- Submissions

Full Text
Techniques in Neurosurgery & Neurology
Plasma Exchange for the Treatment of AQP4- IgG Positive Neuromyelitis Optica in Children: A Case And Literature Analysis
Yaoyuan Zhang, Liu Xue, Shen Peng, Zhiyuan Wang and Shujun Li*
Department of Pediatrics, First Affiliated Hospital of Xinxiang Medical University, China
*Corresponding author:Shujun Li, Department of Pediatrics, The First Affiliated Hospital of Xinxiang Medical University, No.88 of Jiankang road, Weihui, Henan province 453100, China
Submission: September 04, 2023;Published: September 15, 2023

ISSN 2637-7748
Volume5 Issue4
Abstract
Objective: This paper reports 1 case of a 14-year-old female patient diagnosed with NMOSD and reviews
related literature.
Methodology: A review of the patient’s clinical information, including medical history, signs, auxiliary
examination, treatment and follow-up, and a discussion of the documentation.
Result: The patient developed a digestive disorder and was eventually diagnosed with area postrema
syndrome as the initial manifestation of NMOSD. Initial application of hormones, human immunoglobulin
treatment poor effect, and then giving plasma replacement and other complex treatment to clinical relief.
Conclusion: The clinical manifestations of NMOSD are complex and rare in children. The first symptoms
of the gastrointestinal tract are rarer and can lead to misdiagnosis. In clinics, NMOSD is possible when
patients experience similar simpleness or stubbornness and are accompanied by vomiting. Plasma re
symptoms and rapy helps to eliminate disease-causing antibodies early, alleviate clinical symptoms, and
improve the degree of disability.
Introduction
Body fluid immunity plays a major role in the inflammatory dementia of the central nervous system caused by antigen-antibody-mediated Neuromyelitis Optica Spectrum Disorders (NMOSD). The majority of instances are in adolescent patients, with a preponderance of women and 3-5% in children [1]. A comprehensive NMOSD concept was introduced in 2015 by the International Panel for Neuromyelitis Optica Diagnosis (IPND). It includes layers of AQP4-IgG antibodies (AQP4 IgG) to establish a diagnostic criterion for the unknown status, as well as six Core Clinical Characteristics (CCC): optic neuritis, acute polio, area postrema syndrome, intervertebral syndrome, and Acute Cerebrospinal Syndrome (ACS) [2]. In the area where postrema syndrome is mostly caused by persistence and vice versa, as well as nausea, vomiting, and other gastrointestinal symptoms that can be misdiagnosed in the clinic, the condition is characterised by a high prevalence of disability, a high recurrence rate, and diversity. This article describes a 14-year-old female patient who was diagnosed with a gastrointestinal disease. It confirms that NMOSD is the first sign of area postrema syndrome. After a poor response to the initial hormone application, human immuno-globulin treatment, plasma replacement and other sophisticated therapies, patients get clinical relief. The following is a review of the literature and case studies.
Clinical Information
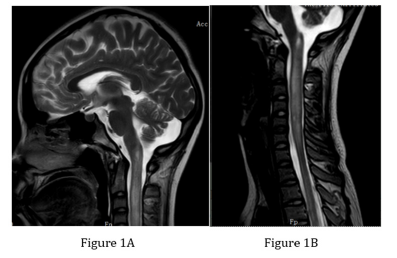
“Nausea, vomiting for 4 days” was the reason the 14-year-old patient was admitted to the hospital. Four days ago, there were seizures in the neck, body, and upper limb order, together with concurrently occurring independent tremors of the upper limb, nausea, vomiting, decreased hunger, poor eating, abdominal discomfort and concurrent hairy skin itching. Remain in the digestive region. Two weeks have passed since the disease’s spontaneous start, and the weight has dropped by about 1kg. No past, no family history, no personal history exists. Three days of treatment included alleviation from nausea and vomiting, headaches that kept coming back, neck pain, skin itching, and limb trembling. An MRI of the head revealed no obvious abnormalities. Long T1 / slightly longer T2 signal, such as knot shaped and striped T2, in the spinal cord of the lower lining of the neck, was seen on the cervical + thoracic MRI. Thin lines in the spinal cord of the chest 1-8 vertebrae (Figure 1), which are long T1 / somewhat longer T2 signals, are indicative of polio. The patient lost consciousness during sexual activity, had a pale face, a racing heartbeat, and was abruptly moved to the Intensive Care Unit (PICU) before recovering and developing a chubby heart rhythm. Physical assessment: W: 51kg, BP: 117/91mmHg, T: 36.3 °C, P: 75 times per minute, R: 20 times per minute. It’s obvious that the spirit is evil. Very little neck movement, huge circles and double-sided eyelids that are lightreflective eyelids are no obvious anomalies in the abdomen, heart, or lungs, although there is a minor depressurization of the cervical chest vertebrae.
