- Submissions

Full Text
Techniques in Neurosurgery & Neurology
The Result of Surgical Treatment of Secondary Stenosis of the Cervical Spinal Canal Due to Instability after Vertebra-Spinal Trauma (Clinical Case)
Aliev MA1*, Mamadaliev AM1, Saidov SS2 and Abdulkhakimov PV1
1Neurosurgery Department of the Samarkand State Medical University, Uzbekistan
2Republican National Center for Rehabilitation and Prosthetics of the Disabled, Uzbekistan
*Corresponding author:Dounia Hmimidi, Academic Teaching Hospital Bayreuth, Germany
Submission: May 10, 2022;Published: May 26 2022

ISSN 2637-7748
Volume5 Issue1
Abstract
In this article we analyzed a clinical case, 38-year-old patient D., with diagnose Outcome of spinal injury. Compression fracture of the VC4 body, displacement of the posterior longitudinal ligament in this area, compression of the spinal cord and dural sac, instability of the VC4-5 segments, post-traumatic cicatriclecystic- atrophic-degenerative process spinal cord in the VC4-5 region and compression myelopathy (posthematomyely state), the postoperative outcome was also assessed due to rupture, compression and thinning of the spine tracts in the VC4-5 region”. The patient showed positive changes in the dynamics of clinical and neurological symptoms, an increase in the range of motion in the upper and lower limbs after 3-month post operation- “Corporectomy of the VC4 body and decompression of the spine, stabilization with the MESH-system and a Plate-system”.
Keywords:Instability; Tracts; Decompression; Stabilization; MESH-system
Introduction
Traumas of the spinal column and spinal cord are one of the actual problems in neurosurgery, traumatology and neurorehabilitation. It explains by many complications associated with the inability of patients with spinal cord injury to self-care, gross functional disorders associated with the control of the pelvic organs, high disability rates and the complexity of the social and mental adaptation of patients. Traumatic Spinal Cord Injury (TSCI) is a devastating condition which occurs with an annual incidence of 12,1-57,8 cases per million [1]. TSCI is associated with permanent disability and decreased life expectancy [2]. TSCI is one of the most devastating types of injury, and it results in varying degrees of paralysis, sensory loss, and bladder/bowel dysfunction. The effects of TSCI are not limited to an individual’s health; it also creates an enormous financial burden for families and society at large [3]. Between 250,000 and 500,000 people sustain a SCI each year worldwide [4]. In the United States 12,000 people experience a SCI each year [5]. Injuries can result from trauma, viruses or tumors, in addition to the more common motor vehicle accidents, falls, firearms, and sport injuries [6]. In large industrial cities of Russia (St. Petersburg, Nizhny Novgorod, Irkutsk), the incidence of spinal cord injuries is 0,58-0,6 cases per 10,000 populations [7,8], in Kazakhstan-1,3 cases [9] and in Ukraine-4,4 cases [10].
Aim of the Study
To analyze the results of postoperative treatment of an obsolete comminuted compression fracture and displacement of the VC4 body and instability of the VC4-5 segment due to spinal trauma using a clinical case as an example.
Materials and Methods of Study
In the Neurosurgery Department of the 1st Clinic of the Samarkand State Medical University was analyzed the results before and after treatment of the clinical neurological, neuroradiological (spondylography, multispiral computed tomography, magnetic resonance tomography, magnetic-resonance tractograpy), neurophysiological (electroneuromyography) examinations of 38 years old patient D. who underwent surgical treatment with a diagnosis of Outcome of the spinal injury. Compression fracture of the VC4 body, displacement of the posterior longitudinal ligament in this area, compression of the spinal cord and dural sac, instability of the VC4-5 segments, post-traumatic cicatricle-cystic-atrophic-degenerative process spinal cord in the VC4-5 region and compression myelopathy (posthaematomyelia state), the postoperative outcome was also assessed due to rupture, compression and thinning of the spine tracts in the VC4-5 region. Tetrasyndrome, dysfunction of the pelvic organs with central disorder.
