- Submissions

Full Text
Techniques in Neurosurgery & Neurology
Spinal Extradural Arachnoid Cyst of the Thoracic Spinal Cord in a Child
Aliev MA*, Rajabov Kh, Mamadaliev AM, Kholmurodova Kh
Department and Clinic of Neurosurgery of Samarkand State Medical University, Uzbekistan
*Corresponding author: Aliev MA, Department and Clinic of Neurosurgery of Samarkand State Medical University, Samarkand, Uzbekistan
Submission: August 01, 2022;Published: August 25, 2022
ISSN 2637-7748
Volume5 Issue2
Annotation
Extradural neoplasms, especially those arising from the thoracic spinal cord, are rare in children. In our case, the patient is a 3-year-old child with a spinal extradural arachnoid cyst of the spinal cord at the level of VTh6-8. Neuroroentgenological signs indicated a cystic extradural tumor at the level of 6-8 thoracic vertebrae of the spine and spinal cord, which was later confirmed by histopathological findings. The patient was diagnosed with neurological deficits according to the McCormick scale-3 degrees and according to the Frankel scale-C in the preoperative period. An operation was performed-”VTh7 and VTh8 hemilaminectomy, total removal of an extradural cystic tumor. “In the postoperative period, neurological deficits regressed from grade 3 to grade 1 on the Mc-Cormick scale and from type “C” to “E” on the Frankel scale.
Output Extradural cystic neoplasms are benign tumors. Total resection with a positive clinical outcome can be achieved with minimal risk.
Keywords: Spinal; Cystic; Tumor; Extradural; MR tractography; Mc-Cormick scale; Perineural; Cyst; Frankel ACDF
Introduction
The incidence of spinal tumors is 1,1 per 100,000 populations. Spinal cord tumors are a relatively rare diagnosis and account for 1 to 10% of all tumors of the central nervous system in children [1-12]. Among primary tumors, extramedullary ones predominate, which occur in 70-90% of cases of the total number of these types of neoplasms. The incidence of extramedullary tumors is 1,3 cases per 100 000 populations per year, approximately 75% of tumors are intradural, 10% paravertebral, and the rest (15%) extradural [3]. Spinal arachnoid cysts are a heterogeneous group of formations, including cysts with different mechanisms of formation and location. The modern morphological classification of spinal arachnoid cysts, proposed by Nabors [8], contributed to the unification of heterogeneous formations combined within this diagnosis, including three types: 1st type: Extradural cysts that do not contain nerve fibers. 1A: extradural arachnoid cysts. 1B: sacral meningocele. 2nd type: Extradural cysts containing nerve fibers, Perineural cysts (Tarlov’s cysts); Meningeal diverticula. 3rd type: Intradural cysts.
It should be noted that spinal arachnoid cysts, regardless of their relation to any type, can be congenital or acquired. The formation of the latter may be based on trauma, infection, hemorrhage, or the consequences of surgery. Extradural arachnoid cysts are relatively rare. Being detected more often in men, mainly in the III-IV decades of life, they are often combined with kyphoscoliosis, syringomyelia, and spinal dysraphia. Cysts are usually located along the dorsal or dorsolateral wall of the dural sac and in 65% of cases they are found in the middle and lower thoracic spine. In 12% of cases, cysts of the thoracolumbar localization are detected, in 13%-lumbar and lumbosacral, in 7%-sacral. The rarest cervical cysts, occurring with a frequency of no more than 3% [1,2].
Spinal Extradural Arachnoid Cysts (SEACs) are rare expansive masses that account for about 1% of all spinal tumors. They arise from a small defect in the dura mater and cause a herniated arachnoid. The etiology of SEACs remains unclear and they are widely recognized as congenital, however they can also develop secondary to trauma, infection, inflammation, or surgery. SEAC is usually observed in young men in the second decade of life, and the clinical picture depends on the localization of the cyst in the spinal canal. SEAC are usually found in the midthoracic region before the thoracolumbar junction, and only 3% of all SEAC are observed in the cervical spine [9]. Case reports provide materials aimed at expanding medical scientific knowledge, especially in neoplastic diseases. The literature provides extremely scarce data on cases of solitary extradural cystic tumors of the thoracic spine in children [4-14].
In this article, we report on the clinical and radiological features, surgical approach and outcomes, postoperative follow-up, and final neurological outcome of the operation. Presentation of the case in a 3-year-old boy for 3 months, there was a gradual decrease in muscle strength in the legs and the development of lower deep paraparesis and partial dysfunction of the pelvic organs of the central type. There was no history of significant medical or surgical intervention. There was no family history of any genetic disease or malignancy. During neurological examination, he had reduced muscle strength on his legs, no sensory disturbances, no pathological reflexes, deep lower paraparesis. According to the Frankel scale type “C” and according to the McCormick scale-3rd degree.
