitation.
C. Post-Experimental Phase: One week after concluding the intervention program, the researcher conducted a post test for both groups, employing similar protocols to measure differences and explore potential cause-and-effect relationships between the Cognitive Intervention Program and improvements in neurocognitive functions based on the Attention Network Test (ANT). The assessment involved subjecting pre-intervention and post-intervention scores to statistical analysis to identify significant differences.
Result and Discussion
The Structure of the Cognitive Intervention Program: The Cognitive Intervention Program spans seven weeks and is designed to reduce depression and enhance neurocognitive functions in young adults. Comprising seven modules, each lasting 45 minutes, the program includes sessions primarily focused on Albert Ellis’s Rational Emotive Behaviour Therapy (REBT) Theory [15] and an explanation of Cognitive Remediation Therapy (CRT) principles. The researcher crafted the program with the goal of imparting the fundamental tenets of REBT and CRT, employing various tasks facilitated by the THINC-it tool-an assessment tool for cognitive functions--Brain HQ, a brain training program developed by Posit Science, and Neuro Nation, a brain training app.
Conclusion
Despite certain limitations, the results indicate that the combination of REBT with CRT principles is highly successful in improving neurocognitive functions. The significant difference in post-test scores between the experimental and control groups underscores the effectiveness of the researcher-designed intervention program in enhancing neurocognitive functions. Moreover, the substantial difference in mean scores between the pre-test and post-test for the experimental group demonstrates the intervention program’s remarkable efficacy in alleviating cognitive impairments in young adults. The effectiveness of this study suggests that the newly developed Cognitive Intervention Program can serve as a valuable tool for enhancing neurocognitive functions.
Acknowledgment
The author(s) express(es) gratitude to the participants of the study and those who contributed to facilitating the research process.
Statement of Ethics
The study, assigned protocol code GS2022-022, underwent review and approval by the UST Graduate School Review Ethics Committee (USTGS-REC).
References
- Renee DG, Andrea HW, June HK, Melody Wu, Sandro Galea, et al. (2020) Trends in anxiety among adults in the United States, 2008-2018: Rapid increases among young adults. Journal of Psychiatric Research 130: 441-446.
- Jean M Twenge, A Bell Cooper, Thomas E Joiner, Mary E Duffy, Sarah G Binau, et al. (2019) Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005-2017. Journal of Abnormal Psychology 128(3): 185-199.
- Sally H Adams, Jason P Schaub, Jason M Nagata, M Jane Park, Claire D Brindis, et al. (2022) Young Adult Anxiety or Depressive Symptoms and Mental Health Service Utilization During the COVID-19 Pandemic. Journal of Adolescent Health 70(6): 985-988.
- Catherine MN, Lisa J Phillips, Shayden Bryce, Sarah Hetrick, Andrea L Wright, et al. (2019) Subjective experiences of neurocognitive functioning in young people with major depression. BMC Psychiatry 19(1): 209.
- Chelsea WR, Tanya T, Melissa M, Ruzica J, Roumen M, et al. (2023) Neurocognition and depressive symptoms have unique pathways to predicting different domains of functioning in major depressive disorder. Can J Psychiatry 68(4): 241-248.
- Julie G, Philippe B, Simon G, Martin FL (2012) Psychosocial and neurocognitive functioning in unipolar and bipolar depression: A 12-month prospective study. Psychiatry Research 196(1): 145-153.
- Jacob J Crouse, Kate M Chitty, Frank Iorfino, Joanne S Carpenter, Django White, et al. (2020) Modelling associations between neurocognition and functional course in young people with emerging mental disorders: A longitudinal cohort study. Transl Psychiatry 10(1): 22.
- Sasha DG, Harald B, Jürgen B, David E, Lena K, et al. (2018) Effectiveness and acceptance of a web-based depression intervention during waiting time for outpatient psychotherapy: Study protocol for a randomized controlled trial. Trials 19(1): 285.
- Christian R, Anita S, Dusan H, Andreas S, Isabell P, et al. (2021) Evidence synthesis of digital interventions to mitigate the negative impact of the COVID-19 pandemic on public mental health: Rapid meta-review. J Med Internet Res 23(3): e23365.
- Franz N, Garst B, Gagnon R (2015) The Cooperative extension program development model: Adapting to a Changing Context. Journal of Human Sciences and Extension 3: 3.
- Kounseok Lee, Daeho Kim, Yongrae Cho (2018) Exploratory factor analysis of the beck anxiety inventory and the beck depression inventory-ii in a psychiatric outpatient population. J Korean Med Sci 33(16): e128.
- Lilla NK, Natália K, Attila G, Anna M, Zsolt D, et al. (2021) Validating the bifactor structure of the ruminative thought style questionnaire--A psychometric study. PLOS ONE 16(7): e0254986.
- David PS, Matthew WG, Erin EM, Angulique YO, Sylvie N, et al. (2022) “Do I Have a Memory Problem? I Can’t Recall”: An evaluation of measurement invariance in subjective reporting of memory symptoms among persons with and without objective HIV-associated memory impairment. J Int Neuropsychol Soc 28(2): 166-176.
- Jia F, Peng X, Lun Z, Guoming Y (2018) Impaired orienting in youth with internet addiction: Evidence from the Attention Network Task (ANT). Psychiatry Res 264: 54-57.
- Martin JT (2016) Rational Emotive Behavior Therapy (REBT), irrational and rational beliefs, and the mental health of athletes. Frontiers in Psychology 7: 1423.
© 2023 Neethu George. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






