- Submissions

Full Text
Techniques in Neurosurgery & Neurology
Acute Ischemic Stroke Followed by Acute Inferior Myocardial Infarction
Mohammed Habib* and Salama Awadallah
Cardiology Department, Alshifa Hospital, Gaza, Palestine, Israel
*Corresponding author: Mohammed Habib, Cardiology Department, Alshifa Hospital, Gaza, Palestine, Israel
Submission: November 21, 2022Published: December 09, 2022

ISSN 2637-7748
Volume5 Issue3
Abstract
Acute ischemic stroke the third cause of death in Palestine. The prevalence of coronary artery disease has been reported in one fifth of stroke patients. Although high risk of acute ischemic stroke after recent myocardial infarction has been reported in several clinical or observational studies. In this case report we describe successful treatment of patient with acute inferior ST elevation myocardial infarction followed by acute ischemic stroke.
Introduction
The incidence of Acute Ischemic Stroke (AIS) after recent Myocardial Infarction (MI) during the hospital stay ranges from 0.7% to 2.2% [1-3]. AIS occurred more frequently in the first days after Acute Myocardial Infarction (AMI), but incidence progressively decreased over time [3-5]. Brandi Witt et al. [6] suggested that during hospitalization for MI 11.1 the AIS occurred per 1000 MI compared with 12.2 in one month and 21.4 in one year. The most positive predictors of ischemic stroke after MI included: older age, hypertension, diabetes, history of previous stroke, history of anterior location MI, previous MI, atrial fibrillation and heart failure [6].
Case Report
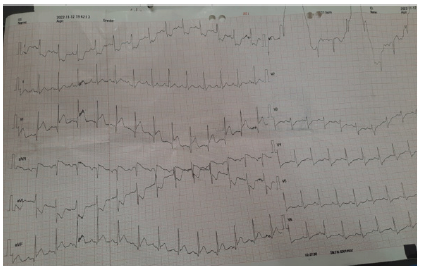
72 years old male patient, previously healthy with no chronic medical illnesses, presented complaining of acute burning retrosternal chest pain within two hours associated with diaphoresis and nausea. On examination, the patient was lying supine mildly anxious and sweaty. Blood Pressure: 142/90mmHg. Oxygen saturation on room air 95%, Pulse rate 105 beats per minute Temperature 37.6. Focused precordial exam: regular tachycardia with no added sounds. Back: normal vehicular breathing sounds with no crepitations. Electrocardiogram was done within 10 minutes and revealed ST segment elevation in inferior leads II, III, aVF with reciprocal ST depression in leads I, aVL (Figure 1).
Figure 1:ECG sinus tachycardia, inferior ST elevation.
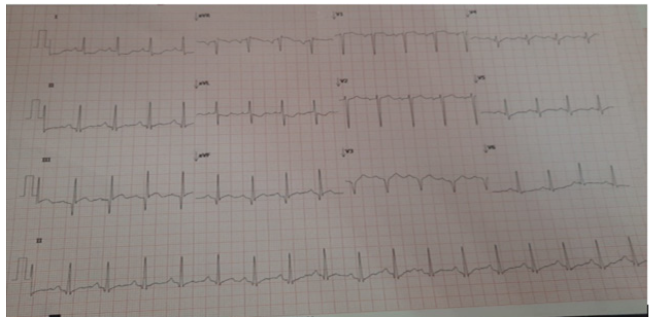
Because the patient arrived at the time window of thrombolytic strategy according to Al-Shifa Hospital protocol, thrombolytics was given rather than primary PCI. The patient was prepared before thrombolytics and was given 300mg loading Aspirin and 300mg loading clopidogrel, Streptokinase 1.5 million units over 60 minutes was given to the patient over 40 minutes in emergency department, then the patient was transferred to the coronary care unit with continuous ECG monitoring and defibrillator. After 90 minutes of giving streptokinase, ECG was done and showed more than 50% resolution of ST segment in inferior leads with great improvement of chest discomfort and symptoms by the patient (Figure 2).
Figure 2:ECG 90 minutes after streptokinase, ST resolution > 50%.
