- Submissions

Full Text
Techniques in Neurosurgery & Neurology
Lumbar Spinal Angiolipoma Managed by Inter- Laminar Full Endoscopic Approach
Marcio R Ramalho Cunha*, Marcello R Ramalho Cunha, Leonardo Correia, Marcelo Glauber, Marcia Luisa M Cunha and Guilherme Monteiro Cunha
Trauma Center, Brazil
*Corresponding author:Marcio R Ramalho Cunha, Trauma Center, Brazil
Submission: September 19, 2023;Published: November 02, 2023

ISSN 2637-7748
Volume5 Issue4
Abstract
Benign spinal tumors have been treated for a long time by surgical open procedures with the solemn message of removing the lesion as much as you can without bringing damage to the neural structures. In the last years we’ve got a lot papers released pointed the tubular M.I.S as a safe way to extract benign spinal tumors .We would like to present a large extradural Angiolipoma be-tween L1/L2 removed by a full endoscopic inter laminar approach under general anesthesia . The major benefit of choosing this surgical option is to decrease the tissue injury related to the approach and perform an efficient removal of the lesion. The preservation of muscle ligaments and bone structures, bring less back pain, low pos operative drugs assistance, fast recovery and as principal consequence no future symptoms associated with spinal instability [1-8].
Keywords: Spine surgery; Minimally invasive approach; Full endoscopy; Lumbar angiolipoma
Introduction
The spinal angiolipoma is a benign tumor composed of both mature fatty and abnormal vascular elements, predominantly located in the mid-thoracic region differently from spinal lipomas commonly found in the lumbar-sacral region [8-30]. They account for 0.04 -1,2% of all spinal axis tumors, undoubtedly a quite rare situation, accounting for about 2-3% of extradural spinal tumors. Normally after the diagnosis of a spinal tumor associated with any neurological sign the surgical treatment is a legitime option to be made. The full endoscopic approach is gaining a lot of followers choosing this option to treat soft disk herniation, spinal stenosis, and other spinal pathologies in the last years. One of the great advantages of this surgical modality is to decrease the complications associated with the open procedures, collecting all the benefits associated with this minimally invasive approach. We reported a case of a large extra dural dorsally spinal angiolipoma between L1/L2, totally removed by a percutaneous full endoscopic inter laminar approach with two years of follow up without any signs of recurrence.
Case Report
History and examination
A male 48-year-old patient, complaining of progressively lumbar back pain for 02 months radiating down to the anterior aspect of the right leg increasing with walking movement without response to the conservative therapy. He got no major neurological signals like muscle weakness, abnormalities in tendon reflexes and radiculopathies.
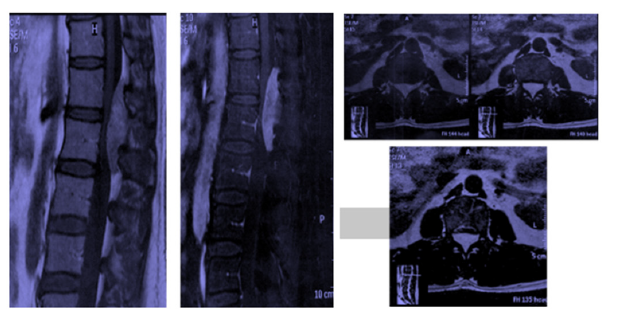
PRE OP Images
An MRI demonstrated a posterior large epidural mass located between L1/L2 with features of a benign spinal tumor suggestive of spinal angiolipoma. This tumor was a homogeneous mass, measured 5,8 x1,8cm moderately hyper-intense relative to spinal cord in T1 and T2 weighted images (Figure 1).
Figure 1:PRE OP Images.
POS OP Images
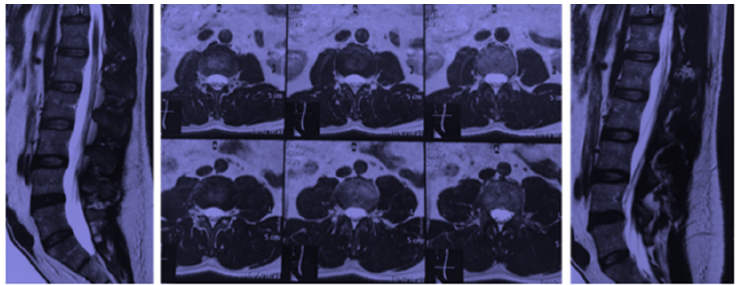
The MRI demonstrated a total resection of the lesion by the percutaneous full endoscopic inter laminar procedure and the histopathological exam confirmed a spinal angiolipoma. Right down below, the first post operative control, four months later (Figure 2 & 3).
