- Submissions

Full Text
Trends in Telemedicine & E-health
Use of Telemedicine During the Second Covid Pandemic Wave of October 2020 in a Tertiary Referral Hospital in Switzerland
Emmanuel Haefliger*, Philipp Suter, Gael Grandmaison and Daniel Ha
Department of Internal Medicine, Switzerland
*Corresponding author: Emmanuel Haefliger, Department of Internal Medicine, Boarding school path 2-6, 1708 Fribourg, Switzerland
Submission: April 8, 2022; Published: April 25, 2022

ISSN: 2689-2707 Volume 3 Issue 3
Abstract
Covid-19 posed major problems for health systems and hospitals, which suddenly had to deal with significantly larger patient flows. Each hospital has responded differently, with telemedicine proving a viable option. Patients were discharged earlier and further monitored by telemedicine; the emergency departments used telemedicine as a triage tool, or consultations were conducted via telemedicine applications. We conducted a retrospective descriptive study analyzing the satisfaction of telemedicine follow-ups of COVID-19 positive patients discharged from hospitalization. Physicians followed up the 24 patients via telemedicine, and 21 questionnaires were completed and analyzed, based on the total of 55 performed consultations. In general, the patients were delighted with the follow-up quality and found this consultation pleasant. The patients would also recommend the telemedicine service to others and want to use this service more often in the future. However, from an outpatient perspective, it remains to be seen whether telemedicine offers the real added value of reducing hospital costs and length of stay.
Keywords: Telemedicine; Second covid; Health systems; Hospitals; Triage tool; Physicians; Pneumonia
Abbreviations: WHO: World Health Organization; HFR: Hospitals of Fribourg; HR: Heart Rate; SBP: Systolic Blood Pressure
Introduction
Since the first description of novel coronavirus pneumonia was reported in Wuhan in December 2019, COVID-19 has spread rapidly worldwide [1] (Figure 1). The emergent virus quickly represented a massive challenge for the health systems worldwide due to the massive influx of patients to hospital facilities with a massive shortage of inpatient beds in acute medicine [2]. This exceptional situation required rapid adaptations and innovative solutions to ensure appropriate and new patient care forms and sufficient hospital beds [3]. A rapid transition of inpatient to outpatient care is one of the possibilities to relieve pressure on hospital facilities. As this transition represents a hazardous period, it was important to develop strategies for adequate monitoring of patients after discharge from the hospital to guarantee their safety and subsequent treatment.
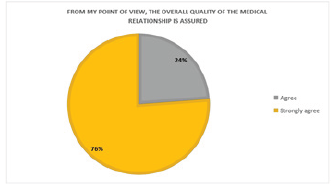
Figure 1:Quality of the medical relationship.
WHO defines telemedicine as “The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities” (WHO. A health telematics policy in support of WHO’s Health- For-All strategy for global health development: report of the WHO group consultation on health telematics, 11–16 December, Geneva, 1997. Geneva, World Health Organization, 1998.) One of the main advantages of telemedicine includes the possibility of consulting at a distance and avoiding displacement to the physician, particularly for people with reduced mobility [4]. At the same time, telemedicine enabled to ensure the safety of patients and health professionals by avoiding unnecessary exposure to infectious diseases in addition to limiting the spread of the virus [4]. During this epidemic, telemedicine was used in many ways, particularly for initial triage of infected patients, monitoring patients treated on an outpatient basis but at risk of worsening [5] or proposing a “hospital-athome” strategy. This approach allows adapted care at home by a specialized nurse and intensive medical monitoring using various telecommunication tools [6]. Telemedicine also enables patients to be monitored at the end of hospitalization, transitioning from being taken in charge by the attending primary care physician. Indeed, well-selected patients requiring close monitoring or gradual weaning from oxygen therapy can be monitored closely after discharge from the hospital.
At the end of October 2020, during the second wave of COVID-19 patients, the Hospitals of Fribourg (HFR) were confronted with a rapid increase in the number of hospitalizations. In this context, the different departments reorganized themselves to maximize their bed capacity and health care workers. To facilitate the transition of fragile patients to outpatient care, a telemedicine service was set up to ensure close monitoring of these patients while limiting the displacement of patients who are still potentially contagious. Although many studies and reviews analyzed the use and implementation of telemedicine [7], relatively few studies in comparison have looked at the satisfaction of patients followed by telemedicine [8,9]. This review aims to study the patient experience and satisfaction with telemedicine post-hospital follow-up.
