- Submissions

Full Text
Trends in Telemedicine & E-health
Assessment of the Effectiveness of Online and Face-to-Face Cognitive Behavioural Therapy for Insomnia/ Nightmares in Adults Exposed to Trauma Using Self-Report and Objective Measures: Preliminary Findings
Isaac F1*, Toukhsati SR1, Di Benedetto M2 and Kennedy GA1,3,4
1School of Science, Psychology and Sport, Federation University, Australia
2Psychologist, Private Practice, Australia
3School of Health and Biomedical Sciences, RMIT University, Australia
4Institute for Breathing and Sleep, Austin Health, Australia
*Corresponding author: Fadia Isaac, School of Science, Psychology & Sport Federation University, Office 211, Building HP, Mt Helen Campus, PO Box 663 Ballarat VIC 3353, Australia
Submission: January 13, 2022; Published: January 31, 2022

ISSN: 2689-2707 Volume 3 Issue 2
Abstract
Online therapies are gaining rapid attention since the COVID-19 pandemic. The ever-evolving way of living during the pandemic changed our health system and the way therapies are delivered and received. Online Cognitive Behavioural Therapy (CBT) has been shown to be as effective as face-to-face therapies in treating insomnia and/or nightmares in adults presenting with trauma symptoms. This review assessed the efficacy of online CBT for the treatment of insomnia in comparison to face-to-face CBT using selfreport and objective measures of sleep such as actigraphy. A literature search on the following databases was carried out: PubMed, MEDLINE, PsychINFO, Scopus, CINAHL, EMBASE, Cochrane Library, EBSCO and Taylor & Francis between January 1990 and January of 2022. Two studies met the inclusion criteria. Findings from this review showed that both online and face-to-face CBT were effective treatments of insomnia, with face-to-face outperforming online CBT in adults with trauma symptoms using sleep diaries. However, findings from actigraphy were not consistent with self-report measures. Further studies that assess and compare online and face-to-face psychological treatments for the treatment of insomnia/nightmares in those presenting with trauma symptoms are needed.
Keywords:Insomnia; Nightmares; Trauma; CBT; Objective; Self-report; Measure
Abbreviations:CBT-I: Cognitive Behavioural Therapy for Insomnia; PSG: Polysomnography; RCT: Randomised Controlled Trials; PRISMA: Preferred Reporting Items for Systematic Reviews and Meta- Analyses guidelines; PICO: Population, Intervention, Comparison, Outcome; PCBT-I=Professional Cognitive Behavioural Therapy for Insomnia; VCBT-I=Video Cognitive Behavioural Therapy for Insomnia; ISI=Insomnia Severity Index; ESS=The Epworth Sleepiness Scale; DBAS=The Dysfunctional Beliefs and Attitudes about Sleeps
Introduction
Sleep disorders including insomnia and nightmares are the most predominant sleep complaints reported by people exposed to trauma [1]. Research shows that both insomnia and nightmares continue to be prevalent even after successful treatment of trauma (77% and 52% respectively) [2,3]. Notably, the presence of sleep difficulties act as antecedents to the development of certain psychiatric conditions including Post-Traumatic Stress Disorder [PTSD] [4-6]. Moreover, treating sleep disturbances in those presenting with trauma, leads to reduction of symptoms for both sleep disorders and related trauma symptoms [6-10]. Therefore, it follows that the focus of future research should be on treating sleep disturbances in those presenting with co-morbid conditions. Cognitive behavioural therapy emerged as the treatment of choice for sleep disturbances, including Cognitive Behavioural Therapy for Insomnia (CBT-I). The American Academy of Sleep Medicine recommends the use of CBT-I as the first line treatment for insomnia [11]. CBT-I incorporates sleep restriction, stimulus control, cognitive restructuring of negative thoughts, relaxation techniques, and sleep hygiene [12]. More specifically, online CBT-I has gained rapid attention since the COVID- 19 pandemic. Online CBT-I is found to promote well-being and resilience and to be a suitable and feasible treatment for individuals subject to home confinement during the pandemic, those doing home schooling, mothers looking after children, and those who cannot access face-to-face health care in a timely manner [13,14]. Online treatment can reach a large number of individuals, is cost effective, it is easy to administer, and guarantees a timely-access to treatments in comparison to face-to-face modality [15]. A number of studies found online CBT-I to be as effective as face-to-face treatments for sleep difficulties including insomnia and nightmares, and at times online CBT-I outperformed face-to-face treatments [16,17].
