- Submissions

Full Text
Techniques in Neurosurgery & Neurology
Characteristics of Pediatric Hospital Fear and Efficiency of New Distraction Technique Holographic Display for Reducing Fear and Pain in Children
Alina Rostsinskaja1, Marianne Saard1,2*, Kirsi Sepp2, Christen Kööp1, and Anneli Kolk1,2
1University of Tartu, Faculty of Medicine, Estonia
2Tartu University Hospital Children’s Clinic, Estonia
*Corresponding author: Marianne Saard, University of Tartu, Faculty of Medicine, Estonia
Submission: April 14, 2022;Published: June 13, 2022

ISSN 2637-7748
Volume5 Issue2
Abstract
Management of pediatric hospital fear and procedural pain is challenging. Distraction techniques are considered as one of the most effective non-pharmacological ways to alleviate children’s pain. The aims of the study were to examine the characteristics of children’s hospital fear and assess the efficiency of holograms in reducing pain during medical procedures. Fifty-one children participated (mean age 8.62 years; SD=4.94). Parents answered the children’s hospital fear questionnaire. Nurses assessed children’s pain with The Face, Legs, Activity, Cry, Consolability (FLACC) Scale during medical procedures before and after initiating holograms. HYPERVSN holographic solution with 31 different 3D animations was applied. Results showed that parents described high hospital fear scores (7-10/maximum 10) in 45.1% of children. Fifty-five percent of parents considered venipuncture as the most frightening procedure. Interestingly, the number of children with high fear scores increased with age (p<0.0001). Also, the results revealed parents’ incapability of dealing with children’s fears. Children’s pain scores during medical procedures were significantly lower after viewing holograms- pain reduction 4.01 points (out of 10). Therefore, the study shows great promise in applying hologram technology as a new effective distraction technique for reducing children’s fear and pain during medical procedures.
Keywords: Hospital fear; Procedural pain; Children; Distraction methods; Holograms
Introduction
Medical fears have been identified as a common subcategory of fear in children [1] and, unlike other types of fear, may increase with age [2]. Fear is an emotion that is thought to arise as an alarm to a dangerous and/or life-threatening situation [3]. Hospital surroundings create fear in children, mostly when associated with invasive and painful medical procedures, which increase their distress in the following hospital visits in the future [4,5]. Management of medical fear and procedural pain is a challenging and complex mission in children. Different hospital procedures are often painful and scary for children in various age-groups. Children’s fears about medical procedures are multifaceted. Research has shown that the most prevalent fears have been associated with needle procedures (injections, blood tests) as these were accompanied by immediate pain [6-9] and can increase pain perception [10]. A study by Salmela [8] revealed that 91% of children expressed at least one fear related to medical procedures, from which 28% of children were afraid of being a patient because it was associated with pain and 29% were frightened by various nursing activities [8]. Fear of needles could continue into adulthood and induce avoidance behaviours [7,8]. Children were also frightened in new and incomprehensible situations when meeting medical staff, who are mostly unfamiliar to them [8,11]. Furthermore, children who had previously been exposed to medical procedures reported even more fears than children who had not been to a hospital [8]. Surgical procedures further increased medical fear and stress in children of all ages [12].
Children’s fear and pain levels have been assessed in various invasive procedures [5,13]. Specifically, during needle procedures in children from their own and their parents’ perspectives. The results showed that the needle‐related fear level was as high as the pain level reported by children themselves [14], however, the parents perceived that the children experienced more fear than pain during needle insertion [15]. Still, further analysis revealed that younger children themselves reported their fear levels to be higher than their pain [14]. Nonpharmacologic techniques in procedural pain and fear relief are generally divided into physical and behavioral techniques. Physical techniques include examples such as massage and counter stimulation; behavioral techniques such as communication before or during the procedure and distraction [16,17]. Efficacy of physical techniques, such as balloon inflation, ball squeezing, and coughing during venipuncture procedures in children aged 7-12 years was confirmed [18]. As an example of behavioral intervention, children participated in a medical playgroup prior to surgical procedures which demonstrated significant reductions in anxiety and self-reported fear level [12]. Moreover, therapeutic play has also had a positive effect on fear and anxiety levels in children with liver transplantation [19], and finger puppet play has been recommended for use by nurses and parents for reducing the fear of surgery in children [20]. One way to alleviate a child’s fear during a medical procedure is distraction and care provided by parents [21]. Parent and nurse directed distraction have shown some benefit [22,23], but may not be as effective when the distractor lacks specific training or is unable to focus on the distraction of the child [24,25].