Figure 1:Long T1 / slightly longer T2 signals in the spinal cord in the lower lining-neck segment are shown on Magnetic Resonance Imaging (MRI) of the cervical + thoracic vertebrae 3.0.
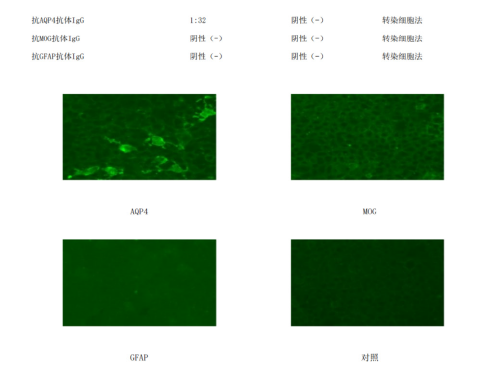
The neural system detects the presence of corneal reflection and the disappearance of abdominal wall reflection. Reduced pain perception, self-sensing skin itchiness, and regular pain in other areas characterize the feeling abnormality in the region between the first rib and the plain vertebrae. Tension in the muscles is normal; left upper limb muscles are 4 degrees, and the remaining limb muscles are 5 degrees. Position feeling is normal; light sensation (pain sensation) is present. Pathological reaction: Bipolar Babinski positive; physiological response: knee reflex, active back reflex. Cerebral stimulation: Kernig (-), straight neck (+) Glasgow scores: three points for wide eyes (during speech stimulation), five points for the best movement response (during local pain), and five points for the best speech response (during talk-oriented activities). EDSS 8.0, Expanded Disability Status Scale. Auxiliary examination: hemoglobin, electrolyte levels, liver and kidney function, blood glucose levels, ammonia levels, lactic acid levels, blood clotting capacity, arterial blood gas analysis, and immune levels five within normal limits. IIF positive (nuclear particle type), anti-Ro52kd antibody (LIA) positive, anti-ds-DNA(IIF), anti-microantibody (LIA), anti-ds-DNA (Lia), anti-protein antibody, anti-SmD1 antibody/LIA, anti-U1-snRNP antibody, and anti-SSB/R60 antibody are among the antibodies that are negative against neutrophilic cells and cell pulses and positive against thyroid cells. Analyze Drip 1:80 positive, Analyze 1:160 weak positive in the drip test. The range of the lymphatic subgroup is normal. The conventional Cerebro Spinal Fluid (CSF) has a colorless, bright, non-condensed, weak positive (±) nuclear cell count of 100×106/L and is classified as 20% polyleucocytes and 80% single nuclei. The fluid pressure is 170mmH2O.The biochemistry of the cerebral fluid is as follows: GLU 3.33mmol/L, ADA 2.00U/L, PRO 396.2mg/L, and Cl-119.0mmol/L. Immunoglobulin concentration in cerebrospinal fluid: 35.6mg/L. PCR-HSV-I negative cerebrospinal fluid; no ink colouring was detected. Negative cerebrospinal fluid culture results. Figure 2 shows serum anti-GFAP IgG positive, anti-MOG IgG negative, and anti-AQP4 IgG:1:32.