In assessing the effectiveness of sleep-specific psychological interventions, researchers mainly rely on self-report measures such as sleep diaries and self-administered scales [18]. There are issues with self-report measures because people presenting with insomnia related to trauma tend to overestimate sleep latency (sleep state misperception), underestimate total sleep time and report sleep problems to be more severe than they are [19-21]. Actigraphy is an objective measure of sleep that measures sleepiness and wakefulness states through the use of a watch that is worn during sleep; it further provides appraisals of sleep parameters that are extracted from sleep diaries and Polysomnography (PSG), the gold standard for measuring sleep [22]. While, Polysomnography (PSG) studies have been robust in assessing sleep quality in individuals with and without trauma symptoms [23-25], PSG and actigraphy effectiveness in assessing treatment outcomes of online vs face faceto- face psychological sleep interventions in adults presenting with trauma symptoms is less clear. Leaders in sleep research call for the need to incorporate objective outcome measures such as PSG and actigraphy as well as self-report measures in assessing the effectiveness of sleep specific treatments to gain more confidence in treatment outcomes; and minimise the gap between objective and subjective measures of sleep [26]. This is vital hence the majority of clinicians working with adults with insomnia and/or nightmares do not have access to objective measures of sleep and rely exclusively on self-report measures. We aimed to address the above limitations by reviewing the literature systematically and summarising the findings on Randomised Controlled Trials (RCT) examining the effectiveness of online and face-to-face psychological treatments for insomnia/nightmares in individuals presenting with trauma symptoms using both self-report as well as objective measures of sleep (PSG and Actigraphy)
Method
The methodology for this review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA) [27]. The protocol for this systematic review was registered on PROSPERO on the 24th of February 2021 (CRD42021232975) [28]. The Population, Intervention, Comparison, Outcome (PICO) method [29] was used to address the following research question: How effective are online and face-toface psychological interventions for treating diagnosed insomnia/ nightmares in adults exposed to trauma using both self-report and objective measures of sleep.
Search method
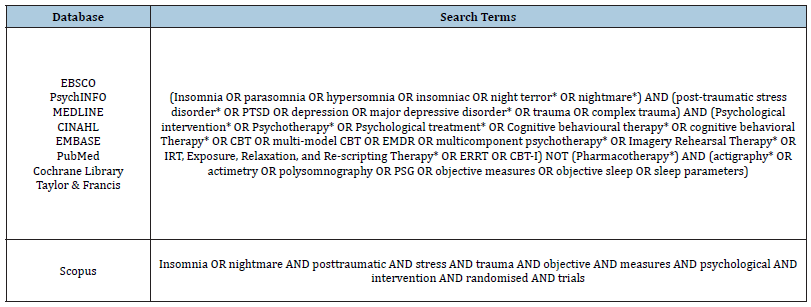
A literature search was performed using databases specified in (Table 1) between January 2021 and January 2022. Moreover, Google Scholar and reference lists manual examination were also implemented. (Table 1) shows the combination of search terms that were used to search databases.
Table 1:Search terms and databases searches.
Study inclusion criteria
Studies written in English and published between January of 1990 and January of 2022 were selected; only peer reviewed RCTs, on adults 18+ years, were considered for this review; studies treating diagnosed insomnia and/or nightmares, as diagnosed by a health professional, in those presenting with trauma symptoms were elected; RCTs assessing the effectiveness of sleep-specific psychological interventions on insomnia and/or nightmares using both objective and self-report scales were selected to be the inclusion criteria (Figure 1).
Figure 1:PRISMA flow diagram of database searches and final studies selection.