Figure 2:POS OP Images.
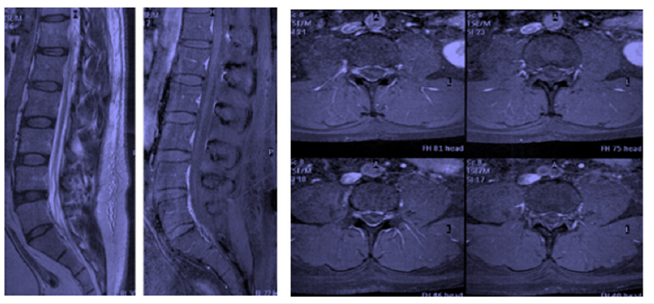
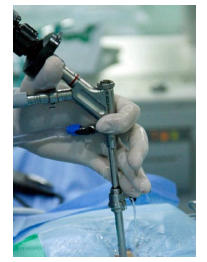
Figure 3:Transoperative.
Surgical technique
The surgical procedure was made by general anesthesia with the patient under prone position. The entry point has been set with the assistance of a C-arm in AP position after placing the end plates of L1/L2 in parallel. A single incision of 08 mm was made in the interlaminar bone window 15 mm from the midline. An obturator is bluntly inserted through the lumbar fascia toward the inter laminar space, then a working channel slides over the obturator under the C-arm AP and lateral confirmation. After this we’ve inserted the endoscope through the working cannula making a good enlargement of the inter laminar bone window, with the assistance of a diamond burr, from the base to the tip of the inferior ascendent facet stretching to the inferior aspect of the lamina of L1. Finally, you’ve made a direct opening of the yellow ligament with assistance of micro punches promoting a good exposition of the lesion. The tumor was a mixing between red and yellow fat with clear borders between the dura mater and the lesion. A total resection was made by piecemeal removal of the lesion, with a total surgical time of two hours and forty minutes. Of course, we could decrease the surgical time by half if we had a proper tool like a tip of an ultrasonic aspirator to extract the lesion through the endoscope. The patient had a hospital discharge within twelve hours after the procedure, using a single pain killer and could have a rapid return to his job. We’ve been following the patient for the last three years and his last exams showed no recurrence of the tumor. Even though is a single case, we believe that in well selected cases of benign spinal tumor, there is a chance to treat these lesions by full endoscopy (Figure 4).
Figure 4:Two Years Later.
Discussion
The spinal angiolipoma is a benign lesion, macroscopically the tumor is an encapsulated or non-capsulated, reddish soft mass extending into the extradural space of the spinal canal. They could be non-infiltrating or infiltrating extending to the vertebral body [8]. Normally, the clinical symptoms are mostly sensory disorders associated or not with motor deficits below the level of the lesion [30]. Radiographically the x-rays are normal with few reports of bone involvement in a quite rare situation, bringing bone erosion with a coarsened trabecular pattern typically associated with vertebral hemangioma. Even though we have some reports of diagnosis made by CT scan, the best radiological diagnosis is made by MRI, which are hyper-intense on non-contrast T1-weighted images to their fatty contents and most lesions enhance with Gadolinium administration, whereas T2-weighted imaging can be variable, bur is usually hyper-intense. As we know, surgical treatment is a legitime procedure to finish the patient’s symptoms. Open surgery associated with a laminectomy is the most common procedure all over the world to remove these lesions safely. Well, the benefits of surgical performance removal of spinal pathologies by minimally invasive way bring less complications, like: Less post op infection, minimal blood loss, reduced drug pain control, short hospital time and rapid recovery for daily activities [2,20-33]. Since 1975, Hijikata et al. [9] developed this new conception to treat contained disk herniations by a lateral percutaneous procedure minimizing the tissue lesion in the management of these lesions [31]. Undoubtedly this technique inspired other colleagues to follow this new concept, leading to the improvement of this surgical option. So, after the release of the YESS endoscope by Anthony Young et al, through an inside-out trans foraminal technique, indeed bringing a new era to the full endoscopy treatment in the management of soft disc herniation [32,33]. After some years, the Inter laminar full endoscopic approach was described by Ruetten et al. [21] treating the disk herniation by the midline approach opening a new conception in the full endoscopic treatment [21].
