- Submissions

Full Text
Techniques in Neurosurgery & Neurology
Severe Spine Cord Compression By Plasmacytoma/Multiple Myeloma, Series of Cases
Marcel Ṣincari1*, Francisco Cabrita1, Gabriel Pina2 and André Fernando Nunes3
1Marcel Ṣincari, Neurosurgery Department, Centro Hospitalar Tondela Viseu, Portugal
2Gabriel Pina, Orthopedic Department, Centro Hospitalar Tondela Viseu, Portugal
3André Fernando Nunes, Serviço de Neurocirurgia, Hospital Prenda, Luanda
*Corresponding author:Marcel Ṣincari, PhD, Neurosurgery Department, Centro Hospitalar Tondela Viseu, Portugal
Submission: July 31, 2023;Published: August 08, 2023

ISSN 2637-7748
Volume5 Issue4
Abstract
Multiple Myeloma (MM) is generally located in the Bone Marrow (BM) and associated with a wide spectrum of clinical, laboratory, and radiological findings [1]. Conversely, Solitary Plasmacytoma (SP) is characterized by a single mass of clonal plasma cells, with no or minimal BM plasmacytosis and with no other symptoms than those derived from the primary lesion [2]. The cases with spine involvement and spine cord suffering from compression always were very complicated and challenging.
Methods: We describe two cases of SP and MM with severe spine cord compression treated surgically
with indication to address the compression and stabilization of the affected segments with subsequent
treatment in hematology and oncology.
Results: In both cases the surgery was a success, the patient with SP survived 3 years and one month
and the patient with MM-1 year and 3 months.
Conclusion: Outcomes of surgical interventions for these patients with spine cord compression
and spinal instability due to multiple myeloma and plasmacytoma of the spine was with improved
neurological function following surgery and no instrumentation failure.
Keywords:Plasmacytoma; Myeloma; Spine
Abbreviations:MM-Multiple Myeloma; BM-Bone Marrow; SP-Solitary Plasmacytoma; SEP-Solitary Extramedullary Plasmacytoma; IMWG-International Myeloma Working Group
Introduction
Most patients with plasma cell neoplasia have generalized disease at diagnosis, i.e., Multiple Myeloma (MM). However, a minority (<5%) of patients with plasma cell malignancies present with either a single bone lesion, or less commonly, a soft tissue mass, of monoclonal plasma cells: Solitary Bone Plasmacytoma (SP) or Extramedullary Plasmacytoma (SEP) [3]. SP has a high risk of progression to MM and on Magnetic Resonance Imaging (MRI) examination at least 25% of patients with an apparent solitary lesion have evidence of disease elsewhere [4]. The primary treatment for most patients will be radiotherapy, but surgery may also be required, where close liaison among the hematologist, radiotherapist and surgeon is crucial for planning optimum care [3]. Solitary bone plasmacytoma has a male: female ratio of 2:1, with a median age of 55 years and primarily affects the axial skeleton especially the vertebrae [2].
The majority of patients with apparent SBP develop myeloma, with a median time to progression of 2 to 3 years, but MM has developed in a few patients as long as 15 years after radiotherapy [2]. Recommended diagnostic criteria for Solitary Bone Plasmacytoma (SBP) and Extramedullary Plasmacytoma (SEP): Single extramedullary mass of clonal plasma cells; Histologically normal marrow aspirate and trephine; Normal results on skeletal survey, including radiology of long bones; No anemia, hypercalcemia or renal impairment due to plasma cell dyscrasia; Absent or low serum or urinary level of monoclonal immunoglobulin [4]. It is recommended that SBP is treated with radical radiotherapy, encompassing the tumor volume shown on MRI with a margin of at least 2cm and treating to a dose of 40Gy in 20 fractions (grade B recommendation, based on level III evidence). For SBP >5cm, a higher dose of up to 50Gy in 25 fractions should be considered (grade C recommendation, based on level IV evidence). Radiotherapy remains the treatment of choice of the primary pathology and surgery is contra-indicated in the absence of structural instability or neurological compromise [4].