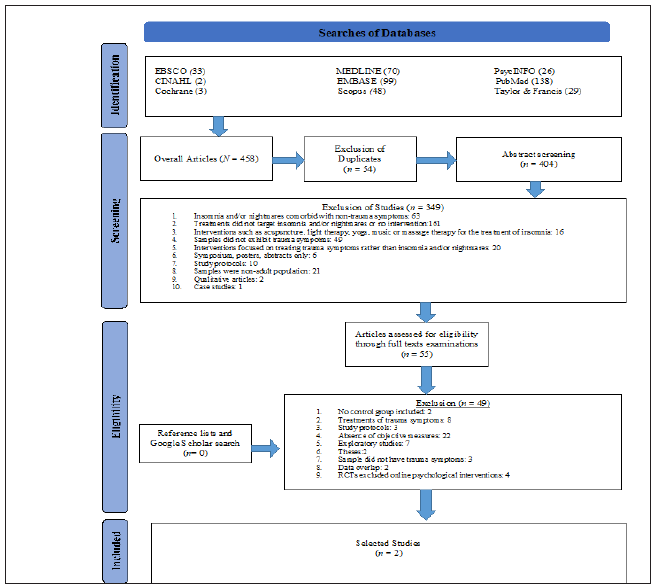
Exclusion criteria
By examining the title, abstract and full text articles, the following studies were excluded: animal studies, posters and oral presentations, symposiums, study protocols, non-adult studies, qualitative studies, RCTs without control or waitlist groups, studies without objective measures, studies with overlapping data, correlational studies, studies that did not include diagnosis of sleep disorders and/or trauma related symptoms, theses, studies treating PTSD rather than sleep disorders, and studies published prior to 1990 (Figure 1).
Examination of studies
The initial search of databases and screening of studies by title and abstracts was performed by one reviewer (FI). Full text examination of RCTs that deemed suitable were screened and underwent further assessment. Once the final articles were selected, their eligibility was reviewed by a senior researcher for verification and appropriateness (GK). A 100% inter-rater agreement between the two reviewers was achieved for the selected studies (FI and GK). There were some concerns about data overlap for four studies. Email correspondence with one author confirmed data overlap in two papers and another paper was deleted because data overlap could not be established.
Risk of bias assessment
The effect of, and adherence to, interventions in RCTs was assessed utilising the Revised Cochrane risk-of-bias tool for randomised trials (RoB 2) [30]. RoB 2 assesses biases in relation to deviations from per-protocol interventions, bias arising from the randomization process and measurement issues, missing data, and bias in reporting results. See (Table 2) for the results of a risk of bias assessment for the selected studies.
Result
A total of 458 studies were detected and screened by both title and the specified inclusion criteria. Fifty-four duplicates were removed from the analysis. This led to examination of 404 articles by abstract. A total of 349 articles were excluded after careful consideration of the inclusion criteria ((Figure 1) for a detailed description of the excluded studies). Fifty-five randomised trials were then assessed by examination of full articles. This led to the exclusion of 53 studies for reasons delineated in (Figure 1). An additional manual checking of reference lists and Google Scholar produced no further articles. Two RCTs met the inclusion criteria and were assigned for the final analysis of this systematic review. (Table 3) provides details of the two RCTs.
Table 2:Risk of bias assessment using the revised cochrane risk-of-bias tool for randomised trials (RoB 2).
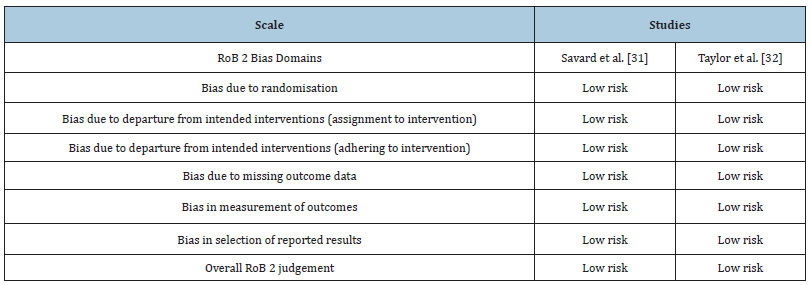
Table 3:The efficacy of psychological treatments for insomnia and/or nightmares.