Results of the Study and their Discussion
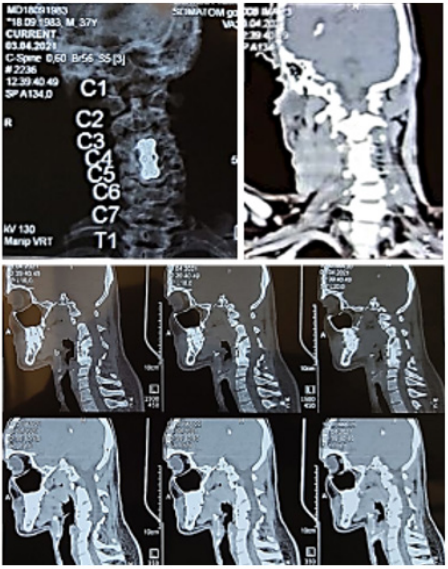
Figure 1: Patient D., 21.07.2019. Computed
tomography reveals a comminuted compression
fracture and displacement of the fourth cervical
spine (VC4) and acute compression of the spinal
cord, instability of the intervertebral segment of
the fourth and fifth cervical vertebrae (VC4-5) as a
result of a spinal trauma.

The patient came to the Neurosurgery Department of the 1st Clinic of SamMU with the complaints of lack of active movements in the upper and lower limbs, urinary incontinence, shortness of breath, abdominal discomfort and general malaise, inability to walk and sit. When studying a case report, the patient states that he considers himself ill since July 21, 2019, and his illness relates to the fact that he injured due to twisting of the neck when diving with his head into the canal. At that period the patient’s arms and legs suddenly lost mobility, and the patient was taken to the Samarkand branch of the Republican Scientific Center for Emergency Medicine, hospitalized in the Neurosurgery Department, and on July 23, 2019, the operation “Ventral elimination of VC4 spondylolisthesis” was performed (Figure 1). After trauma, he had been hospitalized for 50 days using a ventilator through a tracheostomy, and then breathing resumed. For a long time, bedsores were observed in the area of the buttocks, after care and treatment, the bedsores healed, the purulent discharge stopped. Body temperature returned to normal. However, there were no positive changes in the patient. The patient came to the Neurosurgery Department of 1st Clinic of SamMU due to an increase in the number of complaints and was admitted to the Neurosurgical Department for examination and surgical treatment based on the results and complaints of additional examinations (MRI, MR-tractography, ENMG).
Upon admission to the clinic, an objective examination revealed the relative severity of the patient’s general condition, paleness of the skin, slow development of subcutaneous fat, spontaneous respiration, decreased involvement of intercostal muscles during lung excursions, and decreased vesicular respiration in the lungs. On local examination, there is a skin scar on the neck after tracheostomy. Heart sounds are clear. Pulse-80 at 1 minute. Arterial Blood Pressure - 110/70mm Hg. coll. Bloating in the abdomen, constipation, defecation is carried out with a cleansing enema. Low appetite, the urine is passed through a catheter. There are cicatricial changes in the buttocks after a bedsore.
Clinical and Neurological Examination
Clear consciousness, answers questions, general cerebral symptoms were determined. Orientation in time and place is not disturbed. The mood is changeable, depressed. Cerebral nerve activity: in the first pair of nerves - the perception of smell is not disturbed; in pair II - visual acuity and field of vision are the same in both eyes; in pairs III, IV and VI - the movement of the eyeball is unlimited, the strabismus is not observed, the pupils are D=S, the photoreaction is saved; in pair V - the exit sites of the trigeminal nerve are painless, the chewing muscles are developed symmetrically; in VII pair the face is symmetrical; in pair VIII - hearing impairment is not observed; in pairs IX, X - the soft palate is symmetrical, the uvula is located in the center; in pair XI - lifting the shoulders without restrictions, turning the head in both directions is the same, unlimited; in pair XII - the tongue is in the middle line. Skin perception is impaired in the form of conductive hypesthesia, starting from the C4 nerve segments. Spastic tetrasyndrome is determined (lower paraplegia in the legs, deep upper paraparesis in the arms). Sometimes he gathers his legs at the expense of spinal automatism and tries to lift both shoulders (proximal muscle movement relatively preserved). Signs of hypertrophy are found in the muscles of the arms and legs. Ligament reflexes on both sides are enhanced (hyperreflexia), muscle hypertension is determined. The activity of the pelvic organs in the central type is disrupted in the form of seizures, erection and ejaculatory activity are lost.
