- Submissions

Full Text
Trends in Telemedicine & E-health
Telemedicine in the COVID-19 Era: Strengths and Weaknesses
G Olmo1*, L Lopiano2 and A Mauro2
1Department of Control and Computer Engineering, Politecnico di Torino, Italy
2Department of Neuroscience Rita Levi Montalcini, Università degli Studi di Torino, Torino, 10126, Italy
*Corresponding author: G Olmo, Department of Control and Computer Engineering, Politecnico di Torino, Torino, 10129, Italy
Submission: December 1, 2020; Published: April 22, 2021

ISSN: 2689-2707 Volume 2 Issue 5
Abstract
Telemedicine (TLM) has a great innovation potential, and this fact has emerged dramatically in this pandemic period. Besides the monitoring of COVID-19 patients themselves, TLM can improve the followup of affected by chronic diseases, whose access to hospitals and outpatient structures is limited due to the risk connected with the pandemic and the overload experienced by the medical structures and personnel. Hence, this period represents an occasion to experiment new care models. For these purposes, we have implemented a TLM system to help clinicians in the follow-up of COVID-19 patients both in hospital and at home. The same infrastructure has great potential of applications in other fields, e.g., neurodegenerative diseases. During our experiments, we have pointed out some strengths and weaknesses of this novel approach to care. Our conclusion is that, whereas technology and data processing is quite mature, many non-technical aspects have still to be faced in order TLM instruments can enter the daily clinical practice and deeply transform care models.
Introduction
The SARS-CoV-2 pandemic posed a difficult dilemma about the clinical management of patients in all branches of medicine, spanning from the care of COVID-19 patients themselves to the follow-up of chronically ill persons at risk of COVID-19 complications. From one hand, frail patients must be protected from disease-related risks, and their attendance at hospitals should be minimized to reduce the chance of infection and virus spreading. On the other hand, this must not be detrimental for their overall health conditions, also considering that the new procedures imposed by the pandemic imply long waiting lists to be faced with. The possibilities offered by Telemedicine (TLM) to monitor patients at home represent an opportunity, and this pandemic may enable large- scale experimentation of services with great added value. However, so far, there is lack of evidence-based guidelines on how to modify current clinical practice. TLM should go well beyond simple teleconsulting to be appreciated by patients and caregivers as a truly innovative cure model and not only a palliative. Moreover, as pointed out in [1], the accelerated development of TLM raises concerns related to safety, privacy, prevention of data misuse. In this paper, we describe our experience in the development and experimentation of a TLM tool to monitor the clinical evolution of COVID-19 patients, implemented keeping in mind possible applications beyond the pandemic.
State of the Art
Several proposals have been published for home management of COVID-19 patients via transmission of parameters such as temperature and SpO2 to clinical centers. For example, in [2] a TLM system is implemented for monitoring the progression of home-quarantined patients. A smartphone app is addressed to enable a two-way communication between patients and clinicians, and data stored on a cloud service support the team to undergo treatment decisions. Similarly, in [3] an Android-based mobile application is implemented for patients-doctors real-time communication. Embedded sensors automatically capture and transmit physiological parameters to enable a remote monitoring of patients treated at home. Besides clinical parameters, properly designed questionnaires related to symptoms with known correlation with the disease (e.g., ageusia, anosmia, cough [4]) can help in early diagnosis of disease complications. Moreover, the analysis of voice segments, possibly prior and after a light physical exercise, embed sensible information on the patients’ pulmonary conditions [5]. These parameters can be gathered by nursing personnel in hospital of nursing homes, or selfmanaged by patients themselves at home.
