- Submissions

Full Text
Techniques in Neurosurgery & Neurology
Remote Site Intracerebral Bleed Following a Neurosurgical Procedure at another Site-A Case Report
Amit Kumar Ghosh1*, Sutirtha Hazra2 and Balasubramonium C3
1Senior Consultant Neurosurgeon, India
2Associate Consultant Neurosurgeon, India
3Senior registrar Neurosurgery, India
*Corresponding author:Amit Kumar Ghosh, Senior Consultant Neurosurgeon,India
Submission: March 07, 2022;Published: April 28, 2022

ISSN 2637-7748
Volume5 Issue1
Abstract
Keywords:Remote site intracranial hemorrhage; Post operative intracranial hemorrhage; Cerebellar hemorrhage; Post operative hemorrhage
Introduction
Remote site bleed is defined as intracranial haemorrhage at a site away from the operated site. Intracranial haemorrhage occurring at “remote site” from the site of surgery is a rare neurosurgical complication and can create significant morbidity and mortality. The location of remote site bleed can be epidural, subdural, or intracerebral [1,2] and can be supratentorial or infratentorial following a supratentorial or infratentorial surgery.
Case
A 67-year-old male, known hypertensive, non-diabetic presented with severe headache and vomiting and right sided weakness, without any history of trauma. He was drowsy and aphasic. GCS was E2M5V2. He was hemodynamically stable and having normal respiratory parameters. Pupils were reacting in both sides. He underwent a CT scan of brain and that showed a left sided acute subdural hematoma with midline shift. His DSA of cerebral vessels was normal and coagulation parameters were also normal. He was not on any antiplatelets or any anti-coagulants. He underwent left sided craniotomy and evacuation of subdural hematoma. He was extubated after surgery and was in a same clinical status as before. His blood pressure was controlled all through with Labetalol infusion. After 12 hours of surgery, his GCS deteriorated (E1V1M2) and his respiration became irregular. Pupils were still reacting and other brain stem reflexes were present Urgent CT scan was done and it showed large cerebellar hemorrhage with hydrocephalus. Prognosis had been explained to family members and urgent EVD (External Ventricular Drainage) was done. Posterior fossae decompression and evacuation of hematoma was suggested but refused by relatives. Elective ventilation was continued. His condition did not improve, rather further deteriorated. Pupil became fixed and dilated with absence of other brain stem reflexes and finally he died. CT brain was repeated, and it showed multiple scattered intracerebral haemorrhage with brain stem infarct with EVD in situ. Literature was reviewed and, in this case, probable cause was CSF release as the other factors were all satisfactory (Figures 1-3).
Figure 1:Showing left sided acute fronto-temporoparietal
subdural hematoma with mass effect.
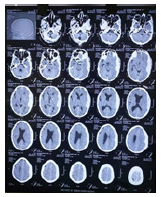
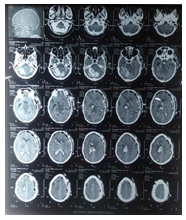
Figure 2:Showing cerebellar hemorrhage with
hydrocephalus with left sided craniotomy for SDH.