Results of Additional Examinations
Magnetic-resonance tomography of the cervical spine (Figure 2) shows obsolete comminuted-compression fracture and displacement of the VC4 body, displacement of the posterior longitudinal ligament in this area, compression of the spinal cord and dural sac, cicatricial-cystic-atrophic-degenerative process of the spinal cord in the VC4-5 area, signs of compression fracture (compression is not completely eliminated even in the postoperative period) (Figure 3).
Figure 2: Patient D., June 12, 2020. Magnetic-resonance tomography (A. sagittal scan, T2; B. sagittal scan,
T1; S. axial scan, T2; D. coronary scan, T2) reveals an obsolete comminuted compression fracture of the fourth
cervical spine (VC4) and compression of the spinal cord as a result of vertebrospinal trauma, instability of the
intervertebral segment of the fourth and fifth cervical vertebrae (VC4-5).
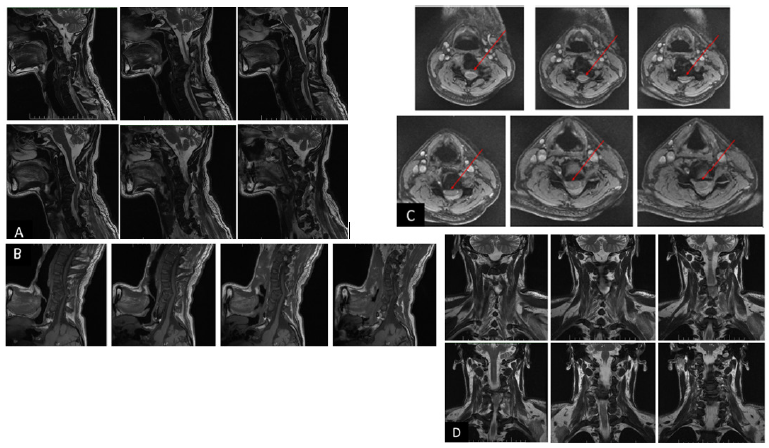
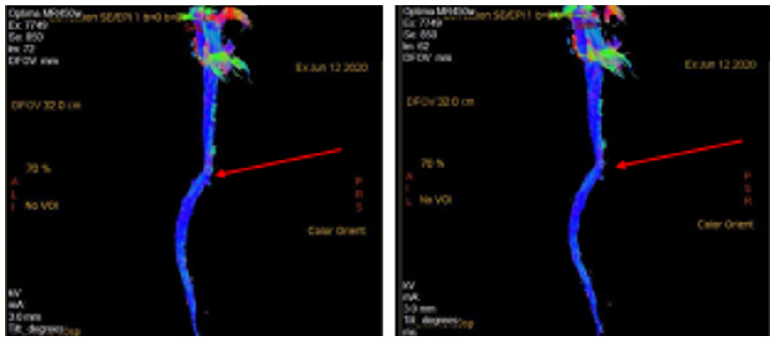
Figure 3: Patient D., June 12, 2020. Magnetic-resonance tractography (Fig. 3) ( in 3D tractographic map) shows
signs of rupture, displacement, deformation and thinning of the vertebral passages in the VC4-5 area.
ENT Conclusion
Pathological signs were not found; Therapist’s conclusion: Signs of pathology of somatic organs were not revealed; The anesthesiologist’s conclusion: there are no indications for anesthesia; Conclusion of the ECG: complete blockade of the right leg of a bundle of His, metabolic changes in the anterior wall of the left ventricle of the heart characterized by signs of hypoxia are determined; Chest X-ray and MSCT examination: no signs of pathology. On electroneuromyography in the projection of the middle cervical segments, impulse blockade was recorded.
Laboratory analyzes
General blood test: Hemoglobin-110,0g/l, leukocytes 5,6; ESR- 38mm/h; erythrocytes-4,0; lymphocytes-29%, monocytes-2%. Blood clotting time according to Sukharev: started-2 minutes 25 seconds, ended -4 minutes 20 seconds. General urine analysis: volume 100,0ml; color - straw yellow; clarity - cloudy; relative density -1015; proteins-no; epithelium -; leukocytes - 4-3-5; erythrocytes - no; from salts - oxalates are found; bacteria -; mucus is found in large numbers. Biochemical analysis of blood: Bilirubin -10,9; AST -0,26; ALT -0,52; creatinine -73,2; urea-5,8; the amount of sugar in the blood is 5,81mmol/l. Indicators of the blood coagulation system: Venous blood coagulation time (according to Fonio): started - 3:09; finished - 4:13; prothrombin time -16 seconds; prothrombin index -100%; INR-1,00. Blood group and Rh factor: B (III), Rh-(negative). Blood test for Hbs Ag and HCV Ag (IFA): negative. Wasserman reaction: RW - negative. The condition of the patient was clinically discussed, and surgical treatment was recommended.