The Bot
The implemented TLM system is based on an open-source Telegram Bot accessed by means of an iOs/Android smartphone. Guided by the chat with the Bot, patients or nursing staff enter vital parameters (temperature, SpO2, heart rate). Additional information on the lung involvement related to SARS-CoV-2 infection is obtained by measuring respiratory rate and fatigue, and reduction in SpO2 levels after a light exercise. Data are processed using Machine and Deep Learning (ML/DL) algorithms to capture early signs of respiratory function deterioration. The “respiratory fatigue” is estimated using a short sentence pronounced by the patient, and the respiratory rate analyzing 30-s silence with the microphone activated. After possible execution of a short walking test (30 steps), Sp02, respiratory rate and voice samples are reinserted. Telegram performs end-to-end cryptography, thus ensuring compliance with privacy and security regulations when transmitting data. The access to the dedicated server in a secure domain is granted to authorized personnel only. The gathered data enable the study of correlations with variables previously considered irrelevant for the clinical evolution of COVID-19 and long-term complications of exposure to SARS-CoV-2. Hence, the application has a twofold application; from one hand, it provides an effective follow-up of patients at home; from the other hand, it addresses Artificial Intelligence application to heterogeneous data, in order to unveil correlation of the disease progression and complications with several clinical and environmental variables.
Experimentation and Emerging Problems
A community version of the Bot has been developed to gather
data from hospitalized patients. A member of the clinical/nursing
staff records the physiological parameters of patients, either
already diagnosed with Covid-19 infection or exhibiting symptoms
compatible with the infection. Again, if the conditions allow this,
respiratory rate, voice segments and possible reduction in SpO2
levels are measured after a light exercise.
Preliminary tests have been carried out at Istituto Auxologico
Italiano, Piancavallo (VB), Italy, and the Department of
Neuroscience, University Hospital “Molinette”, Torino, Italy on
27 patients positive to SARS-CoV-2. Among these latter, 24 have
been able to perform the walking test and the voice registration.
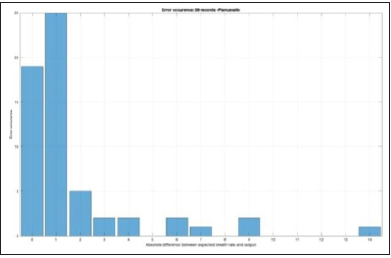
Preliminary results showed that the respiratory rate can be
estimated with adequate precision from 30-s recoding with the
smartphone. The absolute error between the automatic evaluation
and the respiratory rate measured by the medical staff is reported in
Figure 1. It can be appreciated that in most cases, the error amounts
to 0 or 1 respiratory acts, even though the registrations have been
performed in a noisy environment, using a smartphone packed up
in cellophane sheets for safety reasons. Then, the voice data have been analyzed to verify the feasibility of classifying voice measures
as a function of the patients’ pulmonary conditions. Patients were
divided into two subgroups:
Figure 1: Absolute error between the automatic evaluation and the respiratory rate measured
Class 1: patients that exhibited a significant reduction of SpO2
(at least 10mmHg) after the walking test.
Class 2: patients that did not exhibited a significant reduction of
SpO2 after the walking test.
A set of features able to drive the classification task has been defined. Central values of MFCC6 mean, MFCC3 std and F0 std distributions [6] exhibit clearly distinct statistical characteristics in either class, with moderate-high Pearson correlation coefficient between feature and class label. We have analyzed the distribution of these features when either class is further divided into pre- and postwalking test. In particular, the MFCC6 feature measured on Class 2 patients showed a large variance when evaluated prior or after the walking test, revealing a potential usefulness of this parameter for detailed estimation of the patients’ pulmonary conditions. These features were used to drive a linear SVM classification [7] of voice data into pre- and post-walking test classes, achieving accuracy 60%, sensibility 60%, specificity 61%, AUC 0.68. Even though not completely satisfactory, it must be noticed that these data are very preliminary; the few patients were asked to pronounce a single word in a noisy environment, using a smartphone packed up into cellophane sheets. Hence, a lot of improvements to this condition can be identified. Besides these very preliminary technical results, the lessons learned from these experiments are related to the effectiveness, usability and acceptance of a TLM solution. Nurses and clinicians operated in a very difficult situation, end even though the patients were non-critical, the following issues emerged with dramatic evidence.
a) A TLM tool must be extremely easy to use. Even though, in
our opinion, the Bot was very simplified, nurses and clinicians
had to face issues which had not been thought of (managing
the touch screen while wearing safety devices, operating the
smartphone microphone in Telegram environment, using the
Bot in noisy environment, being interrupted while taking a
measure, etc.). There issues are likely not to manifest in home environment; however, the patients’ capabilities to manage
technical instrumentation properly cannot be over-estimated.
