- Submissions

Full Text
Techniques in Neurosurgery & Neurology
Acute Subdural Hematoma Post Spinal Anesthesia in a Parturient
Matouk M*, Kebiri Y and Benmouhoub N
Department of Anesthesia, Algeria
*Corresponding author: Matouk M, Department of Anesthesia, Algeria
Submission: April 04, 2022;Published: April 27, 2022

ISSN 2637-7748
Volume5 Issue1
Abstract
Introduction: Intracranial Subdural Hematoma (SDH) is a rare complication after spinal anesthesia, diagnosis is most often difficult. Objective of the work to report the case of a SDH post spinal anesthesia for cesarean section.
Observation: 29-year-old patient without medical ATCDS, already operated on by caesarean section under spinal anesthesia without incident, the preoperative biological assessment was without anomalies, the spinal anesthesia was performed in a half-sitting position in a single attempt, the intraoperative period was uneventful incidents. On postoperative day 1, onset of headaches on emergence, treated with perfalgan then caffeinated paracetamol per os and rehydration, she left the clinic with 8-day thromboprophylaxis. At the 10th reappearance of the headaches, the patient sees her gynecologist again who prescribes aspegic 100mg. The headaches become resistant to treatment and appearance of visual blurring of the right eye, seen by an ophthalmologist whose examination was normal. He completes the exploration with a cerebral CT scan which reveals a 14mm right hemispherical subdural hematoma with commitment under falcoriel. The hematoma was drained by two burr holes under sedation with placement of a drain The postoperative follow-up was favorable with a cerebral CT scan after removal of the drain showing the absence of a residual collection. A CT angiography eliminated an arteriovenous malformation and a dosage of coagulation factors returned without abnormalities.
Discussion: Intracranial SDH is a rare complication after spinal anesthesia, its ignorance can lead to serious or even fatal sequelae. Its physiopathology is explained by a persistence of the hard merian breach leading to intracranial hypotension causing a displacement of the neuraxis, from various causes. The reported case clearly illustrates that the first manifestations are identical to post-dural puncture headaches.
Conclusion: Severe and progressive headache after spinal anesthesia should be considered as an alert for an intracranial complication: post-spinal anesthesia subdural hematoma is a rare but important complication to be aware of by all practitioners in view of its severity.
Introduction
Intracranial subdural hematoma is a rare complication in spinal anesthesia diagnosis may be difficult initially due to the similitary of symptoms to post dural puncture headaches but neglecting them can lead to serious complications [1].
Observation
We report the case of a 29-year-old patient with no medical history already operated for a cesarean section under spinal anesthesia without incident, l and classified ASA I, the spinal anesthesia was performed in a semi-seated position in a single attempt without incident. A day after postoperative headache on emergence, treated symptomatically peros, the discharge at home is done with a thromboprophylaxis of 8 days. At the 10th reappearance of the headaches, the patient sees her doctor again who prescribes aspirin 100mg which worsened the symptoms: headaches resistant to treatment and appearance of visual blurring in the right eye, seen by an ophthalmologist who’s the examination was normal; it completes the exploration by a cerebral CT scan revealing a 14mm right hemispherical subdural hematoma with falcorial involvement. The postoperative outcome was favorable with a control brain CT after removal of the drain showing the absence of a residual collection. A CT angio ruled out an arteriovenous malformation and a coagulation factor assay returned without abnormalities (Figures 1-3); [2-4].
Figure 1:The hematoma was drained by two trephine holes under sedation with placement of a drain.
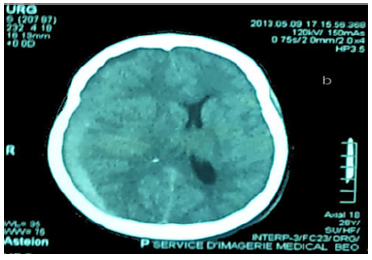
Figure 2:

Figure 3:

Discussion
Intracranial HSD is a rare complication after spinal anesthesia, its ignorance can lead to serious or even fatal sequelae. Its pathophysiology is explained by a persistence of the hard merian breach causing intracranial hypotension at the origin of a displacement of the neuraxis, depending on the gravity which exerts pressure on the bridging veins causing hemorrhage in the subdural space. These veins have a thinner wall in the subdural space than in the subarachnoid space.
The main causes:
a) excessive loss of CSF from multiple puncture attempts, the
use of large gauge or sharp-edged needles
b) the existence of a background of dehydration or of a
pre-existing neurological disease such as cerebral aneurysms or
arteriovenous malformations
c) the use in the pre- or post-operative periods of
anticoagulant drugs.
d) cortical atrophy or pregnancy.
The reported case illustrates that the first manifestations are identical to those of the post dural puncture headaches, namely the worsening in an orthostatic position and improving in strict decubitus which complicated the diagnosis initially, thereafter there was loss of postural character but dominated by ophthalmological signs [5].
Conclusion
The severe and progressive headache after spinal anesthesia should be considered as an alert for an intracranial complication: the subdural hematoma post spinal anesthesia is a rare complication but important to know by all practitioners given its severity. There is a definite interest in monitoring all patients with headaches after spinal anesthesia in order to facilitate early diagnosis, reduce morbidity and mortality and really know the incidence of this complication [6].
References
- Kayacan N, Arici G, Kardhi B, Erman M (2004) Acute subdural haematoma after accidental dural puncture during epidural anaesthesia. Int J Obstet Anesth 13(1): 47-49.
- Amorim JA, Remígio DSCA, Damázio FO, Marcos AGB (2010) Intracranial subdural hematoma post-spinal anesthesia: report of two cases and review of 33 cases in the literature. Rev Bras Anestesiol 60(6): 620-629.
- Katricioglu K, Aydin O, Ozkalanli MY, Serdar S (2009) Cranial subdural haematoma: a rare complication of spinal anaesthesia. Eur J Anaesthesiol 26(9): 793-795.
- Gaiser R (2006) Postdural puncture headache. Cur Opin Anesthesiol 19(3): 249-253.
- Mokri B (2003) Headaches caused by decreased intracranial pressure: diagnosis and management. Curr Opin Neurol 16(3): 319-326.
- Turnbull DK, Shepherd DB (2003) Post-dural puncture headache: pathogenesis, prevention and treatment. Br J Anaesth 91(5): 718-729.
© 2022 Matouk M. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