Treatment
The patient was prepared in the clinic and on June 16, 2020, underwent the operation “Corporectomy of the obsolete compression- comminuted fracture and displacement of VC4 body for the ventral approach, decompression of the spine in this area and the “MESH-system” and stabilization with the Platesystem” (Operation No. 136). On the anterior surface of the neck of a patient who undergoing general endotracheal anesthesia, the skin and subcutaneous soft tissues along the medial edge of the muscle of the left third of m. sternocleidomastoids were cut in a length of 4,5cm. Muscular fascia in the same area, m. platysma was cut. A group of deep muscles of the neck separated by a blunt way. Tissues were dissected in the posterior and paravertebral area, and the ventral surface of the VC3-4-5 vertebral bodies was skeletonized. In this area, secondary deformation of the VC4 body, compression-comminuted fracture and a deep wedge-shaped penetration into the spinal canal is detected. After determination with С-arm, Caspar retractor screws were placed on VC3 and VC5 bodies and vertebrotraction was performed. Initially, discectomy of osteophytes in the area between VC4-5, secondary degenerative changed fibrous ring and pulpous nucleus (disc) were performed. After it, in the VC4 body, which was compression-committed and fractured and a deep wedge-shaped penetration into the spinal cord, was performed corporectomy using special instruments systematically (Kerrison roungers). During corporectomy, it was found that the posterior part of the vertebral body had been removed, pressing on the spinal cord in this area, causing scarring of the posterior longitudinal cortex. The scarring process was carefully separated and decompression of the spinal cord and roots in this area was performed. The anterior surface of the VC3 and VC5 bodies was fitted with a titanium plate “Plate-sytem”, fixed with four screws (Figures 4-7), and the cervical part of the spine stabilized with the anterior and middle support columns.
Figure 4: An implant that stabilizes the body of the spine -MESH system.

Figure 5: The fusion of the MESH-system was controlled with the help of C-arm performed during the operation.
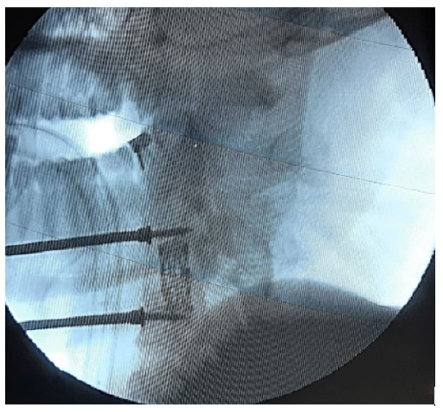
Figure 6: Plate-system-an implant that pre-fixes the spinal bodies.

Figure 7:Stabilization of the spine, decompression of the spinal canal, fixation of the MESH and Plate-system
were confirmed with the help of C-arm, performed during the operation.
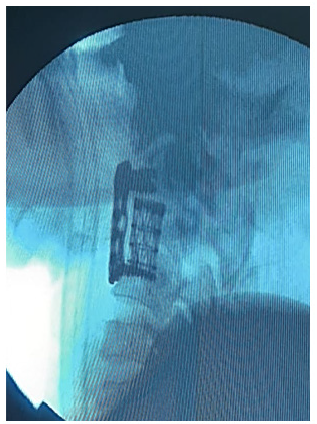
Figure 8: Patient D. April 3, 2021. Multispiral computed tomography of the cervical spine is shown stabilization of
instability in the cervical region of the spine, complete decompression of the spinal canal, satisfactory installation
of the MESH-system and Plate-system 8 months after surgery.
Objective status at the time of discharge
The general condition is moderately severe. Breathing is free. Hemodynamic parameters are stable. The pulse is 78 per minute. ABP is equal to 120/80. The activity of the internal organs is moderate. Appetite improved. Urine is separated through a catheter.