Multiple Myeloma (MM) is a plasma cell neoplasm that accounts for 1%-1.8% of all cancers and is the second most common hematological malignancy with an estimated incidence in Europe of 4.5-6.0/100 000/year [5]. It represents 10% of malignant hematologic neoplasms. This disease usually appears in the elderly, with a median age at diagnosis of 70 years and an incidence rate of 5.6/100,000 inhabitants per year. Its frequency is higher in males and African Americans [6]. Despite the significant improvement in patients’ survival over the past 20 years, only 10%- 15% of patients achieve or exceed expected survival compared with the matched general population [5]. The diagnostic criteria for multiple myeloma and related disorders have been updated by the International Myeloma Working Group (IMWG): Patients with 60% or more clonal plasma cell involvement of the marrow, serum free light chain ratio of 100 or higher (provided involved free light chain level ≥100mg/L), and/or greater than one focal lesion on MRI are defined as MM even in the absence of end-organ damage [1].
The revised IMWG criteria for MM permit the use of CT, low-dose whole-body CT, PET-CT, and whole-body CT to diagnose lytic bone disease in MM. One or more sites of osteolytic bone destruction of at least 5mm or more in size is required. Increased uptake on PET-CT alone is not adequate; there must be evidence of actual osteolytic bone destruction on the CT portion of the examination. A biopsy of one of the bone lesions should be considered if there is any doubt about the diagnosis. These changes will enable early and accurate diagnosis of MM. In addition to these changes, the IMWG clarified that the presence of osteoporosis, vertebral compression fractures, or bone densitometric changes in the absence of lytic lesions is not sufficient evidence of myeloma bone disease [1].
It is now generally accepted that bone pain can be alleviated by hemotherapy and/or radiotherapy; however, the effects of chemotherapy and/or radiotherapy are quite limited in MM patients with skeletal related events such as intractable pain, pathological fracture, spinal instability, spinal cord or nerve root compression and huge soft tissue masses. Such patients usually require surgical treatment. Thus, surgical procedures that are safe and effective in relieving pain and improving quality of life of patients with MM are playing an increasingly important role in the management of bone disease in these patients [7]. Chemotherapy remains the main form of therapy for MM, the trend being toward multidisciplinary cooperation. Orthopedic surgeons should improve the surgical procedures for myeloma bone disease and optimize perioperative management and physicians should consult with surgeons on patients with MM complicated by spinal instability, spinal cord compression or pathologic fracture [8].
Case 1
62 years old woman with a history of arterial hypertension, dyslipidemia, nodules of thyroid gland stables, colon polyps, presented with dorsal pain and legs weakness but able to walk assisted. ST scan and MRI of thoracic region showed severe collapse of Th2 vertebra by lithic lesion with spinal cord compression and regional initial kyphosis (Figure 1A). She was selected for surgical treatment: anterior cervical right-side approach with corpectomy Th2 and Th1-Th3 arthrodesis with mesh cylinder and anterior plate with cemented screws (Figure 1B). Postoperative CT scan reveals good spinal cord decompression and restoration of the height of Th3 collapsed vertebra with the same pattern on CT 1 year and 6 months after surgery. The pathologic anatomy result was Plasmacytoma/ Multiple Myeloma with restriction of kappa chain s. PET showed uptake in the parathyroid region, was biopsied, but with benign result. Treated by hematologist with first line: Cy Bord with VGPR, second line: Dara RD, third line Kd, fourth line: Pomalidomide and dexamethasone, last line with high hematological toxicity. The patient died 3 years and one month after surgery.
Figure 1:A: CT scan and MRI revealing Th2 pathological fracture with severe spinal cord compression.
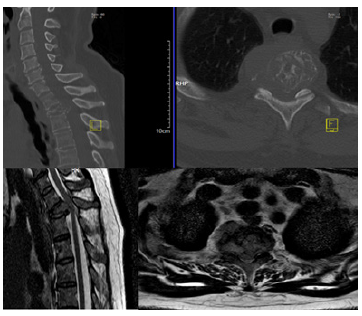
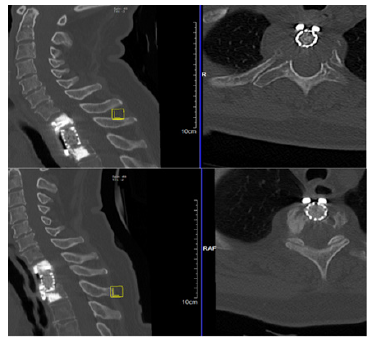
Figure 1b:Postoperative CT scan after corpectomy Th2 and reconstruction with mesh cylinder and anterior plate with cemented screws.