Figure 2:Indirect immunofluorescence from cell transplantation: IgG positive for antibodies against AQP4.
Clinical Diagnosis: NMOSD
Treatment passed
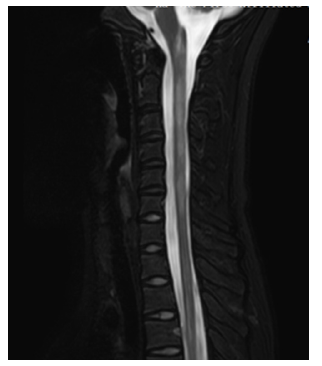
The administration of methamphetamine (0.5g, Q12H×5d) did not alleviate the symptoms. Leg anomalies, headache discomfort, and continuous usage of human immunoglobulin (20g, QD×5d) treatment tended to worsen. Magnetic Resonance Imaging (MRI) scan + improved results: apparent stripe-shaped, unevenly protracted T2 signal shadow in the mouth; vertebral thickening of the vertebrae of the dilated mouth-neck-chest 3 vertebrates (Figure 3). The results of the cerebrospinal fluid were reexamined: 140mm H2O of pressure, a negative Panzer test, 20 ×106/L of nuclear cell count, 0% polyleucocytes, and 0% single nucleic cells. The cerebrospinal fluid’s biochemistry is normal. Methamphetamine therapy should be continued for six days (0.5g, qd×3d, 0.25g and qd×3d). The chest region continues to hurt and there is also occasional headache, skin itching, limb freezing, a rise in nightmares, and delusions. The cerebral electrocardiogram showed no abnormalities. Results of the eye examination: the retinal blood vessels are in normal shape and proportion, the colour of the plates under the eyes is normal, the border is clear and there are no abnormalities in the yellow spots.
Figure 3:Cervical thoracic vertebrae 3.0 + enhanced Magnetic Resonance Imaging (MRI) showing thickening of the spinal cord and an unevenly longer T2 signal picture in the spine with visible stripes.
Perception
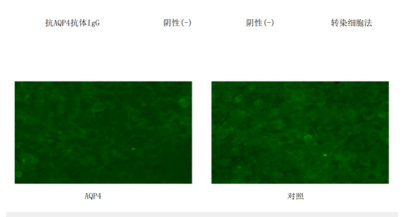
0.8 for each eye. Visual induction level: no anomaly on the right side and extended VEP-P100 on the left. Children’s clinical symptoms and imaging recommendations tend to worsen; the EDSS score increased to 8.5 points; the immunotherapy effect was poor; and the Plasma Exchange (PE) treatment (2700mL of sterilized plasma from the same virus, with a replacement time of 2.7 hours, blood pump speed of 120ml/min and splitting speed of 1000ml/h; once the following day, a total of 5 times) was used. Following the conclusion of physical education, the child’s headache gradually subsided, their neck pain greatly improved, they experienced no illusions or skin itching, and their limbs’ muscular strength returned to five degrees. Following assessment, serum anti-AQP4 antibodies were found to be negative (Figure 4).
Figure 4:Cell transplantation indirect immune fluorescence method: IgG negative to AQP4 anti bodies. Cell-based immunofluorescence technology (cell based transfection immuno fluorescence assay,CBA).
Discussion
In accordance with the “history of disease + core clinical
symptoms + image characteristics + biological markers” as the
basic diagnostic principle, the 2021 Guidelines for the Diagnosis
and Treatment of Diseases in the Spectra of Optic Polio in China
(hereinafter referred to as the “Guidelines”) stipulate that AQP4-
IgG positive patients (CBA testing method) must meet at least
one NMOSD core clinic characteristic, and other diseases can be
diagnosed after ruling out the diagnosis [3]. The girl in question
was a fourteen-year-old girl.
A. IgG-positive serum AQP4 (CBA test technique).
B. Three main clinical symptoms appear in acute polio,
region postrema syndrome and ocular neuritis.