Figure 1:MRI signs of a cystic mass located extradural extramedullary in the spinal canal on the right at the level
of the bodies of Th6-Th8 vertebrae, compressing the spinal cord. T2-contrast magnetic resonance imaging showing
a well-defined hyperintense mass located extradural, extramedullary in the spinal canal on the right at the level of
the Th6-Th8 vertebral bodies. MRI scans: T1 axial (A), coronal (C), T2 axial (B), coronal (G), sagittal (E), primary scan
topogram (G), contrast sagittal (F), 3D tractographic map (H).
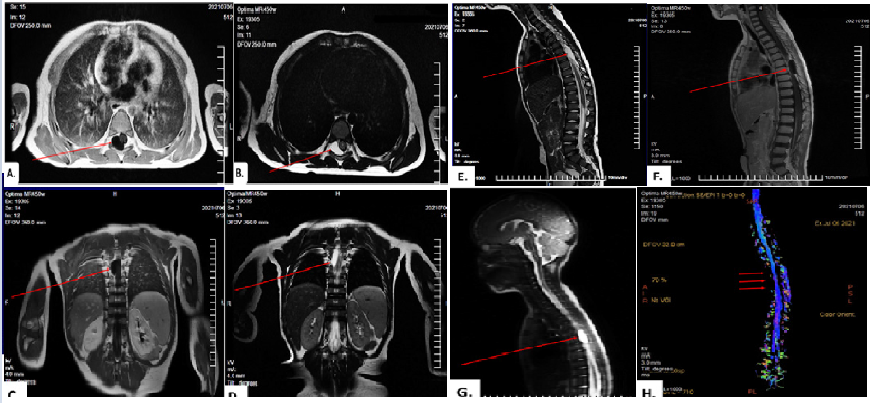
Magnetic resonance imaging (Optima MR450w, General Electric, USA, 1.5 Tesla) showed a well-defined T1-weighted isointense and T2-weighted hyperintense ovoid cystic mass with an enhanced internal solid component, 27cm × 15cm × 8cm, which squeezed the spinal cord from behind at the level of VTh6-8 (Figure 1). An MRtractography (DWI) of the thoracic spinal cord was performed and the following data were determined: pronounced displacement, deformation, and compression of the conductive tracts of the spinal cord to areas of compression of the neoplasm (at the level of VTh6-8). The patient’s vital signs were stable. Body temperature is normal, pulse is regular, 84 beats per minute, blood pressure is 80/50mm of Hg, respiratory rate 22 beats per minute. According to the indications, an operation was scheduled in a planned manner. Surgical treatment was carried out by hemilaminectomy of VTh7 and VTh8 vertebrae at the level of the extradural cyst. Were removed spinal extradural arachnoid cyst totally with a capsule. The patient’s neurological deficit persisted for some time in the postoperative period. According to histological studies, an extradural arachnoid cyst of the spinal cord was confirmed (Figure 2).
Figure 2:MRI gram after surgery. MRI signs of SPE after removal of an extradural extramedullary mass at the level
of the bodies of Th6-Th8 vertebrae (the spinal cyst is not detected, there are no signs of recurrence). MRI scans: T1
axial (A), T1 coronal (B), T1 sagittal (C) and T2 sagittal (D).
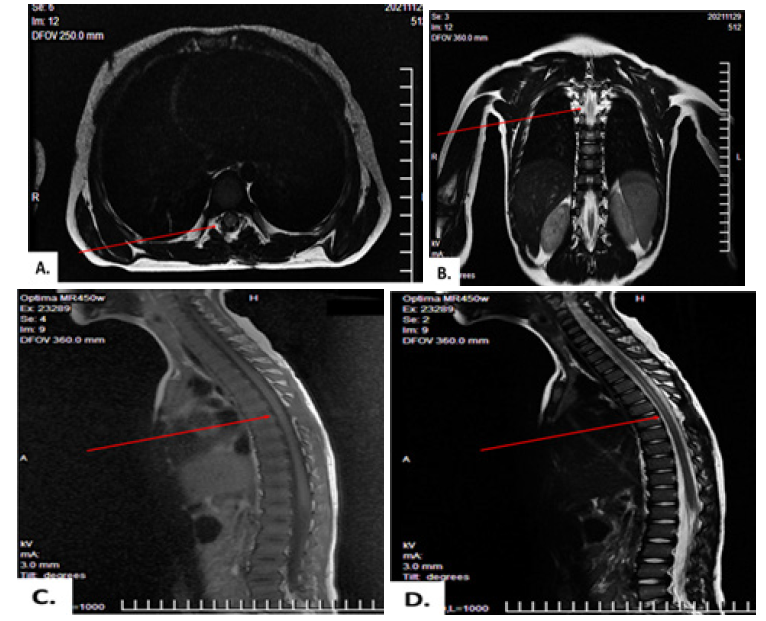
Figure 3:Dynamics of neurological deficits before and after surgery. According to the Mc-Cormick scale (A),
according to the Frankel scale (B).