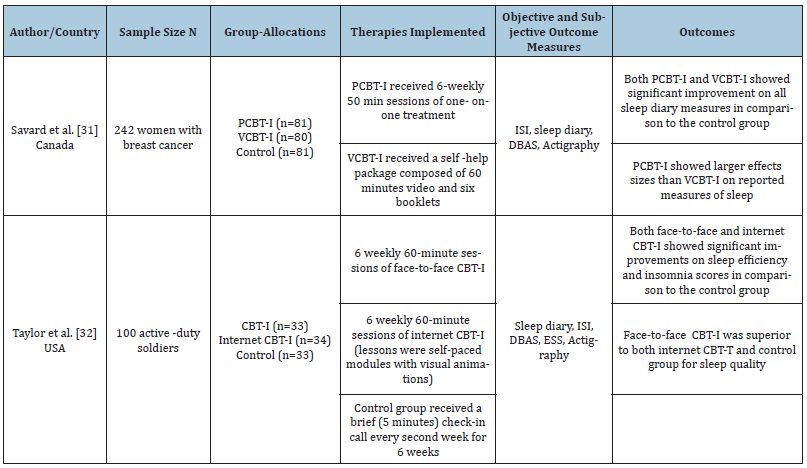
Note: CBT-I=Cognitive Behavioural Therapy for Insomnia; PCBT-I=Professional Cognitive Behavioural Therapy for Insomnia; VCBT-I=Video Cognitive Behavioural Therapy for Insomnia; ISI=Insomnia Severity Index; ESS=The Epworth Sleepiness Scale; DBAS=The Dysfunctional Beliefs and Attitudes about Sleep.
Sample characteristics
Three hundred and forty-two participants were included from the two selected studies. There were 259 females and 83 males. Their mean age ranged between 33 and 54 years.
Outcome measures
The main measure of insomnia was selected to be sleep efficiency extracted from insomnia or nightmare diaries. Sleep efficiency was deemed to be the most appropriate parameter hence it encompasses total sleep time, sleep onset latency, wake time after sleep onset and morning wakeup time [9]. Actigraphy was used in both studies as an objective measure of sleep.
Statistical reporting of data
The interaction effect of time (pre-versus post-intervention), by group (intervention versus control group) was reported where available. Main effects alone were reported if interactions of time by group were not reported.
Findings from selected studies
Face-to-face versus internet/video CBT-I on diary measures: Only two RCTs met the inclusion criteria and were selected for this review. The two RCTs compared the effectiveness of faceto- face and online CBT-I for the treatment of insomnia in those exposed to trauma. Savard and colleagues [31] applied six sessions of CBT-I (stimulus control, sleep restriction, cognitive restructuring, and sleep hygiene) for the treatment of insomnia in women with cancer. CBT-I revealed a significant group by time effect for sleep efficiency SE as measured by sleep diaries for both face-to-face and online CBT-I (p=.001) in comparison to no treatment/control group from baseline to post-intervention. However, effect sizes were greater for face-to-face CBT-I (from pre- to post-treatment, d=0.66 to d=1.84) than online CBT-I (d=0.50 to d=1.40) and control group (d=0.23 to d=0.69) [31]. Furthermore, more participants in the face-to-face CBT-I (71.3%) experienced remission than online CBT-I (44.3%) and control group (25.7%) (p< .04) [31]. Similarly, six sessions of either face-to-face or online CBT-I treatment consisting of stimulus control, sleep restriction, cognitive restructuring, sleep hygiene and relaxation were implemented for the treatment of insomnia in military personnel [32]. A significant group by time interaction for both face-to-face and online CBT-I treatment was found in comparison to the control group receiving a 5-minute check in calls throughout the trial on sleep efficiency (p= .002). Although, no significant difference was detected between face-to-face and online CBT-I treatment on sleep efficiency, larger effect size was found for face-to-face (d=0.89) than online CBT-I (d=0.53) when both treatments were compared to the control group. At six month follow up results remained significant for sleep efficiency (p<.05) between post-treatment and six month follow up for both face-to-face and online CBT-I groups suggesting a durability of treatment [32]. The above findings from the two studies suggest that both face-to-face and online CBT-I are effective in significantly improving sleep efficiency parameters in those presenting with diagnosed insomnia presenting with trauma symptoms with face-to-face CBT-I outper forming online CBT-I with large effects sizes. Both studies were assessed as high-quality RCTs according to the RoB 2 scale [30-32].