C. An MRI scan reveals features similar to those of ocular
neuritis and polio; an MRI of the head shows no evidence of
brain lesions and an MRI of the spinal cord shows long-term
damage to the vertebrae from the pelvis to the chest, eliminating
Multiple Sclerosis (MS).
D. The identification of serum lacking anti-myelin
oligodendrocyte glycoprotein-IgG (MOG-IGG) antibodies.
E. With the exception of the high prevalence of MOGAD
in kids, NMOSD in kids with AQP4-IgG positive diagnoses is
evident and fits into the 8,0 (high subgroup) EDSS grade.
Acute therapy, continuing therapy (relapse prevention therapy), contraceptive therapy, and rehabilitative therapy are all part of the treatment for NMOSD. In order to reduce symptoms, enhance disability, accelerate the disease’s progression, and avert complications, acute therapy—which includes gluco corticosteroid shock therapy, intravenous injectable immunoglobulin, Plasma Exchange (PE), or Immuno Adsorption therapy (IA)—is an essential part of NMOSD therapy [3].Methamphetamine injections into veins aid in the restoration of neurological function and enhance vision; a dose of 1g/d is advised, with treatment lasting 3-5 days. The dose is then gradually lowered based on the patient’s condition and the length of time they need to take the medicine [4].
If high dosages of hormone shock are used with inadequate outcomes, then human immunoglobulin can be used to restore acute disability function [5]. Intravenous drip human immunoglobulin 0.4g/(kg.d), 5d is advised by the guidelines for a single course. Because the methamphetamine shock treatment was ineffective, the patient received one course of active human immunoglobulin therapy. According to the guidelines, “moderate-severe NMASD patients” was substituted for the prior phrase “some patients with severe NMOSD, especially those with poor response to high-dose methyl propionate shock therapy” in the PE application group. The guidelines state that immunosuppressive therapy does not necessitate blood plasma augmentation because it is a novel PE alternative therapy that can function similarly to PE and be administered in units that meet the necessary requirements. The status of PE in the treatment of NMOSD is confirmed when the evidence grade of PE/IA is raised to A recommendation [3]. The EDSS score increased by 8.5 points from 8.5, indicating poor efficacy of hormone and human immunoglobulin therapy, and considering the combined use of PE based on hormone maintenance. Six days after hormone shock therapy and the first round of human immunoglobulin treatment, the patient’s clinical performance worsened.
In order to replenish the extragenic plasma, the patient’s plasma is separated and disposed of using a plasma separator in the PE blood purification model. Large molecular components of blood plasma, including immunoglobulin, white protein, pathogens, and the intention behind disease therapy, will be eliminated during the removal process. The relative molecular mass size of the material to be eliminated from the blood, the pace at which proteins bind to them, the distribution of their solubility, etc. all influence the choice of PE mode. In cases of severe autoimmune disorders, antigen complexes are frequently eliminated from the blood using integrated blood purification schemes and plasma replacement [6,7]. The immunological globule protein AQP4-IgG has a relative molecular mass of about 150KD. Since AQP4-IgG cannot be eliminated by normal blood dialysis or blood flow patterns, it can only be eliminated by applying a plasma replacement pattern.
52 NMASD patients had 67 seizure occurrences examined in retrospective research of plasma replacement NMOSD acute seizures. The efficacy of IVMP and/or PE therapy was compared with the Extended Disability Status Score (EDSS) and Improved Rankin Scale (mRS). After PE therapy was discovered, it was discovered that 12 seizures responded well to hormone-combination PE therapies, whereas 16 seizures remained unresponsive to hormone-associated PE. Of the 28 seizures, none responded well to single-use hormone therapy. A 2020 meta-analysis of the timing of plasma replacement treatment for NMOSD found that plasma substitution was applied in 228 patients with NMOSD and the EDSS score was reduced by an average of 1.04 points after PE treatment. The study suggests that PE therapy should be considered for acute seizures in patients with ineffective NMOSD alone [8]. Patients who received PE treatment within 7 days of the disease’s beginning saw an average 0.64-point drop in their EDSS score. Patients receiving PE treatment between 8-23 days of commencement saw an average 1.41-point drop in their EDSS score. The meta-analysis found that PE helped those with severe NMOSD, and that the best time to begin PE was between 8 and 23 days [9]. However, all the cases that were included were adult cases, and no children were included.
