- Submissions

Full Text
Techniques in Neurosurgery & Neurology
Complicated Epitympano-Mastoid Cholesteatoma With Intracranial Involvement: Tenets for A Modern Multidisciplinary Management
Edoardo Agosti1,2,3*, Graziano Pavan4, Antonio Tabano2,Francesco D Amore5,Armela Gorica4,Gabriele Vinacci5,Andrea Giorgianni5,Sergio Balbi2,3,Paolo Castelnuovo3,4,Davide Locatelli2,3,Marco Maria Fontanella1
1Department of Medical and Surgical Specialties, University of Brescia, Italy
2Department of Biotechnology and Life Sciences, University of Insubria, Italy
3Research Center for Pituitary Adenomas and Saddle Pathology, University of Insubria, Italy
4Division of Otorhinolaryngology, Department of Biotechnology and Life Sciences, University of Insubria, Varese, Italy
5Department of Neuroradiology, ASST Sette Laghi, University of Insubria, Italy
*Corresponding author: Edoardo Agosti, Division of Neurosurgery, Department of Biotechnology and Life Sciences, University of Insubria, Ospedale di Circolo e Fondazione Macchi, Varese, Italy
Submission: October 07, 2022;Published: October 19, 2022

ISSN 2637-7748
Volume5 Issue3
Abstract
Cerebral abscess is becoming a rarer complication of cholesteatoma. In this study we report a sporadic right cholesteatoma with intracranial diffusion and cerebral abscess, highlighting the innovations of the neuroimaging study, and pitfalls, tips, and tricks of its surgical management. We revised a multicentric retrospective registry of patients with complicated cholesteatomas and an exemplary case for the modern multidisciplinary management of complicated cholesteatomas is described. A 77-year-old female was admitted to our hospital for right facial nerve palsy (House-Brackmann type 4), painful irradiation of the right half face, and ipsilateral hearing loss. Neuroimaging diagnostic classification revealed right temporal cerebral abscess related to inner ear cholesteatoma with tegmen tympani erosion. Stereotaxic neuronavigational-assisted drainage of the right temporal brain abscess and microscope-assisted radical mastoidectomy and epitympano-mastoid cholesteatoma exeresis were performed. A regular clinical and radiological follow-up demonstrated regression of the facial nerve palsy and aesthetic improvement, complete reclamation of the cerebral abscess cavity without signs of residual parenchymal inflammation, and total removal of the cholesteatoma in the absence of disease recovery. Preoperative treatment with new generations of antibiotics and lesion studies with advanced neuroimaging techniques have renewed the diagnostic and therapeutic approach to massive intracranial complicated cholesteatoma. The multidisciplinary planning, the choice of the appropriate surgical approach, and the microscopicassisted dissection are mandatory for a disease-safe removal, abating the risk of surgical complications and pathology recurrences.
Keywords: Spinal; Cystic; Tumor; Extradural; MR tractography; Mc-Cormick scale; Perineural; Cyst; Frankel ACDF
Abbreviations: CT: Computed Tomography); ICs: Intracranial Complications; MRI: Magnetic Resonance Imaging; TgT: Tegmen Tympani)
Introduction
Cholesteatoma is a benign lesion of the middle ear consisting of keratinizing epithelium that proliferates and undergoes internal desquamation. While acquired cholesteatoma usually arises in the middle ear due to chronic disease, primary or congenital cholesteatoma is thought to originate from residual embryological epithelial tissue, and it can appear in the mastoid, petrous or tympanic portion of the temporal bone [1]. Bone erosion is a common finding in cholesteatoma. Indeed, although it is a benign lesion, it could lead to erosion of the otic capsule, facial nerve canal, ossicles, Tegmen Tympani (TgT), and tegmen antri [2]. The cholesteatoma growth can lead to the invasion of end temporal and intracranial structures [3]. Complications can be extracranial (i.e., ossicular damage, mastoid abscess, facial nerve palsy, exposed sigmoid sinus, labyrinthine fistula, Bezold abscess) and Intracranial (ICs) (i.e., meningitis, brain abscess, sigmoid sinus thrombosis). A multidisciplinary evaluation and management with a team of otolaryngologists, neurosurgeons and infectious disease specialists is required for its treatment [4]. Timing of intracranial abscess drainage and management of the otogenic focus is still debated [5,6]. We revised a multicentric retrospective registry of patients with complicated cholesteatomas and selected 7 patients with complicated cholesteatoma associated with intracranial abscess. Among these patients, we describe the case of sporadic right cholesteatoma with right petrous bone erosion and development of a temporal intracranial abscess, highlighting the peculiarities of the neuroradiological study images, and the criticalities and pitfalls of the therapeutic management (surgical and pharmacological).