Method
Design of the study
We performed a retrospective descriptive study evaluating the satisfaction of patients who received telemedicine follow-up in the context of the COVID-19 pandemic. The data were obtained from questionnaires completed by patients who benefited from this service between 05.11.2020 and 10.12.2020.
Recruitment of participants
All patients included in this analysis consulted our hospital for an acute COVID-19 infection documented by RT-PCR on a nasopharyngeal swab and received a minimum of one follow-up consultation via telemedicine. The medical criteria required for ambulatory telemedicine follow-up included: stability of vital parameters for 24 hours (heart rate (HR)<100/min and systolic blood pressure (SBP) >90mmHg and respiratory rate (RR)<24/ min); body temperature below 39 °C; a general condition allowing autonomy at home, with the addition of home-based care service if indicated, and the possibility of a return to the emergency room if necessary. The new instauration of oxygen home-therapy after COVID-19 hospitalization did not contraindicate follow-up by telemedicine.
Telemedicine team
A medical team linked to our internal medicine department provided the ambulatory follow-up. It consisted of a pool of 2 doctors, nurses in training and IT and logistical support.
Medical material
The equipment available at each consultation included a Tytocare connected stethoscope (copyright), a blood pressure monitor, a pulse oximeter, a wifi terminal, blood and urine sampling equipment and a touchpad.
Consultation process
The consultations took place at the patients’ homes, guided by a nurse. After initial contact and a nursing consultation, including measuring the vital parameters, a live-streaming video connection was established with the consulting physician. The direct interaction between the patient and the doctor allowed a targeted history and clinical examination via the nurse. In this regard, the doctor could obtain further examinations, like blood or urine samples. A follow-up consultation was organized depending on the evolution since discharge and the medical assessment. In case of emergency, patients could contact the telemedicine team directly to arrange a telemedicine consultation or to be referred to our emergency service.
Data collection
The patients’ medical data were extracted from the digital patient file established during the hospitalization. After the last telemedicine consultation, each patient received a link to an online satisfaction questionnaire. The consulting physicians received a questionnaire at the end of each consultation. These forms were completed independently and anonymously by all participants. The questionnaires can be consulted in the appendix (see supplement 1).