Neurological condition at the time of discharge
The movements in the hands were relatively active, the sensitivity in the legs improved. The mood has improved. Surgical trauma has healed primarily. The stitches have been removed. The patient was discharged home in satisfactory condition. On clinical-neurological re-examination of the patient in catamnesis, skin sensory hypoaesthesia improved, spasticity decreased, tetrasyndrome - lower paraplegia of the legs to deep paraparesis (he raises, collects, extends the leg); it is determined that the deep upper paraparesis in the hands has been restored to the superficial paraparesis. Sometimes spinal automatism did not observe. The lifting activity of both shoulders was not disturbed, pulmonary excursion was restored, trophism of the muscles of the arms and legs was improved. There was a decrease in hyperreflexia in the pelvic reflexes, reduction of muscle hypertension. Hyperreflexia in the tendon reflexes reduced and muscle hypertension decreased. The activity of the pelvic organs is impaired in the form of seizures of the central type, the bladder and rectum feel full, erection and ejaculatory activity is restored, the patient can hold his neck, sit independently.
Results of additional examinations
Multispiral computed tomography of the cervical spine and spondylography (Figure 8) indicated that the implants installed, and the stability of the spine were satisfactory, the secondary stenosis of the spinal canal was completely eliminated, and the spinal cord was noted to be decompressed. Electroneuromyography confirmed a relative decrease in the blockade in the neck area, activation of pulse conduction.
Conclusion
The analysis of the clinical case can lead to the following
conclusions:
In addition to clinical and neurological examinations for traumas
of the spinal column and cervical part spinal cord, it is advisable
to define existing organic changes in the bones and spinal cord based on the data of magnetic resonance tomography, multi-spiral
computed tomography, spondylography. With the help of magnetic
resonance tractography, which is a modern additional MRT
program, it is possible objectively to assess the organic state of the
spinal tracts.
a) This, in turn, plays an important role in choosing the right
type and size of surgery for this type of patient.
b) Reconstructive operations, including decompression,
stabilization and fixation, can cause to a positive regression
of the patient’s clinical and neurological activity, even in the
intermediate and late stages of spinal column and cervical part of
spinal cord trauma if partial spinal tracts are preserved.
References
- Vanden BME, Castellote JM, Fernandez IM, Cuesta JP (2010) Incidence of spinal cord injury worldwide: a systematic review. Neuroepidemiology 34(3): 184-192.
- Hartkopp A, Bronnum HH, Seidenschnur AM, Biering SF (1997) Survival and cause of death after traumatic spinal cord injury. A long-term epidemiological survey from Denmark. Spinal Cord 35(2): 76-85.
- Pickelsimer E, Shiroma EJ, Wilson DA (2010) Statewide investigation of medically attended adverse health conditions of persons with spinal cord injury. J Spinal Cord Med 33(3): 221-231.
- WHO (2013) Spinal cord injury fact sheet, p. 384.
- NSCIS (2013) Spinal cord injury facts and figures at a glance. J Spinal Cord Med 36(1): 1-2.
- Devivo MJ (2012) Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord 50(5): 365-372.
- Kondakov EN, Simonova IA, Polyakov IV (2002) Epidemiology of traumas of the spine and spinal cord in St Petersburg. Zh Vopr Neirokhir Im N N Burdenko 2: 50-52.
- Kuznetsova EY, Garkusha LG, Sidorova GV (2009) Clinical and epidemiological characteristics of disabled people with complicated spinal cord injury as the basis of the basic rehabilitation program. These Report All-Russian Scientific-practical conf VIII Polenov Readings, pp. 96-97.
- Akshulakov SK, Kerimbaev TT (2002) Epidemiology of trauma of spine and spinal cord. Materials of the III Congress of Russian Neurosurgeons, p. 182.
- Shpachenko NN, Klimovitsky VG, Stegniy SA (2007) Features of medical care and prognosis of outcomes in spinal cord injury at the pre-hospital stage. Scientific materials. Conf. dedicated to the 40th anniversary of the Department of Spine Pathology "Spine Surgery - Full Spectrum". pp. 336-339.
© 2022 Aliev MA. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