Case Report
The study was performed in compliance with the Helsinki Declaration. The patient involved in the study signed a consent form to publish their clinical photographs whenever useful.
History and examination
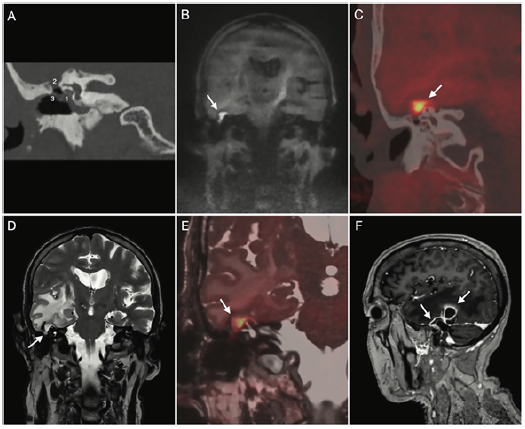
A 77-year-old female was admitted to our hospital for threeweek onset of asthenia associated with right facial nerve palsy (House-Brackmann type 4), painful irradiation of the right half face and ipsilateral hearing loss. Head Computed Tomography (CT) scan showed a right temporo-parietal ipodensity with perilesional edema and contralateral right ventricle shift was shown; additionally, a mastoid-CT highlighted the presence of bone erosion and thinning of the right TgT and right ossicular chain (Figure 1). Ot microscopy revealed a right myringosclerosis without otorrhea or perforation, with scutum erosion and presence of cholesteatoma. The audiological evaluation showed a severe right mixed hearing loss and a mild left sensorineural hearing loss. A Magnetic Resonance Imaging (MRI) highlighted a right temporal abscess surrounded by edema and adjacent signal changes in the tympanic cavity (Figure 1). Given the pronounced edema and the patient incipient confusion, antiedematous drugs (mannitol 18% 60ml x 6 / day iv, dexamethasone 8mg x 2 / day iv) were administered to the patient. A collegial discussion between otolaryngologists, neurosurgeons and neuroradiologists led to the diagnosis of right temporal otogenic abscess consequent to epitympano-mastoid cholesteatoma with TgT erosion and extradural intracranial spread and a shared therapeutic strategy was achieved.
Figure 1:Pre-surgical imaging. (A) CT coronal reformat, right temporal bone: soft tissue filling the tympanic cavity
with ossicular chain and facial nerve canal (tympanic segment) erosion with mildly eroded otic capsule and preserved
bony walls of semicircular canals (1), focal resorption of the tegmen tympani/antri (2) and eroded scutum (3). (B) DW
non-EPI coronal plane: diffusion restricting (bright) mass originating from the middle ear and abutting the middle
cranial fossa. (C) CT plus DW non-EPI fusion, coronal plane: relationship between the eroded tegmen tympani and the
intracranial component (bright yellow) of the cholesteatoma. (D) coronal T2: cholesteatoma (arrow) displacing upwards
the temporal gyri; there is a vast digitiform temporal edema and mass effect distorting the ipsilateral ventricle. (E) thin
section high resolution T2 plus DW non-EPI fusion, coronal plane, showing the relationship between the cholesteatoma
(bright yellow) and semicircular canals, normal in signal and morphology, and the displaced dura (white arrow). (F)
sagittal contrast-enhanced T1: thickened dura (white arrow) overlying the intracranial portion of the cholesteatoma
(non-enhancing) with an adjacent posteriorly located intraparenchymal ring enhancing lesion consistent with abscess
surrounded by subcortical hypointense changes in keeping with edema. Abbreviation: CT, computed tomography; DW
non-EPI, diffusion weighted non-echo planar imaging.