Data Collection
Fifty-five medical consultations were performed in 24 patients. Out of them, four patients had one consultation, 13 patients had two consultations, four patients had three consultations, two patients had four consultations, and one patient had five consultations. Twenty-one (87.5%) patients completed the questionnaire at their last consultation, based on all their received consultations.
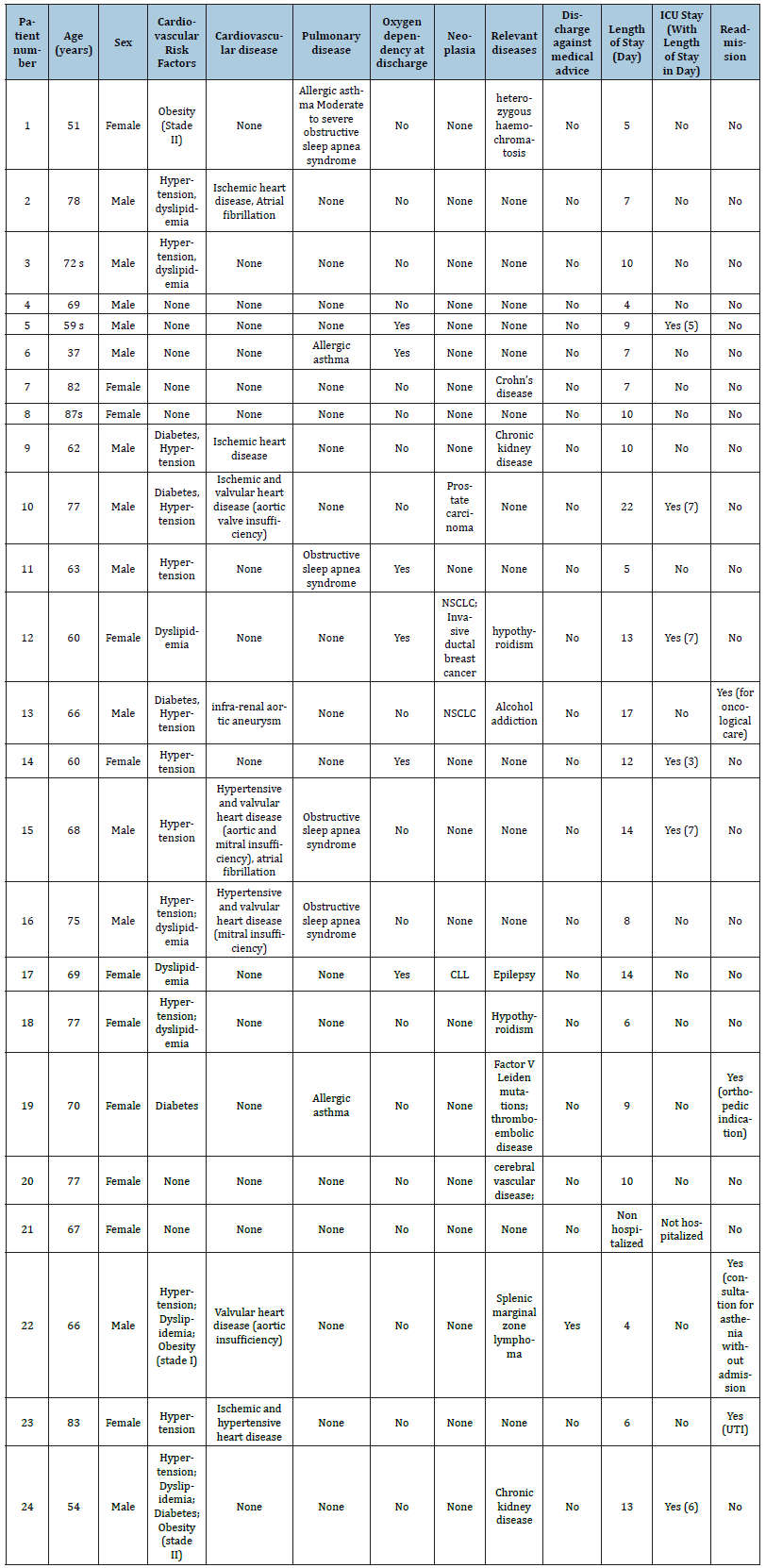
Table 1:Average patient characteristics.

Of the 24 patients followed in telemedicine, 13 (54.2%) were male and 11 (45.8%) female. The average age of the patients was 67.9 years (+/- 11.3 years). All patients were initially hospitalized in our internal medicine department, except one patient who was managed as an outpatient with follow-up via telemedicine, initially addressed by the emergency service. It should be noted that one patient left the hospital against medical advice. This patient did not meet the safety criteria. He was nevertheless followed up via telemedicine to ensure follow-up and safety. The average characteristics are summarized in (Table 1). The characteristics of each patient are summarized in the appendix (see supplement 2).
Patient data
Figure 2:Patient’s expectations regarding doctors.
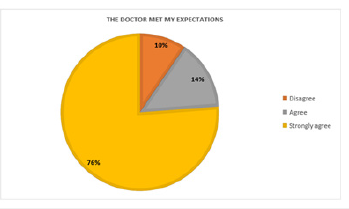
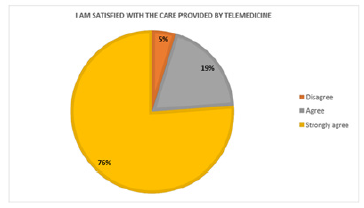
All patients noted that telemedicine provided a good human relationship between doctors and patients. Most patients (90%) mentioned that the doctor met their expectations (Figure 2). The majority of patients (95%) reported feeling generally safe during the consultation (Figure 3). Twenty patients (95%) responded that they felt confident during the medical treatment (Figure 4). The majority of patients (95.2%) mentioned that telemedicine made them gain comfort, while 90.5% of patients agreed that telemedicine made them gain time. Compared with an office consultation, most patients judged the medical care to be good to very good (86%) (Figure 5). The same proportions of responses were found concerning the quality of the relationship with the doctor (Figure 6). Almost all patients (95%) were satisfied with the care provided by telemedicine. About 90% of the patients responded that they were satisfied with the doctor’s care. The majority of patients (90%) said that they would more frequently use the telemedicine service in the future and would recommend it to others (Table 2).