A non-correct use of the monitoring instrumentation must be
considered as one-if not the main-confounding variable when
applying sophisticated AI algorithm to gather information from
the data.
b) A TLM tool must be quick to use. In community
environment, nurses and clinicians were somehow disappointed
when they were asked to use time-consuming procedures.
This can be understood, as they are overwhelmed by tasks to
be performed with the maximum possible efficiency. Hence, a
TLM instrument should be devised, presented, and accepted
as a tool enabling time savings, and not as a further duty to
fulfill. As for patients at home, their boredom and annoyance
in having to complete so many tasks every day should not be
underestimated.
c) Proper information should be provided to get cooperation
of all the involved parties (including caregivers) and achieve
the best possible efficacy of novel technologies.
d) Integration of the various electronic data of patients
should be addressed as a major requirement. Unfortunately,
this task is difficult because in Italy there is a noticeable
standardization lack, and every hospital uses different formats
and tools for recording data of their patients.
Conclusion
Despite technological advances, the implementation of TLM in the clinical practice is being delayed due to concerns regarding validation and acceptability, difficulties in interpreting the data, unclear correlation with patient-centered measures (such as independence and quality of life), lack of standardization. Large, randomized trials are lacking, and systematic reviews often report inconsistent conclusions. Moreover, in our experience, critical human factors such as capability and will of using the technology are of paramount importance, especially in critical situations such as that induced by the SARS-CoV-2 pandemic. On the other hand, we believe that the use of TLM tools is both unavoidable and advantageous in many medical fields. For example, as for the COVID-19 pandemic, proper analysis of other data related to lock-down, for example the consequences of loneliness and isolation on physical and cognitive deterioration, can represent innovative research elements. The generalization potential to other chronic diseases (asthma, COPD, neurodegenerative diseases) is considerable. The study of potential correlations with variables previously considered irrelevant to the clinical evolution of COVID-19 or other pathologies, as well as possible clinical consequences of exposure to SARS-CoV-2 in cured patients, whether in relation to lung or other function, are issues of paramount importance that can be addressed once large masses of data are made available with proper TLM tools.
References
- Gerke S, Shachar C, Chai PR, Glenn CI (2020) Regulatory, safety, and privacy concerns of home monitoring technologies during COVID-19. Nature Medicine 26: 1176-1182.
- Xu H, Huang S, Qiu C, Liu S, Deng J, et al. (2020) Monitoring and management of home-quarantined patients with covid-19 using a Wechat-Based telemedicine system: Retrospective cohort study. J Med Internet Res 22(7): e19514.
- Iutosin T, Absalom EE (2020) Smart healthcare support for remote patient monitoring during covid-19 quarantine. Informatics in Medicine Unlocked 20: 100428.
- Jennifer Chu (2020) Artificial intelligence model detects asymptomatic Covid-19 infections through cellphone-recorded coughs. MIT News Office Cambridge, MA, USA.
- Emily A (2020) Alexa, do I have COVID-19? Nature 586(7827): 22-25.
- Koolagudi SG, Rastogi D, Rao KS (2012) Identification of language using Mel-frequency cepstral coefficients (MFCC). Procedia Engineering 38: 3391-3398.
- Ladicky L, Torr PH (2011) Linear support vector machines. Proceedings of the 28th International Conference on Machine Learning (ICML 2011) Bellevue, Washington USA, pp: 985-992.
© 2021 G Olmo. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