Furthermore, distraction techniques are considered as one of the most effective non-pharmacological ways to alleviate a child’s pain and distress during a medical procedure [26-28]. In a study by Nasab [29], parents reported that distraction was one of the important environmental factors in reducing their children’s hospital fear. Research conducted in clinic waiting areas has shown that positive distraction leads to a significant increase in calm behaviour in children [30]. The effectiveness of distraction lies in the perception of the painful stimuli, which is hindered by diverting the child’s attention to an attractive element [27,31]. This is based on the Gate Control Theory, stating a link between perception of pain and level of attention devoted to the stimulus affecting the painful experience [32,33]. Thus, using distractions with multiple sense engagement, such as auditory and visual, may catch the child’s attention through more than one sense engaging methods. These include coaching, toys, television, music, storytelling, and technology-based interventions such as tablets, computers, or virtual reality (VR) [25,27,34,35]. The use of a certain method depends on the child’s age, developmental stage, and the type of procedure [36]. For example, VR goggles could not be used in all groups of children, as most of the headset manufacturers’ have set the age limit to 7 years and older. One modern technique in distraction could be using holographic videos or holograms. A holographic display uses a spatial light modulator with an encoded hologram to reconstruct a 3D scene by the interference of light. The holographic display reconstructs the 3D scene in depth and enables accommodation and convergence of the eyes [37]. Holograms are captivating and holographic mobile-based applications have had a significant impact on children’s motivation in the classroom [38]. Altogether, data implies that it is important to develop and establish practical methods to be used in children that would decrease children’s medical fear and pain levels. Therefore, we have developed and first introduced the holographic technique as a new method of distraction in children to help alleviate pain and fear during medical procedures.
Hypotheses and Aims
The following hypothesis were formed: children suffer from significant hospital fears reported by their parents and they are most afraid of needle-related procedures; children’s fear scores (reported by the parents) are associated with their pain scores (reported by the nurses) during the medical procedures; expressing fears in procedures depends on each child’s characteristics, the child’s age, the parent’s fear scores, and the type of procedure; higher parental fear is associated with higher scores of fear in children; children whose parents have not prepared them at home or prior to the procedure express more fear and pain; children’s fear and pain levels are significantly higher before watching holograms compared to the condition after hologram-based distraction (assessed by parents and nurses); holograms can reduce parents’ fear scores during the child’s hospital procedure. Little is known about the content and causes of children’s hospital-related fear estimated by parents, and about the effectiveness of developing new distraction methods. Based on this, we set the following aims: to examine hospital fear and procedural pain levels in children based on the parents’ questionnaires and nurses’ reports; to determine the potential relationship between hospital fear and the child’s age, type of procedures performed, and parents’ own fear levels; to investigate the impact of information given by parents to children before hospital visits to reduce the child’s fear; to investigate the efficiency of the holographic display method, the newest nonpharmacological hospital fear mitigation approach.
Methods
The study was designed to gather information on the structure of hospital fear via questionnaires from parents/guardians of the children and to assess children’s pain scores during hospital procedures. The study was carried out between January 2020 and September 2020 in Tartu University Hospital’s Children’s Clinic, in the Department of General Pediatrics and Neurology. The study was approved by The Research Ethics Committee of the University of Tartu (approval number 302/M-11).
Participants
The study group consisted of 51 randomly selected children (mean age of the children was 8.62 years; SD=4.94). The children were admitted to the hospital for various reasons with 28 different diagnoses, the most common was epilepsy (n=13). The procedures that were recorded in the study were the following: vaccination; other procedures utilizing a needle (venipuncture, inserting a cannula, removing a cannula, etc.); ear, nose, and throat examination; wound care; auscultation and ECG; blood pressure measurement; and others. Children’s pain levels were assessed at the beginning of the procedure before distraction and after the intervention was implemented. The questionnaire for parents/guardians of children was answered by 51 parents, pain scores were assessed by nurses. Parental written informed consent and child’s verbal agreement to participate in the intervention was obtained.