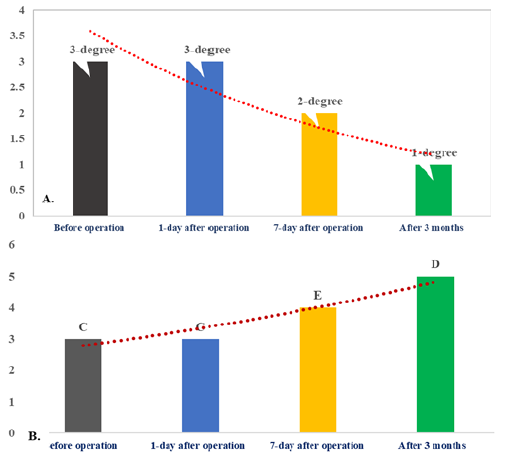
The general condition of the patient in the postoperative period is satisfactory. Breathing is even, respiratory rate 20 beats/ min. Vesicular breathing is heard in the lungs. AD 100/60mm. rt. Art. Pulse 88 beats/min. The abdomen is soft and painless. Urination regular, independent. Consciousness is clear. There are no meningeal symptoms. There are no cerebral symptoms. Pupils D=S, photoreaction saved. The movements in the limbs are not limited. Neurological deficits are eliminated. Functions of the pelvic organs restored. Restoration of neurological deficits according to the Frankel scale from “C” to “E”, according to the McCormick scale from grade 3 to grade 1. Performs stato-coordinator tests without difficulty. Stable in the Romberg position (Figure 3).
The patient was discharged 15 days after the operation in a satisfactory condition, a second consultation was recommended after 2 months. On re-examination, a significant improvement in the patient’s condition and the absence of neurological deficits were determined. At the moment, the patient is developing according to the characteristics of the growth and development of children of his age. Thus, based on this clinical case, the following conclusions can be drawn. In young children, spinal extradural arachnoid cysts of the spinal cord can cause disturbances in sensory and motor functions in the limbs and pelvic organs. In such cases, the use of modern neuroradiological research methods is of great priority, in particular, the use of contrast MRI and MR tractography is appropriate, which is highly informative in choosing an operative approach and predicting the further condition of patients in the preand postoperative period, which can guarantee the effectiveness of the doctor’s treatment tactics. Timely detection of spinal extradural arachnoid cysts and correctly tactful surgical intervention in this pathology provides a complete restoration of vital signs and the ability to work of patients.
References
- Evzikov GY, Kushel YV (2012) Spinal extradural arachnoid cysts. Neurosurgery 2: 8-12.
- Perlmutter OA, Yarikov AV, Smirnov II, Fraerman AP, Simonov AE (2020) Spinal arachnoid cysts (literature review). Povolzhsky Oncological Bulletin 2(42).
- Stupak VV, Shabanov SV, Pendyurin IV, Rabinovich SS (2014) Results of surgical treatment of patients with extramedullary hourglass tumors. Spinal Surgery.
- Bowman JJ, Edwards CC (2020) Extradural arachnoid cyst with bony erosion: A rare case report. J Spin Surg 6(4): 736-742.
- Hulens M, Bruyninckx F, Thal DR, Rasschaert R, Bervoets C, et al. (2022) Large-and small-fiber neuropathy in patients with tarlov cysts. J Pain Res 15: 193-202.
- Medani K, Lawandy S, Schrot R, Binongo JN, Kim KD, et al. (2019) Surgical management of symptomatic tarlov cysts: Cyst fenestration and nerve root imbrication-a single institutional experience. J Spin Surg 5(4): 496-503.
- Murphy KP, Ryan S (2019) Shrinking of a tarlov cyst. BMJ Case Rep 12(3):
- Nabors MW, Pait TG, Byrd EB, Karim NO, Davis DO, et al. (1988) Updated assessment and current classification of spinal meningeal cysts. J Neurosurg 68(3): 366-3
- Özdemir M, Pelin Kavak R, Gülgönül N (2019) Spinal extradural arachnoid cyst in cervicothoracic junction. Spinal Cord Ser Cases 5:
- Sudhakar T, Desir LL, Ellis JA (2021) Tarlov cyst rupture and intradural hemorrhage mimicking intraspinal carcinomatosis. Cureus 13(6):
- Sun JJ, Wang ZY, Teo M, Li ZD, Wu HB, et al. (2013) Comparative outcomes of the two types of sacral extradural spinal meningeal cysts using different operation methods: A prospective clinical study. PLOS One 8(12):
- Wilson PE, Oleszek JL, Clayton GH (2007) Pediatric spinal cord tumors and masses. J Spinal Cord Med 30 Suppl 1(Suppl 1): S15-20.
- Yun ZH, Zhang J, Wu JP, Yu T, Liu QY (2021) Transforaminal endoscopic excision of bi-segmental non-communicating spinal extradural arachnoid cysts: A case report and literature review. World J Clin Cases 9(31): 9598-9606.
- Yoo KH, Kim MC, Ju CI, Kim SW (2020) Extradural spinal arachnoid cyst as a cause of cauda equina syndrome in a child. Korean J Neurotrauma 16(2): 355-359.
© 2022 Aliev MA. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