Surgical treatment
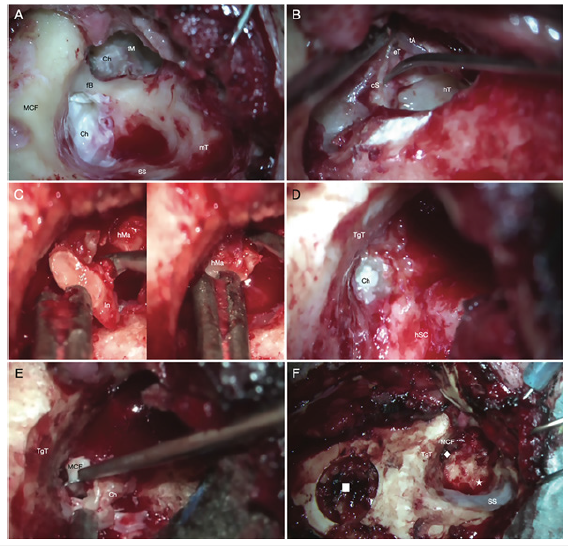
Stereotaxic neuronavigational-assisted drainage of the right temporal brain abscess was performed immediately. After 5 days, once the patient clinical condition had stabilized, a combined ENTneurosurgical procedure was performed: microscope-assisted radical mastoidectomy and epitympano-mastoid cholesteatoma exeresis, surgical enlargement of TgT erosion and excision of the intracranial portion of cholesteatoma. No liquorrhea was detected throughout the procedure. After all the cholesteatoma has been removed macroscopically, the auditory tube was swabbed, and the surgery cavity was obliterated with autologous abdominal fat. Finally, the external auditory canal was closed according to the “cul de sac” technique. Throughout the entire procedure, the facial nerve was constantly monitored (NIM® Nerve Monitoring Systems, Medtronic). The main steps of ENT-neurosurgical combined cholesteatoma removal are detailed in Figure 2. The histopathological examination of the excised material described horny lamellae focal dystrophic calcifications coherent with cholesteatoma. The cultural exam of the abscess isolated a methicillin-resistant Staphylococcus Aureus.
Figure 2:Main surgical steps of combined ENT-neurosurgical cholesteatoma removal. (A) scutum erosion and spread
of cholesteatoma from the epitympanum to the mastoid; the pars tensa of the tympanic membrane is intact and
adheres to the stapes. (B) removal of the facial bridge and cholesteatoma, with exposure of the matrix covering the
ossicular residues of the anvil; elevation of the tympanic annulus which is attached to the capitulum of the stapes; the
stapes is delicately dissected from the tympanic adhesions; mesotympanum and hypotympanum are not infiltrated
by cholesteatoma. (C) removal of incus residue and head of the malleus. (D) erosion of the tegmen tympani with
intracranial passage of the cholesteatoma. (E) exeresis of intracranial cholesteatoma with widening of the bone link
at the level of the tegmen tympani. (F) after widening of the bone link (rhombus), complete removal of the intracranial
portion of cholesteatoma occurs; the epitympano-mastoid surgical cavity (star) is also macroscopically disease-free;
below on the left we see the transcranial neurosurgical access (square) used for the drainage of temporal abscess.
Abbreviation: Ch, cholesteatoma; cS, capitulum of the stapes; eT, epitympanum; fB, facial bridge; hM, head of the
malleus; hSC, horizontal semicircular canal; hT, hypotympanum; MCF, middle cranial fossa; In, incus; mT, mastoid
tip; tA, tympanic anulus; TgT, tegmen tympani; tM, tympanic membrane.
Postoperative course
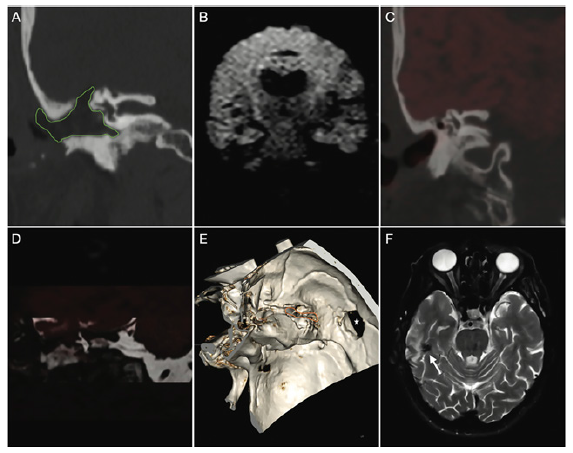
The patient underwent antibiotic therapy with Linezolid 600mg x 2 / die for ten days and then switched to Bactrim 160mg / 800mg x 2 / die for other ten days. A two-day post-operative CT showed regular surgical outcomes. The patient was discharged 5 days after the second surgery. A regular clinical and radiological follow-up was executed. One month and two-month clinical followup confirmed the regular postoperative course with a right facial nerve palsy residual (House-Brackmann type 2). A six-month postoperative MRI demonstrated regular evolution of the surgical site in the absence of residual cholesteatoma (Figure 3).