Case 2
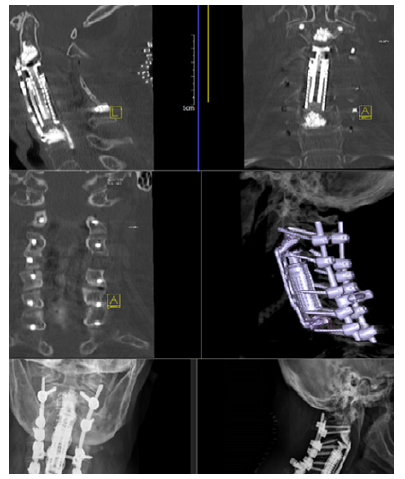
74 years old woman admitted for tetra paresis with a couple of weeks of evolution. Screening for primary tumor (Mammary and thyroid ECO, colonoscopy, MRI cholangiography, tumoral markers, IgM, IgG, IgA and lights chains, superior digestive endoscopy, medullar biopsy) was negative. CT scan and MRI of the cervical spine revealed lithic lesion of C3-C5 vertebral bodies with severe spinal cord compression and infiltration of the left lateral mass of C4 (Figure 2A). She was submitted to a two stage surgery during the same anesthesia, first was performed posterior fixation C2-C7 (C2 transpedicular, C3-C7 lateral mass on the right side, on the left side lateral mass C4 was skipped, it was removed because of tumoral infiltration), laminectomy C3-C5, removal of C4 left side lateral mass trough posterior medial approach and second anterior right side approach with corpectomy C3-C5, anterior arthrodesis C2-C6 with cylinder and anterior plate with cemented screws (Figure 2B). On the second postoperative day the patient suddenly worthened with respiratory insufficiency, the anterior cervical wound was opened in the ward with drainage of the hematoma, was intubated and revised in the operating room without discovering the hemorrhage source with subsequent good and uneventful recuperation. CT scan and X-Ray showed adequate decompression and good positioning of the fixation construction. The pathological anatomy result was Plasmacytoma/ Multiple myeloma with restriction of Kappa chains. PET revealed uptake in the proximal regions of both tibias and in the diaphysis of left femur bone. The first bone marrow biopsy was normal and 5 months later biopsy was hypercellular with plasmocytic infiltration, being half of the cellular count, marked exclusively by Kappa chains. Treated with CyBord in 6 cycles with bad toleration and radiotherapy. Presented rapid progression of the disease with multiple rib spontaneous fractures and deceased 1 year and 3 months after surgery.
Figure 2a:MRI revealing lithic lesion of C3, C4, C5 vertebral bodies infiltrating C4 left lateral mass with pronounced spinal cord deformation.
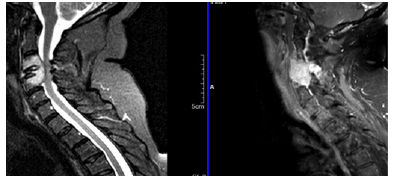
Figure 2b:Postoperative CT scan and X-Ray after corpectomy C3, C4, C5 and reconstruction with expansive cylinder, anterior plate with cemented screw and posterior fixation with cross link.
Discussion
The treatment of SP/MM involving the spine is medical, including radiotherapy, chemotherapy or both modalities. However, instability is the main reason for pain, which can only be relieved completely by surgery. Spinal stability was not considered an issue in SP because the vertebral body had compensated for the osteolytic defects by thickening its cortices [9]. The main indication was severe spinal cord compression with neurological motor deficit. The symptoms were relieved after surgery, and it permitted to reduce analgesic drug consumption and to maintain daily activity. Firm diagnosis should be made, including histological evidence of the lesion; complete skeletal survey; bone marrow examination, immunological as well as biochemical study.