The approach was made by the inter laminar bone window, opening the yellow ligament under a direct vision bringing almost the same conceptions of a classical micro discectomy, but now made under a skin incision less than 01cm [2,23,24]. We’ve been constantly performing this procedure to treat disk herniations and spinal stenosis in the last years from the lumbar to cervical region, increasing enthusiasm about the possibilities to expand this technique to treat small benign tumors. So far, we have few reports of benign spinal tumors by full endoscopy [25-34], the great majority of M.I.S publications the surgical treatment was made by assisted tubular endoscopy procedure [6]. The full endoscopy minimize the local tissue aggression and bring others benefits like the magnification and clearness of the anatomical structures and the great advantage to promote an over the top 25 or 30 angle visualization of the spinal elements in the contra-lateral side. One of main concerns in these procedures is the blur provoked by small bleedings in the tumor lesion piecemeal resection, being responsible to enlarge the surgical time resection. Perhaps with the assistance of proper tools like, ultrasonic aspirator or a RITA radio-frequency device, these blur hindrances could be easily overwhelmed, decreasing the surgical time and making it better than open procedures. The disadvantage of this technique is lack of maneuvering area caused by the rigidity of the working channel and the absence of a second hand to promote a better exposure of the surgical area.
The risk of a dural tear is indeed a concern in the endoscopic spinal procedure, because direct dural repair is always a big challenge. We have other options like: Grafts, fibrin sealant and patches that are associated with bed rest and oral medications normally bringing a good response to this conservative therapy. The great advantage of full endoscopy is the reduction of dead space in the surgical approach, making it easier to manipulate in situations of dural tear and making the exteriorization of CSF leak a quite rare situation. Even though the anatomical difficulties, related to the multilevel extension of the tumor, we could perform a total resection of the lesion with a single skin incision of 08mm keeping all the advantages related with a minimal invasive full endoscopic approach and bringing good expectations for this kind of treatment in the management of benign spinal tumors.
Conclusion
Surgical resection is a good treatment option to remove these lesions, no matter the approach you choose by open surgery or full endoscopy the main objective is total resection. Of course, the endoscopic option is feasible, but we still need to develop more proper tools and endoscopes to turn this method as effective as the open surgical approaches. The future will respond to the feasibility of the security of these procedures as a safe tool to approach these lesions. The success of this treatment is well related to the learning curve and the personal experience of the spinal surgeon with spinal full endoscopy in his medical daily practice.
References
- Caspar W (1977) A new surgical procedure for lumbar disk herniation causing less tissue damage through a microsurgical approach. Adv Neuro surg 4: 74-80.
- Choi G, Lee SH, Raiturker PP, Lee S, Chae YS (2006) Percutaneous endoscopic interlaminar discectomy for intracanalicular disc herniation at L5-S1 using a rigid working channel endoscope. Neurosurgery 58(1 Suppl): ONS 59-ONS 68.
- Choi G, Lee SH, Lokhande P, Kong BJ, Shim CS (2008) Percutaneous endoscopic approach for highly migrated intracanal disc herniations by foraminoplastic technique using rigid working channel endoscope spine 33(15): E508-15.
- Choi G, Prada N, Modi HN, Vasavada NB, Kim JS (2010) Percutaneous endoscopic lumbar herniectomy for high grade down-migrated L4-L5 disc through an L5/S1 interlaminar approach atechnical note. Minim Invasive Neurosurg 53: 147-152.
- Choi G, Modi HN, Prada N, Ahn TJ, Myung SH, et al. (2013) Clinical results of XMR-assisted percutaneous transforaminal endoscopic lumbar discectomy. J Orthop Surg 8: 14-18.
- Destandau J (1999) A special device for endoscopic surgery of lumbar disc herniation. Neurolog Res 21: 39-42.
- Ditsworth DA (1998) Endoscopic transforaminal lumbar discectomy and reconfiguration: a poster-lateral into the spinal canal. Surg Neurolog 49(6): 588-598.
- Gelabert M, Agulleiro J, Reyes RM (2002) Spinal extradural angiolipoma with a literature review. Child Nerv Syst 18: 725-728.
- HijikataS, Yamagishi M, Nakayama T (1975) Percutaneos discectomy: A new treatment method for lumbar disc herniation. J Todenshop 5: 5-13.
- Ido K, Urushidani H (2001) Fibrous adhesive entrapment of lumbosacral nerve roots as a cause of sciatica. Spinal Cord 39(5): 269.