Figure 3:Post-surgical imaging follow-up. (A) CT coronal reformat: radical mastoidectomy with autologous fat graft
(green shape). B, C and D: no evidence of residual cholesteatoma. (B) coronal DW non-EPI in coronal view; this
technique allows for higher spatial resolution and less conspicuous artifacts at the bone-air interfaces. (C) coronal CT
plus DW non-EPI fusion. (D) coronal T2 plus DW non-EPI fusion. (E) CT 3D-VR reformat showing surgical access to the
middle cranial fossa (asterisk) and surgical tegmen remodeling (orange circle) status post cholesteatoma resection. (F)
axial T2: postsurgical parenchymal changes (white arrows). Abbreviation: 3D-VR, 3D-volume rendering; CT, computed
tomography; DW non-EPI, diffusion weighted non-echo planar imaging.
Discussion
In this work we presented the case of a right temporal cerebral abscess related to inner ear cholesteatoma shedding light on the innovative surgical and diagnostic techniques for setting and managing the diagnostic-therapeutic process of this cerebral otological complication which is infrequent in current clinical practice. The proximity among infratemporal (middle ear cleft and mastoid air cells) and intracranial compartments, combined with the presence of thin layers of bone to divide extracranial and intracranial districts, is the anatomical basis for the diffusion of phlogistic and infectious processes to the meninge-cerebral structures from middle ear affections. Among the ICs, meningitis (15%-19%) and cerebral abscess (12%-15%) are the most common. Otogenic abscess localize homolaterally to the otogenic focus at the temporal (54%), cerebellar (44%), or both (2%) levels [7].
Currently, a lower incidence of cholesteatoma related cerebral abscesses has been reported due to the targeted chronic ear treatment with new generation antibiotics, early diagnosis of ICs (increased availability of CT and MRI), and earlier referral to tertiary centers. The low frequency of cholesteatoma related ICs has led to a difficulty in defining surgical therapeutic protocols (single or combined approach, endoscope- or microscope-assisted) [8]. The aim of therapy is radical surgery to completely remove the lesion with minimal morbidity. The balance achievable between postoperative morbidity and radical dissection should be carefully assessed, and surgery should be performed according to the principles of skull base microsurgery. Several cases of cholesteatoma with temporal abscess are described in the literature, but a common opinion on surgical treatment strategies and timings is still lacking among the authors [1].
Regarding treatment timings, several authors recommended performing otological surgery at the same time as drainage of the intracranial abscess. In our experience, two-stage management of the brain abscess and otogenic focus is the safest route. Priority must be given to the abscess drainage, since between the two the pathology is more urgent and more at risk of evolution. In this way the aggressiveness of the single surgical procedure is reduced, the patient is given time to recover, and the type of mastoidectomy is pondered based on the possible permanence of the abscess residue. Some authors propose a single surgical approach using radical mastoidectomy with enucleation of the cholesteatoma and drainage of the cerebral abscess by otogenic route. In favor of single surgical access, there is less surgical aggression and shorter hospitalization times. In our experience aspiration of intracranial abscess of otogenic origin by subtemporal transcranial burr hole approach and concurrent mastoidectomy allows to dominate more infectious collection, especially in case of medial and anterior extension of the abscess; conversely, performing a single stage otogenic surgical access is at greater risk of leaving intracranial abscess residues.