According to R. Trivedi, in cases with cord compression from a soft tissue epidural tumor in multiple myeloma, the specific use of early surgical intervention improves neurological function and maintain stability. Surgery may play an important role in the treatment of selected patients with multiple myeloma [10]. Timely diagnosis and treatment are important in patients with spine cord compression caused by myeloma. In the absence of spinal instability and severe neural deficits, radiotherapy is often selected in combination with corticosteroids, to improve motor function and relieve pain [11].
Conclusion
Treatment of spinal SP/MM lesions will vary based on the degree of involvement of the vertebral body. A combination of radiation and surgical resection is the most common treatment. A pathologic compression fracture was found in up to 60% of myeloma patients [12]. Both cases had extensive vertebral body involvement with spinal cord compression and in one case with pathologic fracture of the affected vertebra. Good postoperative evolution was due to careful preoperative planning, adequate decompression and follow up of possible complications. According with the Portuguese Groupe of MM, despite the significant clinical gains obtained in recent years, the treatment of MM continues to be challenging, as it is multi-refractory, extramedullary disease with poor cytogenetic/molecular prognosis. Among the therapies that are expected to reach clinical practice in the coming years are CAR-Ts (Cell Therapies With Chimeric Antigen Receptor), bispecific antibodies, monoclonal antibodies conjugated with anticancer drugs, drug-conjugated peptides such as melflufen (melphalan flufenamide) and cereblon E3 ligase modulators (CELMoDs) [13].
Acknowledgement
To Mark-Daniel Şincari for helping with design arrangements.
References
- Rajkumar SV, Dimopoulos MA, Palumbo A, Joan B, Giampaolo M, et al. (2014) International myeloma working group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol 15(12): e538-e548.
- Dimopoulos MA, Moulopoulos LA, Maniatis A, Alexanian R (2000) Solitary plasmacytoma of bone and asymptomatic multiple myeloma. Blood 96(6): 2037-2044.
- Moulopoulos LA, Granfield CA, Dimopoulos MA, Kim EE, Alexanian R, et al. (1993) Extraosseous multiple myeloma: Imaging features. AJR Am J Roentgenol 161(5): 1083-1087.
- Richard S, Helen L, Graham J, Anthony R, Jenny B, et al. (2004) Guidelines on the diagnosis and management of solitary plasmacytoma of bone and solitary extramedullary plasmacytoma, 2004 United Kingdom Myeloma Forum. British Journal of Hematology 124(6): 717-726.
- Usmani SZ, Hoering A, Cavo M, Jesus S, Hartmut G, et al. (2018) Clinical predictors of long-term survival in newly diagnosed transplant eligible multiple myeloma IMWG research project. Blood Cancer J 8(12): 123.
- Walker RC, Brown TL, Jones JB (2012) Imaging of multiple myeloma and related plasma cell dyscrasias. J NuclMed 53(7): 1091-1101.
- Du X, Chen WM, Chen S (2013) The surgical treatment of multiple myeloma bone disease. People Health Press, pp. 50-59.
- The Surgeon's Committee of the Chinese Myeloma Working Group of the International Myeloma Foundation (2016) Consensus on surgical management of myeloma bone disease. Orthopedic Surgery 8: 263-269.
- Molloy S, Kyriakou C (2014) Expert's comment concerning grand rounds case entitled "total spondylectomy for solitary bone plasmacytoma of the lumbar spine in a young woman. A case report and review of literature. Eur Spine J 23(1): 40-42.
- Rishi Jayesh Trivedi (2021) Spinal cord compression because of spinal plasmacytoma in a patient with multiple myeloma: A case report. Clin Pract 11(1): 124-130.
- Bo Chen a, Lin Cai b, Fuling Zhou (2021) Management of acute spinal cord compression in multiple myeloma. Crit Rev Oncol Hematol 160: 103205.
- Mulligan M, Chirindel A, Karchevsky M (2011) Characterizing and predicting pathologic spine fractures in myeloma patients with FDG PET/CT and MR imaging. Cancer Investig 29(5): 370-376.
- João C, Rui B, Joana S, Celina A, Paulo B et al. (2023) Multiple myeloma treatment guidelines by the portuguese group of multiple myeloma. Acta Med Port 36(7-8): 517-526.
© 2023 Marcel Ṣincari. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