Objective/actigraphy assessment of insomnia: Both studies found no significant group by time interaction effect on the actigraphy measures for any sleep parameters except for a reduction of total sleep time TST from pre- to post-treatment for those who received face-to-face CBT-I in comparison to online CBT-I (p=.004, p=.05 respectively) [31,32].
Discussion
We searched the literature for RCTs that compared online and face-to-face CBT for diagnosed insomnia/nightmares in those exposed to trauma using self-report and objective measures of sleep. Two RCTs were located that compared online and face-to-face CBT for the treatment of insomnia in those with trauma symptoms using self-report and objective measures of sleep [31,32]. No studies for the treatment of nightmares were identified in this review. Preliminary findings from this review showed that both face-to-face and online CBT-I are effective in improving sleep efficiency with faceto face CBT-I showing larger effect sizes than online CBT-I [31,32]. Online CBT-I can be challenging due to the absence of therapist’s support and other issues relating to access and motivation of client [32]. Face-to-face CBT-I outperformed online CBT-I in this review which is in line with other research findings, perhaps due to participants having the support of a therapist who provides encouragement and reassurance in relation to treatment [31,33,34].
Both support and helpful feedback provided by a therapist can affect treatment outcomes positively [33]. This is contradictory to what has been reported recently by Gieselmann and Pietrowsky [17] who found that digital treatment for insomnia outperformed face-to-face treatment. Researchers of this study suggested that online therapy can potentially be made more personalised to meet the needs of the individual by increasing self-governance and personal responsibility towards therapy, and providing more privacy to those receiving therapy [17]. This review also showed that results obtained from actigraphy were not in line with subjective measures. Research suggests that the reduction of TST on actigraphy could be a function of the rigorous application of sleep restriction therapy which restricts the amount of time in bed, as a result affecting the recorded TST [16,35]. Objective measures are not widely researched due to costs involved and difficulties with implementation that potentially affects sleep quality for participants during sleep [36,37].
The COVID-19 pandemic changed the way we live. It has also changed the way we receive and provide health care. In order for us to continue to provide health care in a sensible and effective way, digital therapies and online methods need to come to the forefront of research and clinical practice. The progression in digital therapies and treatment methods have been slow despite considerable demands for them [38]. This review highlighted the scarcity of online CBT-I interventions for the treatment of insomnia and the absence of studies that addressed nightmares in those presenting with symptoms of trauma using both self-report and objective measures of sleep. As such, there is an urgent need for RCTs that address the above limitations. We propose the need for immediate RCTs that assess the effectiveness of online CBT treatments for both insomnia and nightmares in adults presenting with trauma symptoms. We also propose the need for clinical assessments of sleep and trauma symptoms in this cohort. The effectiveness of treatments’ outcomes should be assessed using both objective and subjective measures at pre, post and follow up treatments. Perhaps more research and more rigours implementation of measures of sleep will assist in upscaling online treatments to be as effective as face-to-face interventions during a time where COVID-19 continues to impact our lives in an unprecedented way.
Acknowledgment
Fadia Isaac is supported by an Australian Government Research Training Program (RTP) Fee-Offset Scholarship administered through Federation University.
References
- Isaac F, Toukhsati, SR, Benedetto M, Kennedy GA (2021) A systematic review of the impact of wildfires on sleep disturbances. International Journal of Environmental Research and Public Health 18(19): 10152-10174.
