- Submissions

Full Text
Trends in Telemedicine & E-health
Need for Navigators for Care of Patients with Diabetes in Rural, Underserved Areas
Richard J Santen*
Division of Endocrinology and Metabolism, University of Virginia Health Care System, USA
*Corresponding author: Richard J Santen, Professor Emeritus, Division of Endocrinology and Metabolism, University of Virginia Health Care System, Charlottesville, Virginia, USA
Submission: April 22, 2022; Published: May 02, 2022

ISSN: 2689-2707 Volume 3 Issue 3
Opinion
This opinion piece will provide the background and rationale why navigators are needed for the care of patients with diabetes living in rural, underserved areas and who are utilizing telehealth and its requisite technology. My experience with 280 rurally-based patients with diabetes over the last five years has uncovered multiple problems with utilization of technology. This has been difficult for my patients and clinical staff to handle. This experience has raised the concept that an experienced and highly trained troubleshooter (Navigator) could assist the clinical staff and patients and enable more effective utilization of multiple technological components of telehealth programs. Patients with diabetes living in rural, underserved areas in the United States encounter several difficulties regarding effective management of their glucose levels and relevant co-morbidities. The major factors involved include: barriers to health care access and education; long travel distances; lack of public transportation; financial challenges in paying for professional fees and prescriptions; and communication difficulties due to lack of internet coverage [1]. An additional problem is the workforce gap in endocrinologists available to provide specialty care for patients with diabetes. Studies indicate a workforce gap of approximately 1500 Endocrinologists in the United States overall but this gap is particularly exaggerated in rural areas [2].
One solution to this problem is the extensive use of technology to enlist the participation of endocrinologists practicing at distant sites to provide specialty expertise. Telehealth with all of its components provides a means for endocrinologists practicing in urban areas to care for patients living at distant, rural , underserved areas [3]. Several key components to facilitate this specialty care can be accomplished by telehealth and associated technological components. Teaching of the principles underlying diabetes and nutrition can be effectively accomplished by telemedicine with one-on-one interactions between the patient and certified diabetes educator. Glucose levels can be obtained with continuous monitoring devices or with non-finger stick devises such as the libre 2 and these data can be transmitted via the cloud. Use of algorithms to determine insulin doses such as the Glucomander-outpatient system facilitates therapeutic dose-decision making. Weight scales and blood pressure cuffs linked to the internet can provide important data to the endocrinologist working at distant sites. As compliance is a major issue in management, “smart insulin pens” are now available which record usage of insulin electronically and transmit this information to the internet. A novel means of education is to provide “meal replacements” to patients, as these give examples of calorie and carbohydrate control. Subjective assessment of compliance can monitored via telephone or telemedicine.
The major problem in implementing each of these components is the lack of understanding and experience of patients in the use of this technology, particularly in groups of patients with limited education. Clinic staff also struggle with the intricacies of multiple platforms and devices. In our experience, patients have difficulty setting up the transfer of glucose data to their smart phones, computers or cloud. The sensors are often not placed properly or become inoperable prior to their 10 to 14 day expiration period and assistance is needed. Use of electronic scales often results in difficulties with transmission of data. Connections with the internet are often intermittent and subject to equipment problems. One practical solution to these problems is to hire navigators. Notably, the issue of hiring navigators to troubleshoot and solve these problems came up as a major topic of discussion at a recent White House Conference. The White House Office of Science and Technology Policy (OSTP) recently convened a virtual meeting entitled “Community Connected Health Initiatives” in order to discuss the problems encountered across the country with the care of patients in underserved areas. Part 1, held on February 3, 2022 addressed “Innovation with Community Health Organizations and Providers” [4]. As a participant, I raised the concept during the discussion that there was a critical need for “navigators”. These would be individuals with technological expertise to assist patients and clinical staff in managing all of the various components of technology. The navigators would be particularly important in the Telehealth care of patients with diabetes in rural, underserved areas. This suggestion was widely discussed by participants from several areas of the country and from various types of clinic setting. The concept was then widely agreed upon that a highly trained navigator would serve to solve many of the technological issue that arise with patients.