Figure 3:Showing the multiple scattered intracerebral
haemorrhage with brain stem infarct after EVD.
Discussion
Medline and Pubmed search were done for remote site intracranial bleed following cranial neurosurgery using key words like postoperative hematoma, remote site hemorrhage. The search found 83 such reports. Postoperative surgical site hematomas can be a life-threatening complication in neurosurgery and are commonly due to inadequate intraoperative hemostasis [3]. Compared to them intracerebral haemorrhage occurring “remote” from the site of craniotomy is a rare neurosurgical complication and can lead to significant morbidity and mortality [4,5]. Different mechanisms have been proposed to explain such a rare occurrence The only common implicating factor among the 83 patients reviewed was sudden decompression in case of Chronically Elevated Intracranial Pressure (ICP). The other possible factors for postoperative remote site bleed are coagulation disorders and hypertension. However, only one patient in our series had hypertension. Transient hypertensive peaks during the recovery from anesthesia have in the past been considered as an important risk factor. More recently, this theory has been partly refuted as only some patients had documented high (200mmHg) blood pressure levels in the perioperative period [6]. Some authors consider that aggressive intraoperative volume loss and CSF removal together or acute obstruction of the venous outflow, can cause brain shift that contributes to intracerebral hemorrhage [7-9]. It is also hypothesized that the tissue thromboplastin released from the injured brain tissue in severe Traumatic Brain Injury (TBI) leads to a local consumptive coagulopathy [10]. The same can happen due to extensive blood loss during surgery and transfusion reactions. The loss of substantial CSF volume during surgery appears to play a central role in the pathophysiological development of remote site hematoma. Suction of the CSF may cause intracranial hypotension. Further reduction of intracranial pressure leads to an increased transluminal venous pressure with subsequent rupture of veins [11,12]. Substantial loss of CSF leads to sagging of the cerebellum away from the tentorium and thus stretching of the cerebellar veins with an increase in the transmural pressure [13] or it may be due to jugular vein compression by the transverse process of atlas in extended neck position [14]. Cerebellar “sag” as a result of CSF hypovolemia, causing transient occlusion of superior bridging veins within the posterior fossa and consequent hemorrhagic venous infarction, has also been proposed to be the most likely pathophysiological cause of remote cerebellar hematoma [15]. Pin site Extradural Hematoma (EDH) is an also a known etiology for remote site bleed [16]. One retrospective study on cerebellar hemorrhages after supratentorial surgery had reported these to be a postoperative event rather than an intraoperative one [17,18].
We strongly advocate screening of all major neurosurgical cases for coagulation, bleeding diathesis and hypertension. While positioning undue neck compression should be avoided to prevent intracranial venous hypertension. Mayfield or three pin fixation needs to be carefully done to prevent breach of inner cortex of skull. During surgery, whenever possible, sudden decompression of brain should be avoided. Cases where massive blood loss is expected, use of preoperative embolization, intraprocedural use of cell saver and even staging of the procedure is warranted to prevent consumptive coagulopathy. In case of sudden rise of ICP or brain becoming tense during surgery in an otherwise relaxed brain, an immediate postoperative CT scan is warranted to rule out remote site bleed. We routinely perform CT scan of our post-operative patients after 4 hours of cranial surgery and after 12 hours. Clinicians need to keep a high index of suspicion to diagnose this fatal complication at an early stage. In a patient with delayed reversal and deteriorating Glasgow Comma Scale (GCS) after surgery, CT is performed at the earliest to rule out this cause. Wide fluctuations in the blood pressure in the operative and postoperative periods should be avoided. In patients with remote site bleed, workup of complete coagulation profile before surgical intervention is highly warranted, Decision to evacuate remote site hematoma should be tailored based on clinical, radiological, and coagulation profile [18]. In patients with deranged coagulation profile, appropriate corrections should be done before any surgical intervention. External ventricular drain or twist drill may be the options in patients who are likely to deteriorate due to abnormal coagulation profile [18]. Though we found 83 reported cases, but it seems unreported and unpublished incidence of such complications are not very uncommon. So, neurosurgeons have to be very careful about this complication and take adequate preoperative and post-operative precautions as mentioned to prevent these catastrophic complications.
References
- Koizumi H, Fukamachi A, Nukui H (1987) Postoperative subdural fluid collections in neurosurgery. Surg Neurol 27(2):147-153.
- Kodama Y, Emoto K, Onda J, Yukawa O (1990) A case of epidural hematoma occurring on the opposite site of craniotomy after clipping surgery performed on internal carotid giant aneurysm. No Shinkei Geka 18(6): 567-570.
- Nagano N, Tabata H, Hashimoto K (1991) Anticoagulant-related intracerebral hemorrhage in patients with prosthetic heart valves-report of two cases. Neurol Med Chir (Tokyo) 31(11): 743-745.
- Fukamachi A, Koizumi H, Nukui H (1985) Postoperative intracerebral hemorrhages: a survey of computed tomographic findings after 1074 intracranial operations. Surg Neurol 23(6): 575-580.
- Kalfas IH, Little JR (1988) Postoperative hemorrhage: a survey of 4992 intracranial procedures. Neurosurgery 23(3): 343-347.
- Marquardt G, Setzer M, Schick U, Seifert V (2002) Cerebellar hemorrhage after supratentorial craniotomy. Surg Neurol 57(4): 241-251.
- Fukamachi A, Koizumi H, Nukui H (1985) Postoperative intracerebral hemorrhages: A survey of computed tomographic findings after 1074 intracranial operations. Surg Neurol 23(6): 575-580.
- Papanastassiou V, Kerr R, Adams C (1996) Contralateral cerebellar hemorrhagic infarction after pterional craniotomy: report of five cases and review of the literature. Neurosurgery 39(4): 41-51.
- Rapana A, Lamaida E, Pizza V (1998) Multiple postoperative intracerebral haematomas remote from the site of craniotomy. Br J Neurosurg 12(4): 364-368.
- Palmer JD, Sparrow OC, Iannotti F (1994) Postoperative hematoma: A 5-year survey and identification of avoidable risk factors. Neurosurgery 35(6): 1061-1064.
- Rapana A, Lamaida E, Pizza V (1998) Multiple postoperative intracerebral haematomas remote from the site of craniotomy. Br J Neurosurg 12(4): 364-368.
- Dinc C, Iplikcioglu AC, Bikmaz K, Navruz Y (2008) Intracerebral haemorrhage occurring at remote site following evacuation of chronic subdural haematoma. Acta Neurochir (Wien) 150(5): 497-499.
- Konig A, Laas R, Herrmann HD (1987) Cerebellar haemorrhage as a complication after supratentorial craniotomy. Acta Neurochir (Wien) 88(3-4): 104-108.
- Seoane E, Rhoton AL (1999) Compression of the internal jugular vein by the transverse process of the atlas as the cause of cerebellar hemorrhage after supratentorial craniotomy. Surg Neurol 51(5): 500-505.
- Friedman JA, Piepgras DG, Duke DA, McClelland RL, Bechtle PS, et al. (2001) Remote cerebellar hemorrhage after supratentorial surgery. Neurosurgery 49(6): 1327-1340.
- Naik V, Goyal N, Agrawal D (2001) Pin site bilateral epidural hematoma: A rare complication of using mayfield clamp in neurosurgery. Neurol India 59(4): 649-651.
- Honegger J, Zentner J, Spreer J, Carmona H, Schulze BA (2002) Cerebellar hemorrhage arising postoperatively as a complication of supratentorial surgery: a retrospective study. J Neurosurg 96(2): 248-254.
- Garg K, Tandon V, Sinha S, Suri A, Mahapatra AK, et al. (2014) Remote site intracranial hemorrhage: Our experience and review of literature. Neurol India 62: 296-302.
© 2022 Amit Kumar Ghosh. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