In this instance, the pre-phase treatment recommended hormone shock therapy and human immunoglobulin therapy were ineffective. On the tenth day of the illness, PE was combined based on hormone maintenance and the child’s clinical symptoms significantly improved following the conclusion of the third round of plasma replacement therapy. Following five PE treatments, the patient’s headache, neck pain, and skin itching subsided and their ESDSS score improved to 7.0. Two days later, the serum anti-AQP4 antibodies (measured using the CBA test method) were reviewed, and the results were negative. After the patient’s condition showed signs of improvement, they were moved to the regular hospital to receive further care. According to the 2021 edition of the guidelines for NMOSD mitigation therapy, immunosuppressants should be increased in conjunction with RTX, satralizumab and low-dose hormones as advised in grade A, or they should be taken concurrently with RTX and low-dose hormones [3]. In this instance, the child chose oral sulfurine maintenance therapy, which has been followed for one month, and the condition is stable and does not reoccur because of family economic considerations combined with a tiny amount of hormone maintenance treatment.
Conclusion
The earliest clinical cases with gastrointestinal symptoms are more uncommon and are very prone to misinterpretation than the complex and rare clinical presentations of NMOSD in youngsters. Since the treatment of symptoms is not ideal, the clinical experience of patients with comparable simple or stubborn symptoms who also vomit suggests that the likelihood of NMOSD should be taken into consideration. Timely improvements in disease-specific tests, examinations, diagnosis assistance and early treatment are all important. Replacement therapy with plasma may lessen clinical symptoms, increase the degree of disability and help get rid of antibodies that cause the disease at an early stage. This was the situation for a single child, involving extensive clinical trials, extended follow-ups, and short follow-up times.
Fund Project
LHGJ20210519, a joint project of Henan Province Medical Science and Technology Research Program.
References
- Tenembaum S, Chitnis T, Nakashima I, Nicolas C, Andrew M, et al. (2016) Neuromyelitis optica spectrum disorders in children and adolescents. Neurology 87(9 Suppl 2): S59-66.
- Wingerchuk DM, Banwell B, Bennett JL, Philippe C, William C, et al. (2015) International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology 85(2): 177-189.
- Huang Dehui W, Hu Xueqiang (2021) Guidelines for the diagnosis and treatment of neuromyelitis optica spectrum disorders in China. Chinese Journal of Neuroimmunology and Neurology 28(6): 423-436.
- Guo S, Jiang H, Jiang L, Peng J, Wang J, et al. (2021) Factors influencing intravenous methylprednisolone pulse therapy in Chinese patients with isolated optic neuritis associated with AQP4 antibody-seropositive neuromyelitis optica. Sci Rep 11(1): 22229.
- Wu Yubi, Xia z (2018) Expert consensus on clinical application of plasmapheresis in children. Chinese Journal of Practical Pediatrics 33(15): 1128-1135.
- (2021) Consensus working group on the application of continuous blood purification in critical illnesses in children. Expert consensus on the application of continuous blood purification in critically ill children. Chinese Journal of Pediatrics 59(5): 352-360.
- Wang Z, Wang M (2020) Understanding of severe blood purification in pediatrics. China Blood Purification 19(12): 847-849.
- Srisupa OT, Siritho S, Kittisares K, Jiraporn J, Chanjira S, et al. (2018) Beneficial effect of plasma exchange in acute attack of neuromyelitis optica spectrum disorders. Mult Scler Relat Disord 20: 115-121.
- Huang X, Wu J, Xiao Y (2021) Timing of plasma exchange for neuromyelitis optica spectrum disorders: A meta-analysis. Mult Scler Relat Disord 48: 102709.
© 2023 Shujun Li. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