Parents’ Questionnaire
The study utilized a questionnaire created by the authors (considering cultural background) to parents or guardians. The questionnaires were sent out and completed by parents retrospectively after the procedures using Redcap software. The questionnaire sent to the children’s parents/guardians recorded the type of medical procedures that had been performed and whether the procedure was painful or not. The questionnaire also indicated the general characteristics of the children, such as easily excited; worried or mostly brave and cheerful; etc. The parents were asked in detail what procedures created the most fear and pain in their children, how they have prepared their child before hospital visits, and what distraction techniques and devices could reduce medical fear. The questionnaire included a 10-point Likert scale to assess the fear level of the child and the parent. A Likert scale is a type of psychometric response scale in which responders specify their level of agreement to a statement typically in five points: (1) Strongly disagree; (2) Disagree; (3) Neither agree nor disagree; (4) Agree; (5) Strongly agree. As one aim of the study was to evaluate the efficacy of a novel hologram system used in this study, the questionnaire furthermore inquired whether the children had seen the hologram system and how parents and their children reacted to it.
FLACC Pain Scale
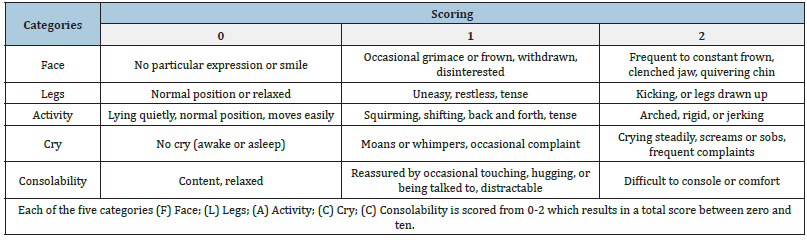
The pain level scores during the procedure and after viewing the hologram were assessed by the nurses performing the procedure. The pain scores were assessed with The Face, Legs, Activity, Cry, Consolability Scale. The FLACC scale assesses the children in the aforementioned five categories and can allocate 0, 1, or 2 points in each category, which are then added to acquire a behavioral score. Each patient must be observed for at least 2-5 minutes (Table 1).
Table 1: Scoring criteria under the five categories of the FLACC Scale.
Hologram System
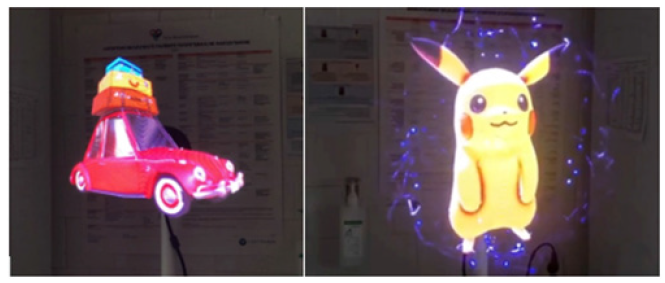
The study concentrated on evaluating the efficacy of the HYPERVSN all-in-one 3D holographic solution in reducing the fear and procedural pain of young patients through distraction. The holographic display is a four-ray rotor that spins fast enough to result in a convincing 3D holographic image. Sound-tuned, hightechnology video projectors produce high-definition 3D visuals with a realistic holographic effect and the management platform allows the creation of various unlimited 3D holograms [39]. The intervention with holograms was standardized. Children were displayed 31 different holographic 3D animations and images in specific order, selected by authors. The animations were also accompanied by sounds and music. Holograms were shown during the procedure/examination. At the time, the children did not receive any other intervention methods. The hologram system was installed in the treatment room of Tartu University Hospital’s Children’s Clinic, in the Department of General Pediatrics and Neurology (Figure 1).
Figure 1:The illustration of 3D holographic images applied in the procedure room.
Data Analysis
The statistical analysis was performed using the statistical package SAS Version 9.4 and program R 4.0.2. The Kolmogorov- Smirnov test was used for the assessment of normality. Statistical comparisons between non-normally distributed continuous variables were performed with Wilcoxon-Mann-Whitey test. To examine the association between variables, the Pearson’s correlation, Spearman correlation, simple linear regression analysis, and Fisher’s Exact Test were used. Paired Sample’s T-Test or Test of Symmetry was conducted to assess whether longitudinal changes in groups were significantly different. The confidence level was set to p<0.05. We controlled the false discovery rate (FDR) to be lower than 5% by using linear step-up procedure for multiple t-tests. Only p-values that are below the adjusted FDR significance threshold are therefore significant.