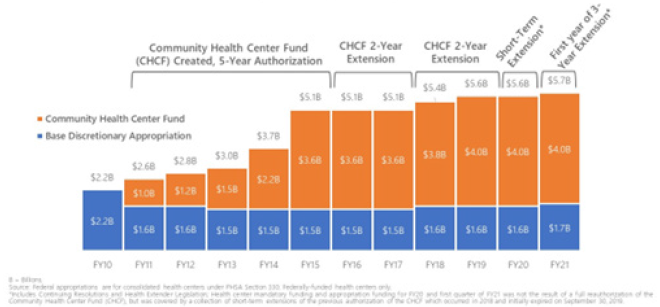
The White House meeting focused on one component of the Federal Health System which best could provide care for patients with diabetes in rural, underserved areas and could most benefit from navigators. This involved the Federally Qualified Community Care System (FQCHCS). There are 1368 clinics in the United States with formal FQCHC status [4]. These clinics handled 29,000,000 total patient visits last year. The five largest clinics in the USA had 2,318, 048 patient visits in 2020. The funding for the FQCHC program has grown from 2.28 billion dollars in 2010 to 5.78 billion in 2021 (Figure 1). The program requires the following elements for certification as a FQCHC:
Figure 1:Federal health center federal appropriation and mandatory funding history, FY10-FY21.
i. Provision of comprehensive primary and preventative
care
ii. Patients cared for regardless of ability to pay or health
insurance status
iii. Enhanced reimbursement for Medicare and Medicaid
iv. Must serve an underserved area or population;
v. Sliding scale fees
vi. Have ongoing quality assurance program
vii. Have a governing board of directors composed primarily
of patients
viii. Be a non-profit or public organization. Because of
emphasis and funding, these clinics provide an important
resource for care of patients with diabetes, use of telehealth,
and need for navigators.
An example presented at the virtual White House meeting was a program with approximately 30 clinics serving West Virginia and Arkansas. With such a centrally administered series of clinics, one navigator should be able to use telemedicine to educate patients and personnel about the technology and to troubleshoot when technical problems arose. This would be a much more efficient means of handing difficulties than having non-trained patients and personnel contact the various technology companies. My own experience has convinced me of the potential utility of hiring navigators. As an academic endocrinologist, I have been supported over several years in an unequaled way by navigators guiding me through the process of obtaining Institutional Review Board approval for clinical research projects. My current activity is to serve as the Endocrinology specialist for five FQCHCs. I have experienced firsthand, the difficulties with utilization of continuous glucose monitors, the glucomander-outpatient system for decision making about insulin, and the use of electronic scales and blood pressure cuffs. This has supported my strong opinion that navigators are urgently needed in the FQCHC system and that such experts would enable improved care in a cost effective fashion. I have written this opinion article in order to convince others to figure out ways of funding navigators for this purpose.
References
- Ross S, Benavides-Vaello S, Schumann L, Haberman M (2015) Issues that impact type-2 diabetes self-management in rural communities. Journal of the American Association of Nurse Practitioners 27(11): 653-660.
- Vigersky RA, Fish L, Hogan P, Stewart A, Kutler S, et al. (2014) The clinical endocrinology workforce: current status and future projections of supply and demand. Journal of Clinical Endocrinology & Metabolism 99(9): 3112-3121.
- Santen RJ (2019) Re-booting" after retirement: Novel approach using telemedicine to solve the work-force gap in diabetes management. Maturitas 133: 68-69.
- (2022) Community Connected Health Initiative Roundtable Series. HRSA Center for innovation.
- You Tube video of Conference.
- How many Federally Qualified Health Centers are there?
© 2022 Richard J Santen. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