Figure 3:Feeling of safety.
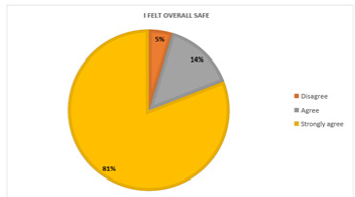
Figure 4:Feeling of confidence.
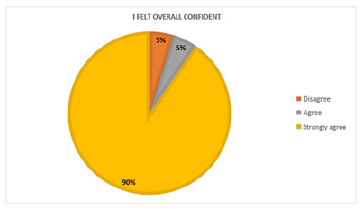
Figure 5:Comparison with an office consultation.

Table 2:patients’ characteristic.
Discussion
Figure 6:Quality of the relationship with the doctors.
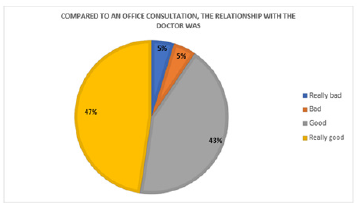
Since the emergence of telemedicine in the last few years, its use has mainly been studied in the management of chronic diseases such as heart failure [10], chronic and acute respiratory diseases [11-13] or diabetes [14]. This study aimed to analyze the possibilities of using telemedicine in the transition phase between hospitalization and discharge. The different results obtained tend to show a high general satisfaction in our cohort. From the patients’ point of view, many declared themselves satisfied with the relationship they developed with the doctor and generally felt confident and safe. There was a high level of satisfaction with the care offered by telemedicine (Figure 7). Most of the patients stated that they would like to use the telemedicine service more often and would recommend this service to their family and friends. Compared to a traditional consultation, it is also interesting to note that the patients were highly satisfied with the administrated medical care. The possibility for elderly patients with numerous comorbidities to consult at home without travelling seems to represent an undeniable gain in time and comfort. Our consulting doctors felt that their care had been effective and of good quality, that the distance had not interfered with their clinical and physical assessment and that they were satisfied with the consultation method. It is interesting to note that the medical degree of the situations was considered difficult to very difficult in almost one-third of the consultations and that, in comparison with a consultation, in a general practitioner office, the doctors considered that in a quarter of the consultations their administered care was less satisfying. The reasons for these difficulties were not developed in our questionnaire and prevented us from objectively identifying the reasons. However, the consulting doctors reported that the medical difficulties had mainly been generated by technical problems, including video and sound cuts and difficulties in establishing a connection. However, the intrinsic medical difficulty was not higher than in the office with a representative population of patients seen in general internal medicine consultations. In the end, we assume that the main difficulties encountered were due to logistical difficulties which need to be corrected in order to improve further care by telemedicine
Figure 7:Satisfaction provided by telemedicine.
During this pandemic, general practitioners did a great work by monitoring possible critically-ill patients on an outpatient basis and at discharge from the hospital. However, due to the heavy workload, the age of some practitioners at risk and the quarantine of health professionals, this follow-up could not always be carried out [15]. This analysis shows that telemedicine can provide perceived adequate care during the transition phase between the hospital and the ambulatory environment, a particularly highrisk phase for some patients. It is interesting to note that only four patients had emergency consultations or were readmitted at six months. Of these patients, three were readmitted for medical indications other than COVID-19 infection. Only one, more precisely the one discharged against medical advice, consulted the emergency room because of asthenia in the context of COVID, without any resulting hospitalization. The values obtained are similar to the hospitalization rates of two studies carried out in Spain, where 6% and 8% respectively of the patients monitored by telemedicine had to be hospitalized [5,16]. Telemedicine, although requiring the travel of a health worker, thus makes it possible to protect consulting physicians at risk of severe infection while allowing them to continue to assume their workload, even when they are in quarantine [15,17]. This system allowed us to include a retired doctor in our consultation team who could carry out remote consultations. In addition, it limits the movement of patients who are still potentially contagious and reduces the risk of viral spreading. The consulting doctors mentioned a very comfortable consultation mode, which permits also ensuring a high-quality follow-up of this particular patient group after an acute hospitalization.