Results
Characteristics of Children’s Hospital Fear and Pain
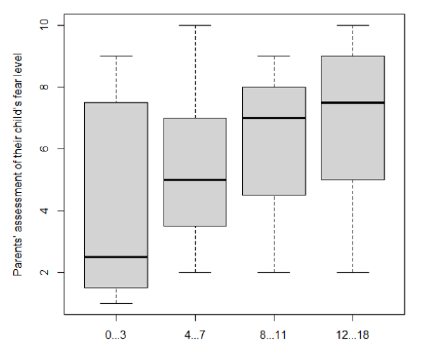
1) The parents assessed the fear scores of their children on a
10-point Likert scale based on the child’s latest hospital procedure.
The results showed that the parents reported the highest possible
fear scores (7-10 points) for 45.1% of the children (n=23, Table
2). The percent of children with higher fear scores significantly
increased with age (Fisher’s Exact Test p<0.0001), which means
that older children were reported to have higher fear scores
compared to younger children (Table 2 & Figure 2). The fear level
7 and above was reported among 58.3% of the children aged 12-18
years compared to 33.3% in children aged 0-3 years (Table 2).
Table 2: The relationship between the level of hospital fear and the age of the child.
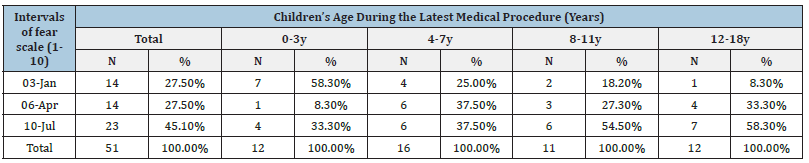
Figure 2:The relationship between the level of hospital fear and the age of the child (simple linear regression model
with 95% confidence limits, p=0.0072, R-Square=0.12).
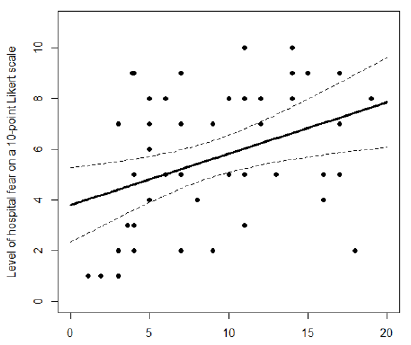
The mean fear level was highest in the oldest children’s group: 6.8 points out of 10 in children aged 12-18 years- and lowest in the youngest children’s group: 4.2 in children aged 0-3 years (Table 3 & Figure 3).
Table 3: Characteristics of the parents’ assessment of their children’s fear levels on a 10-point scale in different agegroups.
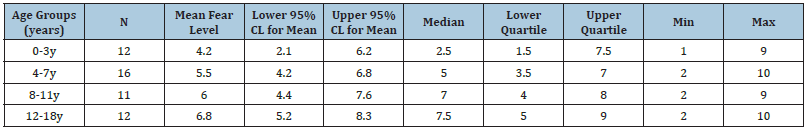
Figure 3:Distribution of the children’s fear levels between different age groups.
Interestingly, there did not exist a significant association between the children’s age and the number of procedures that they had gone through (p=0.97) therefore, the higher fear scores of the older children could not be explained by their higher participation in the procedures during their life. The potential relationship between children’s hospital fear scores and the parents’ fear scores was analyzed. There was not a statistically significant association between the children’s and parents’ fear scores: the Pearson correlation coefficient r=0.1779, p=0.212.
2) The association between children’s fear scores reported
by the parents with children’s pain scores reported by the nurses
was examined. There were no significant differences between
the fear and pain levels in children assessed by the parents and
the nurses before the hologram distraction (Test of Symmetry,
p=0.072). Therefore, the parents assessed their children’s fear
scores to be similar to the nurses’ assessment of pain scores in
the same children. Thus, higher scores of fear are associated with
higher pain perception in children.