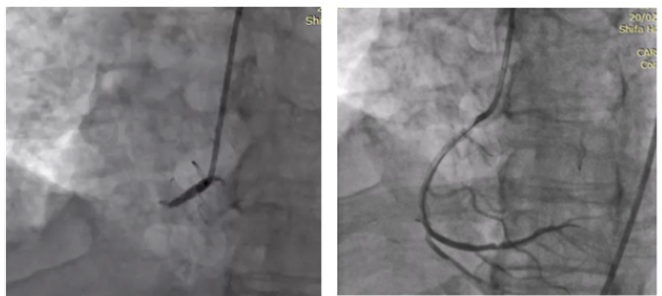
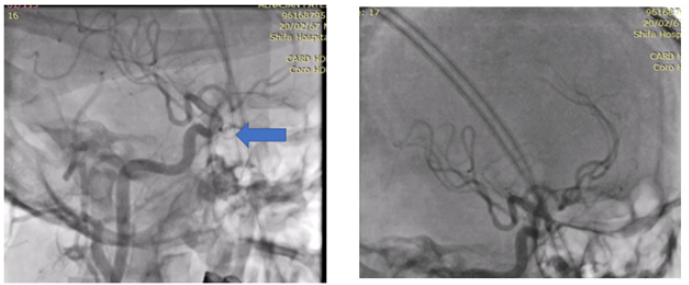
The day after that, the patient was transferred to the catheterization laboratory for pharmaco-invasive PCI and while sterilization process the patient suddenly developed difficult speech, weakness in the left arm and disorientation. Rapid coronary angiography by femoral access showed total occlusion of the mid right coronary artery and 2.75x26mm resolute stent (drug eluting stent) was deployment. At the same time, the interventional cardiologist went to cerebral circulation and on the screen appeared haziness in the right Middle Cerebral Artery (MCA). IA tPA 4mg was given into right MCA with TICI flow III. After 5 minutes he was able to speak fluently and move his left arm with full power and good consciousness level, after 48 hours the patient discharge from hospital without any complications.
Discussion
According to the 2018 guideline of scientific statement from the
American Heart Association/American Stroke Association (AHA/
ASA) [7]
A. For patients presenting with AIS and a history of recent
MI in the past 3 months, treating the ischemic stroke with IV
alteplase is reasonable if the recent MI was non-STEMI (Class
IIa).
B. For patients presenting with AIS and a history of recent
MI in the past 3 months, treating the ischemic stroke with IV
alteplase is reasonable if the recent MI was a STEMI involving
the right or inferior myocardium (Class IIa).
C. For patients presenting with AIS and a history of recent
MI in the past 3 months, treating the ischemic stroke with IV
alteplase may reasonable if the recent MI was a STEMI involving
the left anterior myocardium. (Class IIb) The main concerns
about giving rt-PA to patients with AIS and history of recent MI
are (Beyond the bleeding): 1.Thrombolysis-induced myocardial
hemorrhage predisposing to myocardial wall rupture 2.
Possible ventricular thrombus that could be embolized because
of thrombolysis. 3-post-myocardial infarction pericarditis
that may become hemopericardium the safety of IV rt-PA for
Acute Ischemic Stroke (AIS) treatment after recent Myocardial
Infarction (MI) is still controversial. In recent Retrospective
review article of 102 AIS patients admitted for AIS with history
of recent MI in the previous 3 months.
Patients according to treated with standard IV rt-PA dose for AIS were divided into 2 groups: treated or not treated. Four patients with STEMI patients in the week preceding ischemic stroke (8.5%) and IV rt-PA treated died from confirmed cardiac rupture/ tamponade. This complication occurred in 1 (1.8%) patient in the nontreated group (P=0.178), and no non-STEMI patients receiving IV rt-PA had cardiac complications [8]. The new recommendation according to 2021 guidelines of European Stroke Organization (ESO) on intravenous thrombolysis for acute ischemic stroke suggested that (14): Contraindication of rt-PA For patients with acute ischemic stroke of <4.5h duration and with history of subacute (>6h) ST elevation myocardial infarction during the last seven days. Insufficient evidence to make a recommendation for patients with acute ischemic stroke of <4.5h duration and with history of ST-elevation myocardial infarction of more than a week to three months. IV rt-PA for patients with acute ischemic stroke of < 4.5 h duration and with a history of non-ST-elevation myocardial infarction during the last three months (Figure 3).