- Taylor DJ, Pruiksma KE, Hale W, McLean CP, Zandberg LJ, et al. (2020) Sleep problems in active duty military personnel seeking treatment for posttraumatic stress disorder: presence, change, and impact on outcomes. Sleep 43(10): zsaa065.
- Pruiksma KE, Taylor DJ, Wachen JS, Mintz, J, Caughan SY, et al. (2016) Residual sleep disturbances following PTSD treatment in active duty military personnel. Psychological Trauma: Theory, Research, Practice, and Policy 8(6): 697-701.
- Babson KA, Feldner MT (2010) Temporal relations between sleep problems and both traumatic event exposure and PTSD: a critical review of the empirical literature. Journal of Anxiety Disorders 24(1): 1-15.
- Belleville G, Guay S, Marchand A (2009) Impact of sleep disturbances on PTSD symptoms and perceived health. The Journal of Nervous and Mental Disease 197(2): 126-132.
- Germain A (2013) Sleep disturbances as the hallmark of PTSD: Where are we now? American Journal of Psychiatry 170(4): 372-382.
- Colvonen PJ, Straus LD, Stepnowsky C, McCarthy MJ, Goldstein LA, et al. (2018) Recent advancements in treating sleep disorders in co-occurring PTSD. Current Psychiatry Reports 20(7): 48.
- Ulmer CS, Edinger JD, Calhoun PS (2011) A multi-component cognitive-behavioral intervention for sleep disturbance in veterans with PTSD: A pilot study. Journal of Clinical Sleep Medicine 7(1): 57-68.
- Taylor DJ, Pruiksma KE (2014) Cognitive and behavioural therapy for insomnia (CBT-I) in psychiatric populations: A systematic review. International Review of Psychiatry 26(2): 205-213.
- Wu JQ, Appleman ER, Salazar RD, Ong JC (2015) Cognitive behavioral therapy for insomnia comorbid with psychiatric and medical conditions: A meta-analysis. JAMA Internal Medicine 175(9): 1461-1472.
- Edinger JD, Arnedt JT, Bertisch SM, Carney CE, Harrington JJ, et al. (2021) Behavioral and psychological treatments for chronic insomnia disorder in adults: An American Academy of sleep medicine clinical practice guideline. Journal of Clinical Sleep Medicine 17(2): 255-262.
- Morin CM, Espie CA (2007) Insomnia: A clinical guide to assessment and treatment. Springer Science & Business Media, USA.
- Altena E, Baglioni C, Espie CA, Ellis J, Gavriloff D, et al. (2020) Dealing with sleep problems during home confinement due to the COVID‐19 outbreak: Practical recommendations from a task force of the European CBT‐I academy. Journal of Sleep Research 29(4): e13052.
- Cheng P, Casement MD, Kalmbach DA, Castelan AC, Drake CL (2021) Digital cognitive behavioral therapy for insomnia promotes later health resilience during the coronavirus disease 19 (COVID-19) pandemic. Sleep 44(4): zsaa258.
- Sawdon OL, Elder GJ, Santhi N, Alfonso-Miller P, Ellis JG (2021) Testing an early online intervention for the treatment of disturbed sleep during the COVID-19 pandemic in self-reported good and poor sleepers (Sleep COVID-19): Study protocol for a randomised controlled trial. Trials 22(1): 1-13.
- Bruin EJ, Bögels SM, Oort FJ, Meijer AM (2015) Efficacy of cognitive behavioral therapy for insomnia in adolescents: A randomized controlled trial with internet therapy, group therapy and a waiting list condition. Sleep 38(12): 1913-1926.
- Gieselmann A, Pietrowsky R (2019) The effects of brief chat-based and face-to-face psychotherapy for insomnia: A randomized waiting list-controlled trial. Sleep Medicine 61: 63-72.
- Stout JW, Beidel DC, Alfano CA, Mesa F, Trachik B, et al. (2017) Sleep disturbances among combat military veterans: A comparative study using subjective and objective sleep assessments. Military Psychology 29(3): 189-201.
- Caldwell BA, Redeker N (2005) Sleep and trauma: An overview. Issues in Mental Health Nursing 26(7): 721-738.