3) Additionally, the relationship between different medical
procedures and children’s fear was analyzed. In total, the highest
percent of the parents (55%, n=28) reported that their child
was most afraid of the venipuncture (Table 4). The same vast
venipuncture fear occurred in 61% of children (n=14) in the highest
fear level (scores 7-10 out of 10) group.
Table 4: Painful procedures and the children’s fear levels assessed by parents.
4) Furthermore, the effect of parental preparation of children for a hospital visit was studied. Interestingly, the Wilcoxon-Mann- Whitney test revealed that children whose parents had prepared them at home or prior to the medical procedure in some way did not express significantly less fear compared to the children whose parents had not prepared them for the upcoming procedure [median 5.5 (3.5-8.0) vs 3.0 (2.0-5.0), p=0.15].
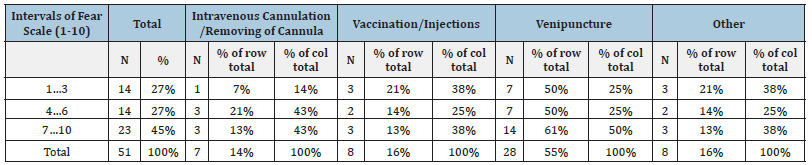
Efficiency of the Novel Hologram Method
In assessing the efficiency of the new hologram technique, we found significant positive changes in children’s reduced pain scores on FLACC scale (p<0.0001) (Table 5). The results showed that the pain scores of most of the children were lower after initiating the hologram distraction during the procedure compared to their initial pain level score before the hologram. Further analysis showed that the hologram distraction eliminated the pain: children’s pain scores were reduced to zero in 57% of the children who presented with pain scores 4-6 on FLACC scale before seeing the hologram during the painful procedure (Table 5).
Table 5: Children’s fear levels on FLACC scale before and after the hologram distraction during procedures.
In a detailed analysis of the children’s pain scores on FLACC before and after initiating the hologram technique, the results showed that the mean reduction of pain level was 4.01 points (95% CI: 3.5-4.6) (Figure 4) therefore, after using the hologram, the children’s pain scores were statistically significantly lower (4 points on average, Paired Samples T-Test, p<0.0001) (Table 4).
Figure 4:Differences in children’s pain levels on FLACC scale before and after initiating the hologram technique.
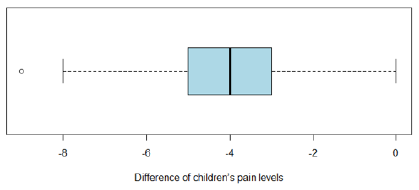
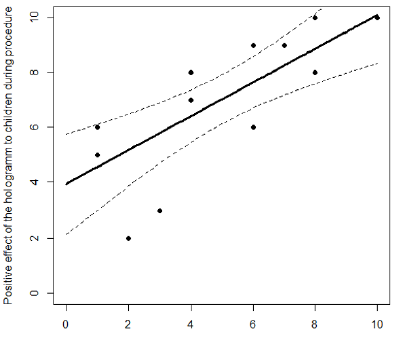
Figure 5:Association of the positive effect of the hologram technique for the children and their parents.
The nurses’ feedback revealed that directing attention to the hologram helped to facilitate the procedure.
According to the parents, hologram technology significantly helped to reduce their child’s fear levels during medical procedures. An additional analysis with the parents’ feedback questionnaire showed that after initiating the hologram, reduction of the children’s fear scores was significantly associated with their parents’ fear reduction – the parents that reported a higher positive effect of the hologram for their child also reported higher calming effect to themselves (Figure 5) (Spearman correlation r=0.80475, p=0.0003).