Figure 3:a: Mid RCA totally occluded; b: patent RCA after stent deployment.
The recent retrospective trial among 40 396AIS patients with age ≥65 years, the patients treated with rt-PA were 241 patients (0.6%) had recent MI in the past 3 months, of which 19.5% (41 patients) were ST-segment-elevation myocardial infarction. Patients with recent MI had more severe stroke than those without. Among older patients receiving rt-PA for AIS, a recent history of MI in the past 3 months was associated with higher in hospital mortality compared with no history of MI in ischemic stroke patients treated with rt-PA (Figure 4). This association was more prominent in patients with STEMI than those with NSTEMI. This association was not significant, if the time frame from the onset of MI to the indexed AIS was >3 months [9]. Despite the increasing risk of mortality, further studies are necessary to determine whether the benefit of rt-PA outweighs its risk among AIS patients with a recent history of MI in last 3 months.
Figure 4:a: haziness in the Right MCA; b: TICI flow III in right MCA.
According to Alshifa hospital classification this is type II cardio cerebral infarction syndrome and diagnosis AIS (a sudden onset of focal neurological deficit caused by an cerebral vascular narrowing cause) and recent history of MI (acute elevation cardiac enzyme plus ischemic electrocardiogram changes and/or symptoms) in the previous 3 months but not in first 12 hours from MI. and the causes may be Left ventricle thrombus formation or Increased coagulation activity or The circulatory inflammatory cytokines or Post myocardial infarction atrial fibrillation/atrial flutter or Intervention of myocardial infarction (PCI and CABG) [10].
Conclusion
Type II cardio cerebral infarction syndrome is one of the most challenging medical emergency conditions and requires timely management. Therapeutic strategies and efficient teamwork among neurologists and cardiologists are required for ideal management for such exceptional cases. We believe that invasive treatment using mechanical thrombectomy for cerebral arteries and PCI to culprit coronary artery must be done. Future clinical trial study, though difficult to perform due to its rarity, is required in order to develop the optimal management of this catastrophic clinical scenario.
References
- Al Suwaidi J, Al Habib K, Asaad N, Singh R, Hersi A, et al. (2012) Immediate and one-year outcome of patients presenting with acute coronary syndrome complicated by stroke: Findings from the 2nd Gulf Registry of Acute Coronary Events (Gulf RACE-2). BMC Cardiovasc Disord 12: 64.
- Longstreth WT, Litwin PE, Weaver WD (1993) Myocardial infarction, thrombolytic therapy, and stroke. A community-based study. The MITI Project Group. Stroke 24(4): 587-590.
- Kajermo U, Ulvenstam A, Modica A, Jernberg T, Mooe T (2014) Incidence, trends, and predictors of ischemic stroke 30 days after an acute myocardial infarction. Stroke 45(5): 1324-1330.
- Mooe T, Olofsson BO, Stegmayr B, Eriksson P (1999) Ischemic stroke. Impact of a recent myocardial infarction. Stroke 30(5): 997-1001.
- Brammås A, Jakobsson S, Ulvenstam A, Mooe T (2013) Mortality after ischemic stroke in patients with acute myocardial infarction: Predictors and trends over time in Sweden. Stroke 44(11): 3050-3055.
- Witt BJ (2006) The incidence of stroke after myocardial infarction: A meta-analysis. The American Journal of Medicine 119(4): 354.
- Berge E, Whiteley W, Audebert H, De Marchis GM, Fonseca AC, et al. (2021) European Stroke Organisation (ESO) guidelines on intravenous thrombolysis for acute ischaemic stroke. European Stroke Journal 6(1): 1-101.
- Collet JP, Thiele H, Barbato E, Barthélémy O, Bauersachs J, et al. (2021) 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. European Heart Journal 42(14): 1289-1367.
- Mehran R, Bode C, Halperin J, Verheugt FW, et al. (2016) Prevention of bleeding in patients with atrial fibrillation undergoing PCI. N Engl J Med 375(25): 2423-2434.
- Habib M (2021) Cardio-Cerebral Infarction Syndrome (CCIS): Definition, diagnosis, pathophysiology and treatment. Cardiology and Cardiovascular Research 5(2): 84-93.
© 2022 Mohammed Habib. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