- Perlis ML, Giles DE, Mendelson WB, Bootzin RR, Wyatt JK (1997) Psychophysiological insomnia: The behavioural model and a neurocognitive perspective. Journal of Sleep Research 6(3): 179-188.
- Slightam C, Petrowski K, Jamison AL, Keller M, Bertram F, et al. (2018) Assessing sleep quality using self‐report and actigraphy in PTSD. Journal of Sleep Research 27(3): e12632.
- Smith MT, McCrae CS, Cheung J, Martin JL, Harrod CG, et al. (2018) Use of actigraphy for the evaluation of sleep disorders and circadian rhythm sleep-wake disorders: An American Academy of sleep medicine clinical practice guideline. Journal of Clinical Sleep Medicine 14(7): 1231-1237.
- Baglioni C, Nanovska S, Regen W, Spiegelhalder K, Feige B, et al. (2016) Sleep and mental disorders: A meta-analysis of polysomnographic research. Psychological Bulletin 142(9): 969-980.
- Kobayashi I, Boarts JM, Delahanty DL (2007) Polysomnographically measured sleep abnormalities in PTSD: A meta‐analytic review. Psychophysiology 44(4): 660-669.
- Zhang Y, Ren R, Sanford LD, Yang L, Zhou J, et al. (2019) Sleep in posttraumatic stress disorder: A systematic review and meta-analysis of polysomnographic findings. Sleep Medicine Reviews 48: 101210.
- Buysse DJ, Ancoli-Israel S, Edinger JD, Lichstein KL, Morin CM (2006) Recommendations for a standard research assessment of insomnia. Sleep 29(9):1155-1173.
- Moher D, Liberati A, Tetzlaff J, Altman DG, Prisma Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine 6(7): e1000097.
- International Prospective Register of Systematic Reviews (PROSPERO) (2021) Psychological interventions and their effects on the treatment of insomnia and nightmares.
- Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S (2014) PICO, PICOS and SPIDER: A comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Services Research 14(1): 579.
- Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JA (2019) Assessing risk of bias in a randomized trial. Cochrane Handbook for Systematic Reviews of Interventions, pp. 205-228.
- Savard J, Ivers H, Savard MH, Morin CM (2014) Is a video-based cognitive behavioral therapy for insomnia as efficacious as a professionally administered treatment in breast cancer? Results of a randomized controlled trial. Sleep 37(8): 1305-1314.
- Taylor DJ, Peterson AL, Pruiksma KE, Young-McCaughan S, Nicholson K, et al. (2017) Internet and in-person cognitive behavioral therapy for insomnia in military personnel: A randomized clinical trial. Journal of Sleep and Sleep Disorders Research 40(6): zsx075.
- Lancee J, Straten A, Morina N, Kaldo V, Kamphuis JH (2016) Guided online or face-to-face cognitive behavioral treatment for insomnia: A randomized wait-list controlled trial. Sleep 39(1): 183-191.
- Palmqvist B, Carlbring P, Andersson G (2007) Internet-delivered treatments with or without therapist input: Does the therapist factor have implications for efficacy and cost?. Expert Review of Pharmacoeconomics & Outcomes Research 7(3): 291-297.
- Miller CB, Espie CA, Epstein DR, Friedman L, Morin CM, et al. (2014) The evidence base of sleep restriction therapy for treating insomnia disorder. Sleep Medicine Reviews 18(5): 415-424.
- Hood B, Bruck D, Kennedy G (2004) Determinants of sleep quality in the healthy aged: the role of physical, psychological, circadian and naturalistic light variables. Age and Ageing 33(2): 159-165.
- Moore M, Evans V, Hanvey G, Johnson C (2017) Assessment of sleep in children with autism spectrum disorder. Children 4(8): 1-17.
- Wind TR, Rijkeboer M, Andersson G, Riper H (2020) The COVID-19 pandemic: The ‘black swan’ for mental health care and a turning point for e-health. Internet interventions 20: 100317.
© 2022 Isaac F. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