Discussion
Previously, research has found that management of medical fear and procedural pain in children is a challenging and complex mission. The child’s perception of coping with fear during medical procedures grows with well-being, which is related to positive images, play, humor, natural environment, learning, and receiving presents [8,40]. In the current study, we found that 45.1% of the children in the study group had high scores of medical fear (7-10 points out of ten) reported by their parents. An important result of this study was that the levels of fear in children were related to the age of the child - children’s fear levels increased with age. Remarkably, the mean fear level was highest in the oldest children’s group: 6.8 points out of 10 in children aged 12-18 years- and lowest in the youngest children’s group: 4.2 in children aged 0-3 years. Previously have been found that medical fears induce further avoidance behaviors in patients over time [8], and these children who had previously participated in fearful medical procedures have reported more fears than children who had not been to a hospital [8]. We did not find a significant association between the children’s age and the number of procedures that they had gone through– therefore, the higher fear levels of the older children’s group could not be explained by their higher participation in the procedures during their life. This may be instead related to a lack of preparation for children in the healthcare processes and treatment of fear in the past. Thus, we can confirm that medical fears, unlike other types of fear in children, may increase with age as previously reported by Gullone [2]. Different hospital procedures are often painful and scary for children in various age-groups. Previously, researchers have shown that the most prevalent fears have been associated with needle procedures. In the current study, when considering different types of procedures, in all age groups 55% of the parents reported that their child was most afraid of venipuncture. Like many authors have emphasized, children need an extra level of preparation in the healthcare processes. Their primary need is to know that they are safe and given age-appropriate information to reduce fear and anxiety [41]. Our results showed that children whose parents had prepared them at home or prior to the medical procedure did not express significantly less fear compared to the children whose parents had not prepared them. Our study furthermore confirms the parents’ lack of ability to deal with children’s hospital fears, which could mean that the parents do not have enough knowledge of how to prepare their children. It means that parents need instructions and education in this field and more available information. Developing parental and future medical professionals’ expertise for dealing with hospital fear and pain is an important area. Also, educating children about the upcoming medical procedure by watching an animated video or a cartoon about the procedure is effective in reducing children’s perceived level of fear and pain during an intervention [42].
In the current study, for the first time according to our knowledge, the novel hologram system was utilized and proved to be an effective distraction technique in children for fear and pain reduction during hospital procedures. The holographic technique was effective for children in all age groups, including smaller children aged 10-13 months. In addition, procedures like measuring blood pressure and Botox therapy were also easier to be conducted using the hologram method. It should be added that the parents reported the calming effect of the hologram viewing on themselves. We believe that looking at the holograms with music, the multiple senses are involved and in addition to distraction, may improve children’s emotional state, attention, and perception of control over pain. Compared to cartoons on screens, the holograms could be more attractive to children, because of novelty and spatial characters. Referring to previous studies- the more a child is active and engaged in the activity of distraction methods, the more effective the results might be [43]. In summary, the interest in more interactive and engaging methods of distractions increases [44]. We highly recommend that healthcare providers would use new distraction techniques, like holograms, during children’s hospital procedures. After releasing our preliminary results, five additional departments in our clinics and four other hospitals in the country started using the hologram technique in everyday practice [45-47].
Limitations
We would recommend continuing research and studies in this field with larger sample sizes and various diagnoses and age groups. Furthermore, developing distraction methods that more specifically consider the child’s age and apply multi-sensory techniques to children in older age groups by engaging senses like touch and scent.
Conclusion and Clinical Message
This study shows great promise in using new hologram technology as a distraction method into hospital fear and pain management by significantly reducing children’s fear and pain scores during procedures. Finding new solutions for children’s hospital fear is an important topic as it would make the hospital experience less stressful for children and their parents, also benefiting the work of the medical staff and increasing the quality of medical services. As children’s fears of medical procedures are multifaceted, we recommend creating multimodal approaches to engage children during procedures and even before the hospital visit, e.g., starting from home by using web-based applications. Because knowledge of fear and pain management in parents is still quite inadequate, effective educational efforts in this area would be recommended.
Funding
The study was funded by the Estonian Science Foundation PRG789.
Declaration of Conflicting Interests
The authors have no conflicts of interest to declare. All authors declare no competing interests.
References
- Ollendick TH (1983) Reliability and validity of the revised fear survey schedule for children (FSSC-R). Behav Res Ther 21(6): 685-692.
- Gullone E (2000) The development of normal fear: A century of research. Clin Psychol Rev 20(4): 429-451.
- Albano AM, Causey D, Carter BD (2000) Fear and anxiety in children. In: Walker CE, Roberts MC (eds.), Handbook of Clinical Child Psychology. New York, USA, pp. 291-316.