Furthermore, even regarding the reconstructive phase there are no common guidelines, and some authors do not perform simultaneous obliteration of the mastoid and/or tympanoplasty. In the case described here, in consideration of the severe ipsilateral hearing loss, the patient’s age, the size of the brain abscess (2.2 x 1.7 x 1.5cm), the extent of the TgT post-surgical bone defect, and the possible post-surgical infectious complications, an oto-mastoid obliteration was performed. Indeed, the obliteration of the surgical cavity reduces the risk of surgical cavity over infection due to a greater hermetic closure of the surgical access route. Moreover, the use of post-operative antibiotic therapy has a role both in reclamation of the abscess cavity and in prophylaxis of reinfection of the surgical site.
The use of microscope- and endoscope-assisted techniques has certainly contributed to improving surgical results, simultaneously reducing the risk of post-surgical residues and damage to neurovascular structures. The endoscope-assisted procedure is especially useful in the drainage of otogenic temporal and cerebellar abscesses with medial extension, ensuring greater vision with less stretching of the neurovascular structures. The microscope plays an essential role in infratemporal dissection, to preserve the facial nerve, the structures of the inner ear and avoid fissuring of the sigmoid sinus walls. In the case reported here, optical fibers and endoscope-assisted techniques were not used, preferring to exploit the magnification offered by the microscope for removal both of the extra-and intracranial part of the cholesteatoma.9 Finally, the neuroimaging techniques used in this case played a decisive role in guiding the diagnostic and therapeutic process. CT and diffusion weighted non-echo planar imaging (DW non-EPI) fused images increase further the diagnostic accuracy by reliably localizing cholesteatoma and its relationship to critical structures [9-11].
Conclusion
We described the multidisciplinary management of cholesteatoma with TgT erosion, intracranial extension and related temporal lobe abscess, demonstrating the advantages of an innovative neuroimaging study and a combined ENTneurosurgical approach. The multidisciplinary planning, the choice of the appropriate surgical approach, and the microscopic-assisted dissection are mandatory for a disease safe removal, abating the risk of surgical complications and pathology recurrences or remnants.
References
- Cazzador D, Favaretto N, Zanoletti E, Martini A (2016) Combined surgical approach to giant cholesteatoma: A case report and literature review. Ann Otol Rhinol Laryngol 125(8): 687-693.
- Habesoglu TE, Balak N, Habesoglu M (2009) Intracranial cholesteatoma-case report and critical review. Clinical Neuropathology 28(6): 440-444.
- Musharaf M, Ajmal M, Saeed I, Fatima S (2011) Prevalence of cholesteatoma and its complications in patients of chronic suppurative otitis media. Journal of Rawalpindi Medical College (JRMC) 15(1): 16-17.
- Smith JA, Danner CJ (2006) Complications of chronic otitis media and cholesteatoma. Otolaryngol Clin N Am 39(6): 1237-1255.
- Duarte MJ, Kozin ED, Barshak MB (2018) Otogenic brain abscesses: A systematic review. Laryngoscope Investig Otolaryngol 3(3): 198-208.
- Alaani A, Coulson C, McDermott AL, Irving RM (2010) Transtemporal approach to otogenic brain abscesses. Acta Otolaryngol 130(11): 1214-1219.
- Sennaroglu L, Sozeri B (2000) Otogenic brain abscess: Review of 41 cases. Otolaryngol Head Neck Surg 123: 751-755.
- Morwani KP, Jayashankar N (2009) Single stage, transmastoid approach for otogenic intracranial abscess. J Laryngol Otol 123(11): 1216-1220.
- Orhan KS, Çelik M, Polat B (2019) Endoscope-assisted surgery for petrous bone cholesteatoma with hearing preservation. J Int Adv Otol 15(3): 391-395.
- Locketz GD, Li PM, Fischbein NJ, Holdsworth SJ, Blevins NH (2016) Fusion of computed tomography and propeller diffusion-weighted magnetic resonance imaging for the detection and localization of middle ear cholesteatoma. JAMA Otolaryngol Head Neck Surg 142(10): 947-953.
- Sharma SD, Hall A, Bartley AC, Bassett P, Singh A, et al. (2020) Surgical mapping of middle ear cholesteatoma with fusion of computed tomography and diffusion-weighted magnetic resonance images: Diagnostic performance and interobserver agreement. Int J Pediatr Otorhinolaryngol 129: 109788.
© 2022 Edoardo Agosti. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