Figure 8:Satisfaction with doctor’s care.

Figure 9:Future use of telemedicine services.
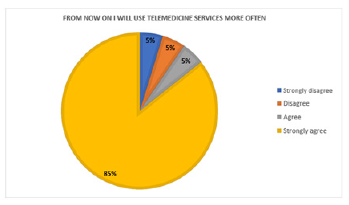
From a financial point of view, telemedicine has long been seen as a promising tool with the potential of reducing the direct and indirect costs associated with consultations by reducing intermediaries and avoiding travel costs and decreasing of professional productivity of patients while increasing their satisfaction [7] (Figure 8). However, there is a lack of quality randomized studies to demonstrate this economic gain. A Japanese systematic review [18] showed encouraging results, particularly in the management of palliative and geriatric patients. Although a Spanish study [19] on the length of stay of geriatric patients showed no difference between hospital and home care, other studies have shown that care by telemedicine reduces the number of rehospitalizations and emergency consultations [20,21]. Further studies are needed to determine whether the costs of telemedicine are sustainable and whether it significantly reduces the length of stay and readmission. In addition, it remains to be determined whether the patient selection criteria have made it possible to select patients who really need close monitoring (for example, patients who have refused treatment such as rehabilitation or a short stay, usual contacts in quarantine, fragile patients) or whether they have resulted in the selection of stable patients for whom telemedicine was in fact unnecessary. Interestingly, a quarter of the selected patients were newly receiving oxygen therapy prescribed during hospitalization. Thanks to telemedicine, this subgroup of patients could likely be discharged early from the hospital with safety and financial gain and a reduction in length of stay [20] and a reduction in patient overload in our internal medicine department and rehabilitation ward [5] (Figure 9).
Limitations
There are several limitations to the data analysis quality in this work. First, the group’s relatively small size only allows us to identify a trend. In addition, the questionnaire submitted to the participants includes an element of interpretation complicating its analysis.
Conclusion
Figure 10:Recommendation of telemedicine.

To our knowledge, this is the first Swiss study of ambulatory telemedicine follow-up of patients discharged from hospital. Other applications linked to telemedicine have not been evaluated in this study. These include the possibility of remote consultations by specialists [22] or medical triage in emergencies [23] (Figure 10). First, there is great satisfaction on the part of doctors and patients (Telemedicine offers a pleasant mode of consultation that limits contact between potentially contagious patients and health personnel at risk. It provides additional security in the transition phase between hospital and outpatient settings and allows for appropriate medical management, especially if the treating physician cannot assess the patient quickly. However, from an outpatient perspective, it remains to be seen whether telemedicine offers real added value of reducing hospital costs and length of stay. Further studies are also needed to assess telemedicine care’s safety and quality profile.
Ethical consideration
Our institutional review board approved this study. As a quality control study, this analysis did not require approval by the ethics committee. All participants signed an institutional personal medical data use consent form. The authors declare that there is no conflict of interest.
References
- Zhu N, Zhang D, Wang W, Li X, Yang B, et al. (2020) A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 382(8):727-733.
- Pellaud C, Grandmaison G Thien HPPH, Baumberger M, Carrel G, et al. (2020) Characteristics, comorbidities, 30-day outcome and in-hospital mortality of patients hospitalized with COVID-19 in a Swiss area - A retrospective cohort study. Swiss Med Wkly 150: 20314.
- Mazouri-Karker S, Vendeuvre LP, Sandoval J, Regard S, Braillard O, et al. (2020) Telemedicine at the heart of management of the COVID-19 crisis. Rev Med Suisse 16(706): 1699-1702.
- Kruse CS, Krowski N, Rodriguez B, Lan T, Jackeline V, et al. (2017) Telehealth and patient satisfaction: A systematic review and narrative analysis. BMJ Open 7(8): 1-12.