- Chen E, Zeltzer LK, Craske MG, Katz ER (2000) Children's memories for painful cancer treatment procedures: Implications for distress. Child Dev 71(4): 933-947.
- McMurtry CM, Riddell RP, Taddio A, Racine N, Asmundson GJG, et al. (2015) Far from “just a poke” common painful needle procedures and the development of needle fear. Clinic J Pain 10: 3-11.
- Karlsson K, Rydström I, Enskär K, Englund AC (2014) Nurses' perspectives on supporting children during needle-related medical procedures. Int J Qual Stud Health Well-Being 9(2): 23063.
- Noel M, McMurtry CM, Chambers CT, McGrath PJ (2010) Children’s memory for painful procedures: the relationship of pain intensity, anxiety and adult behaviors to subsequent recall. J Pediatr Psychol 35(6): 626-636.
- Salmela M, Salanterä S, Aronen ET (2009) Child-reported hospital fears in 4 to 6-year-old children. Pediatr Nurs 35(5): 269-276.
- Taddio A, Ipp M, Thivakaran S, Jamal A, Parikh C, et al. (2012) Survey of the prevalence of immunization non-compliance due to needle fears in children and adults. Vaccine 30(32): 4807-4812.
- Rhudy JL, Meagher MW (2003) Negative affect: effects on an evaluative measure of human pain. Pain 104(3): 617-626.
- Monteiro HM, Shetty AP, Bagali PV (2014) Fears of school-age children and parental perceptions of nursing support during hospitalization in a selected pediatric hospital, Mangalore. Muller Journal of Medical Science and Research 5(2): 139-142.
- Jones MT, Kirkendall M, Grissim L, Daniels S, Boles JC (2021) Exploration of the relationship between a group medical play intervention and children's preoperative fear and anxiety. J Pediatr Health Care 35(1): 74-83.
- Castillo BT, Torres JAP, Sánchez LM, Castellanos ME, Fernández LE, et al. (2019) Reducing the pain in invasive procedures during paediatric hospital admissions: Fiction, reality or virtual reality? An Pediatr (Engl Ed) 91(2): 80-87.
- Hedén L, Essen L, Ljungman G (2020) Children's self‐reports of fear and pain levels during needle procedures. Nurs Open 7(1): 376-382.
- Hedén L, Essen L, Ljungman G (2016) The relationship between fear and pain levels during needle procedures in children from the parents' perspective. Eur J Pain 20(2): 223-230.
- Canbulat N, Ayhan F, Inal S (2015) Effectiveness of external cold and vibration for procedural pain relief during peripheral intravenous cannulation in pediatric patients. Pain Manag Nurs 16(1): 33-39.
- Dutt Gupta J, Brown T, Mycama M (2007) Effect of communication on pain during intravenous cannulation: A randomized control trial. Br J Anaesth 99(6): 871-875.
- Girgin BA, Göl I (2020) Reducing pain and fear in children during venipuncture: a randomized controlled study. Pain Manag Nurs 21(3): 276-282.
- Zengin M, Yayan EH, Düken ME (2020) The effects of a therapeutic play/play therapy program on the fear and anxiety levels of hospitalized children after liver transplantation. Journal of Peri Anesthesia Nursing 36(1): 81-85.
- Kostak MA, Kutman G, Semerci R (2021) The effectiveness of finger puppet play in reducing fear of surgery in children undergoing elective surgery: A randomised controlled trial. Collegian 28(4): 415-42
- Power N, Liossi C, Franck L (2007) Helping parents to help their child with procedural and everyday pain: Practical, evidence-based advice. J Spec Pediatr Nurs 12(3): 203-209.
- Cavender K, Goff MD, Hollon EC, Guzzetta CE (2004) Parents’ positioning and distracting children during venipuncture: Effects on children’s pain, fear and distress. J Holist Nurs 22(1): 32-56.
- McCarthy AM, Kleiber C, Hanrahan K, Zimmerman MB, Westhus N et al. (2010) Impact of parent-provided distraction on child responses to an IV Child Health Care 39(2): 125-141.
- Fernández-Castro M, Martín-Gil B, López M, Jiménez JM, Liébana-Presa C, et al. (2021) Factors relating to nurses’ knowledge and attitudes regarding pain management in inpatients. Pain Manag Nurs 58: 54-62.