- Iones AA, Stambough JL, Balderston RA, Rothman RH, Booth RE (1989) Long term results of lumbar spinal surgery complicated by unintended incidental durotomy. Spine 14: 443-446.
- Jang JS, An SH, Lee SH (2006) Transforaminal percutaneous endoscopic discectomy in the treatment of foraminal and extraforaminal lumbar disc herniations. J Spinal Disord Tech 19: 338-343.
- Kambin P, Sampson S (1989) Posterolateral percutaneous suction-excision of herniated lumbar intervertebral disc. Report of interim results. Clin Orthop 207: 37-43.
- Kambin P (1990) Arthroscopy microdiscectomy: Minimal intervention spinal surgery. Baltimore, MD: Urban & Schwarzenberg, Germany.
- Knight MT, Ellison DR, Goswami A, Hillier VF (2001) Review of safety endoscopic laser foramonoplasty for the management of back pain. J Clin Laser Med Surgery 19(3): 147-157.
- Mayer HM (1993) Brock: Percutaneous Endoscopic Lumbar Discectomy (PELD). Neurosurg Rev 16(2): 115-120.
- Mixter W, Barr J (1934) Rupture of the intervertebral disc with involvement of the spinal canal. N Engl J Med 211: 210-215.
- Mathews HH (1996) Transforaminal endoscopic microdiscectomy. Neuro Surg Clin N Am 759-763.
- Onik G, Helms CA, Ginsburg L, Hoaglund FT, Morris J (1985) Percutaneous lumbar discectomy using new aspiration probe . AJR Am J Roentgenol 144: 1137-1140.
- Ruetten S, Komp M, Merk H, Godolias (2005) An extreme lateral access for the surgery of lumbar disk herniation inside the spina canal using the full-endoscopic uni portal transforaminal approach technique and prospective results of 463 patients. Spine 30(22): 2570-2578.
- Ruetten S, Komp M, Godolias G (2006) A new full-endoscopic technique for the interlaminar operations of lumbar disc herniations using a 6mm endoscopes: prospective 2-years results of 331 patients. Minimally Invasive Neurosurgery 49(2): 80-87.
- Ruetten S, Komp M, Merk H, Godolias G (2008) Full-Endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: A prospective randomized, contolled study. Spine 33(9): 931-939.
- Ruetten S, Komp M, Merk H, Godolias G (2009) Recurrentr disc lumbar herniation after conventional microdiscectomy: a prospective randomized study comparing full-endoscopic interlaminar and transforaminal versus microsurgical revision. J Spinal Disord Tech 22: 122-129.
- Panjabi MM, Krag MH, Chung TQ (1984) Effects of disc injury on mechanical behavior of the human spine: Spine 9: 707-713.
- Sentürk S, Ünsal ÜÜ (2019) Percutaneous full-endoscopic removal of lumbar intradural extramedullary tumor via translaminar approach. World Neurosurgery (125): 146-149.
- Schubert M, Hoogland T (2005) Endoscopic transforaminal nucleotomy with foraminoplasty for lumbar disk herniation. Oper Orthop Traumatol 17: 641-661.
- Smith L, Garvin PJ, GeslerRM, Jennings RB (1963) Enzyme dissolution of the nucleous pulposus. Nature 198: 1311-1312.
- Smith MM, Foley KT (1998) Micro Endoscopic Discectomy (MED): The first 100 cases Neurosurgery 43: 702.
- Stolke D, Sollmann W, Seifert V (1989) Intra and postoperative complications in lumbar disc surgery. Spine 14: 569.
- Stookey B (1927) Intradural spinal angiolipoma: report of a case and symptoms for 10 years in child age 11: Review of literature. Arch Neurol Psychiatry 18: 16-43.
- Spangfort EV (1972) The lumbar disc herniation: A computer-aided analysis of 2504 operations. Acta Orthop Scand Supp 142: 1-95.
- Yeung AT (1988) Minimally invasive disc surgery with the Yeung Endoscopic Spine System (YESS). Surgical Technology International 8: 267-277.
- Yeung AT, Tsou PM (2002) Posterolateral endoscopic excision for lumbardisc herniation: Surgical technique, outcome and complications in 307 consecutive cases. Spine 27(7): 722-731.
- Ying GY, Yao Y, Shen F, Ren YC, Chen CM (2017) Percutaneous endoscopic removal of a lumbar epidural angiolipoma via Interlaminar approach: A technical report. World Neurosurgery 99: 59-62.
© 2023 Marcio R Ramalho Cunha. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