- Xu H, Huang S, Qiu C, Liu S, Deng J, et al. (2020) Monitoring and management of home-quarantined patients with COVID-19 using a wechat-based telemedicine system: Retrospective cohort study. J Med Internet Res 22(7): e19514.
- Nogués X, Sánchez-Martinez F, Castells X, Díez-Pérez A, Sabaté RA, et al. (2021) Hospital-at-home expands hospital capacity during COVID-19 pandemic. J Am Med Dir Assoc 22(5): 939-942.
- Monaghesh E, Hajizadeh A (2020) The role of telehealth during COVID-19 outbreak: A systematic review based on current evidence. BMC Public Health 20(1): 1193.
- Orlando JF, Beard M, Kumar S (2019) Systematic review of patient and caregivers' satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients' health. PLoS One 14(8): e0221848.
- Agha Z, Schapira RM, Laud PW, McNutt G, Roter DL (2009) Patient satisfaction with physician-patient communication during telemedicine. Telemed J E Health 15(9): 830-839.
- Gensini GF, Alderighi C, Rasoini R, Mazzanti M, Casolo G (2017) Value of telemonitoring and telemedicine in heart failure management. Card Fail Rev 3(2): 116-121.
- Polisena J, Tran K, Cimon K, Hutton B, McGill S, et al. (2010) Home telehealth for chronic obstructive pulmonary disease: A systematic review and meta-analysis. J Telemed Telecare 16(3): 120-127.
- Conley J, O'Brien CW, Leff BA, Bolen S, Zulman D (2016) Alternative strategies to inpatient hospitalization for acute medical conditions: A systematic review. JAMA Intern Med 176(11): 1693-1702.
- Jeppesen E, Brurberg KG, Vist GE, Wedzicha JA, Wright JJ, et al. (2012) Hospital at home for acute exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 5.
- Faruque LI, Wiebe N, Ehteshami-Afshar A, Liu Y, Dianati-Maleki N, et al. (2016) Effect of telemedicine on glycated hemoglobin in diabetes: A systematic review and meta-analysis of randomized trials. CMAJ 189(9): E341-E364.
- Rabuñal R, Suarez-Gil R, Golpe R, Martínez-García M, Gómez-Méndez R, et al. (2020) Usefulness of a Telemedicine Tool TELEA in the Management of the COVID-19 Pandemic. Telemed J E Health 26(11): 1332-1335.
- Buerhaus PI, Auerbach DI, Staiger DO (2020) Older clinicians and the surge in novel coronavirus disease 2019 (COVID-19). JAMA 323(18): 1777-1778.
- Arias-de la TJ, Alonso J, Martín V, Valderas JM (2020) Hospital-at-home as an alternative to release the overload of healthcare systems during the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic. J Am Med Dir Assoc 21(7): 990-991.
- Akiyama M, Yoo BK (2016) A systematic review of the economic evaluation of telemedicine in Japan. J Prev Med Public Health 49(4): 183-196.
- Mas MÀ, Santaeugènia SJ, Tarazona-Santabalbina FJ, Gámez S, Inzitari M (2018) Effectiveness of a hospital-at-home integrated care program as alternative resource for medical crises care in older adults with complex chronic conditions. J Am Med Dir Assoc 19(10): 860-863.
- Shepperd S, Doll H, Angus RM, Clarke MJ, Iliffe S, et al. (2009) Avoiding hospital admission through provision of hospital care at home: A systematic review and meta-analysis of individual patient data. CMAJ 180(2): 175-182.
- Stall N, Nowaczynski M, Sinha SK (2014) Systematic review of outcomes from home-based primary care programs for homebound older adults. J Am Geriatr Soc 62(12): 2243-2251.
- Dekio I, Hanada E, Chinuki Y, Akaki T, Kitani M, et al. (2010) Usefulness and economic evaluation of ADSL-based live interactive teledermatology in areas with shortage of dermatologists. Int J Dermatol 49(11): 1272-1275.
- Rademacher NJ, Cole G, Psoter KJ, Kelen G, Fan JWZ, et al. (2019) Use of telemedicine to screen patients in the emergency department: Matched cohort study evaluating efficiency and patient safety of telemedicine. JMIR Med Inform 7(2): e11233.
© 2022 Emmanuel Haefliger. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