- Williams A, Ishimine P (2016) Non-pharmacologic management of pain and anxiety in the paediatric patient. Current Emergency and Hospital Medicine Reports 4(1): 26-31.
- Birnie KA, Noel M, Chambers CT, Uman LS, Parker JA (2018) Psychological interventions for needle‐related procedural pain and distress in children and adolescents. Cochrane Database Syst Rev 10(10): 5179.
- Koller D, Goldman RD (2012) Distraction techniques for children undergoing procedures: a critical review of pediatric research. J Pediatr Nurs 27(6): 652-681.
- Stinson J, Yamada J, Dickson A, Lamba J, Stevens B (2008) Review of systematic reviews on acute procedural pain in children in the hospital setting. Pain Res Manag 13(1): 51-57.
- Nasab SN, Azeri ARK, Mirbazel S (2020) Effective environmental factors for reducing children's fear in children's hospital: Using parent's attitudes. International Journal of Architecture and Planning 8(1): 1-19.
- Pati D, Nanda U (2011) Influence of positive distractions on children in two clinic waiting areas. HERD 4(3): 124-140.
- Kleiber C, McCarthy AM (2006) Evaluating instruments for a study on children's responses to a painful procedure when parents are distraction coaches. J Pediatr Nurs 21(2): 99-107.
- McCaul KD, Malott JM (1984) Distraction and coping with pain. Psychol Bull 95(3): 516-533.
- Melzack R, Wall PD (1965) Pain mechanisms: a new theory. Science 150(3699): 971-979.
- Hanrahan K, Kleiber C, Miller BJ, Davis H, McCarthy AM (2018) The distraction in action tool©: feasibility and usability in clinical settings. J Pediatr Nurs 41: 16-21.
- Erdogan B, Ozdemir AA (2021) The effect of three different methods on venipuncture pain and anxiety in children: distraction cards, virtual reality, and Buzzy®(randomized controlled trial). J Pediatr Nur 58: 54-62.
- Olsen K, Weinberg E (2017) Pain-less practice: techniques to reduce procedural pain and anxiety in pediatric acute care. Clinical Pediatric Emergency Medicine 18(1): 32-41.
- Haeussler R, Gritsai Y, Zschau E, Missbach R, Sahm H, et al. (2017) Large real-time holographic 3D displays: enabling components and results. Appl Opt 56(13): F45-F52.
- Cerezo R, Calderón V, Romero C (2019) A holographic mobile-based application for practicing pronunciation of basic English vocabulary for Spanish speaking children. International Journal of Human-Computer Studies 124: 13-25.
- KNM EESTI (2021) KNM Eesti Hyper VSN.
- Salmela M, Salanterä S, Aronen ET (2010) Coping with hospital-related fears: experiences of pre-school-aged children. J Adv Nurs 66(6): 1222-1231.
- Lerwick JL (2016) Minimizing pediatric healthcare-induced anxiety and trauma. World J Clinic Pediatr 5(2): 143-150.
- Düzkaya DS, Bozkurt G, Ulupınar S, Uysal G, Uçar S et al. (2021) The effect of a cartoon and an information video about intravenous insertion on pain and fear in children aged 6 to 12 years in the pediatric emergency unit: a randomized controlled trial. J Emerg Nurs 47(1): 76-87.
- Dahlquist LM, McKenna KD, Jones KK, Dillinger L, Weiss KE et al. (2007) Active and passive distraction using a head-mounted display helmet: Effects on cold pressor pain in children. Health Psychol 26(6): 794-801.
- Khadra C, Ballard A, Déry J, Paquin D, Fortin JS, et al. (2018) Projector-based virtual reality dome environment for procedural pain and anxiety in young children with burn injuries: a pilot study. J Pain Res 11: 343-353.
- Benjamini Y, Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Statistic Soc: B 57(1): 289-300.
- Plaisance L, Logan C (2006) Nursing students’ knowledge and attitudes regarding pain. Pain Manag Nurs 7(4): 167-175.
- Voepel LT, Shayevitz JR, Malviya S (1997) The FLACC: a behavioral scale for scoring postoperative pain in young children. Pediatr Nurs 23(3): 293-297.
© 2022 Marianne Saard. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






