- Submissions

Full Text
Techniques in Neurosurgery & Neurology
Post COVID Grisel’s Syndrome, is there any Association?
Ali Riazi, Firooz Salehpour, Masih Sabouri, Bahram Aminmansour, Majid Rezvani, Farhad Mirzaee, Bohlool Asghari Kaleibar and Ata Mahdkhah*
Department of Neurosurgery, Iran
*Corresponding author: Ata Mahdkhah, Department of Neurosurgery, Iran
Submission: November 10, 2021;Published: January 24, 2022

ISSN 2637-7748
Volume4 Issue5
Abstract
Grisel’s Syndrome (GS) is a rare, non-traumatic and rotatory atlantoaxial subluxation. Upper airways, head and neck infections and surgical procedures are the main causes of this syndrome. Post COVID GS is not studied on the literature. Although we believe that COVID-19 spreading in upper airways, related immune response and over-relaxation of ligaments can lead to C1-C2 rotatory subluxation and GS, the exact pathophysiology of this process is unknown. We conclude that the virus may present with an extensive range of manifestations such as GS and should be considered in children with COVID-19 infection. As a result, we report 3 GS cases associated with COVID-19 infection for the first time.
Introduction
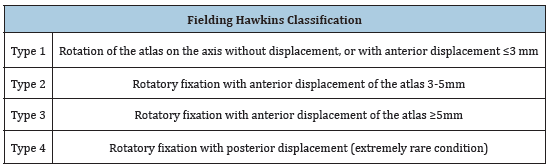
Grisel’s Syndrome (GS) is a rare, non-traumatic and rotatory atlantoaxial subluxation. It is usually detected in children. Upper airways, head and neck infections and surgical procedures are the main causes of this syndrome [1-12]. History of the mentioned items and patients presenting with painful torticollis, fever and reduced range of motion should be notified. Anterior-posterior Direct Cervicography (DCG), Cervical Computerized Tomography (CT) and Magnetic Resonance Imaging (MRI) are usually recommended to confirm diagnosis and classify the patients. Fielding-Hawkins classification can be used to evaluate these cases (Table 1). Based on type and time of syndrome, supportive and surgical therapy is recommended [13,14]. Clinical symptoms and signs of CNS (Central Nervous System) and PNS (Peripheral Nervous System) involvement can be seen in up to 25% of SARS-CoV-2 (severe acute respiratory syndrome coronavirus-2) infected patients. Some researchers propose the term “euro-COVID syndrome” for presentations with pure CNS and PNS presentations at onset. Post COVID GS is not studied in the literature. As a result, we report 3 GS cases associated with COVID-19 infection for the first time.
Table 1: Fielding hawkins classification.
Description of Cases
Case 1
A 9-year-old female patient was admitted with painful torticollis and reduced cervical range of motion. She had a history of hospitalization for 4 days due to COVID-19 infection one week before. Her past chief complaint of first admission was fever and cough and positive subjective or objective clinical findings were malaise, dyspnea, and anosmia. Moreover, the standard diagnostic method by real-time reverse transcription polymerase chain reaction (rRT-PCR), from a nasopharyngeal swab confirmed the detection of the virus’ nucleic acid. At this time, there was not any complication related to COVID-19 on physical examination. Neurological assessment was also normal. Anterior-posterior DCG showed Cock-robin position and cervical CT detected asymmetric thickening of the left parapharyngeal soft tissue and rotator atlantoaial subluxation (Type 2 F-H). She was assessed by neurosurgery department and recommendations of bed rest, immobilization, physical therapy, reduction, antibiotics, and antiinflammatory treatment. Clinical manifestations slowly decreased, and the patient was symptom free after one month.
Case 2
A 7-year-old male patient was hospitalized with clinical manifestations including fatigue and breathing difficulties. rRTPCR detected COVID-19 infection. 5 days after admission, her neck was painful and deviated severely. Physical examination showed fever and torticollis and cervical imaging’s (DCG and CT) confirmed the similar positive findings of Case 1 (Type 2 F-H). Physical limitation, manipulation, traction, reduction, antibiotics, and antiinflammatory medications lead to full recovery after 3 weeks.
Case 3
An 8-year-old female with a 2-week history of recent COVID-19 infection manifestations such as fever, cough, nausea, and fatigue presented to the neurosurgery clinic with painful torticollis, fever and reduced range of motion. She had a documented positive rRTPCR. Similar diagnostic (DCG and CT, Type 3 F-H) and therapeutic (conservative therapy) approaches could not reach to recovery after 3 months. MRI showed C1-C2 rotatory subluxation with narrowing of cervicomedullary junction. Unfortunately, Halo application was not successful. Consequently, we decided to have C1-C2 cervical fusion. This led to complete resolution of subluxation without adverse outcomes.
Discussion
Based on literature, there are different symptoms and signs related to SARS-CoV-2 including dizziness, headache, altered mental state, meningitis, encephalitis, ischemic stroke, hemorrhagic stroke, venous sinus thrombosis, seizure, subarachnoid hemorrhage, neuroimmunology disorders, movement disorders, smell and/ or taste impairment, Guillain-Barre syndrome, myasthenia gravis, myositis, rhabdomyolysis, myopathy, neuropathy, and hydrocephalus. As mentioned earlier, there is not any association between this infection and GS in the literature, but we can focus on this possibility [15-18]. Moreover, there is not any history of even mild trauma in these patients. Clinical manifestations of GS were initially described by Charles Bell in 1830. After one century, the French physician Grisel reported 2 cases of C1-C2 subluxation after nasopharyngeal inflammation [19-25]. Probable causes of higher rate of GS in children are immature bone structure, more horizontal facets, larger synovial folds, adenotonsillar hypertrophy, further hypermobile C1-C2, more laxity of ligaments and elevated rate of infections. Totally, there are 183 reported cases of GS in the literature. Range of patients is between 4.5-14 years. 61.5% of cases were involved due to upper respiratory tract and head/ neck infections and 36% were postsurgical ones. Type 1 was the most common F-H grade and most of patients (96%) were treated conservatively [26,27]. As you can see, our cases are matched with these data. Although we believe that COVID-19 spreading in upper airways, related immune response and over-relaxation of ligaments can lead to C1-C2 rotatory subluxation and GS, the exact pathophysiology of this process is unknown.
Conclusion
We conclude that the virus may present with an extensive range of manifestations such as GS and should be considered in children with COVID-19 infection.
References
- Fielding JW, Hawkins RJ, Hensinger RN, Francis WR (1978) Atlantoaxial rotary deformities. Orthopedic Clinics of North America 9(4): 955-967.
- Dağtekin A, Kara E, Vayısoğlu Y (2011) The importance of early diagnosis and appropriate treatment in Grisel's syndrome: report of two cases. Turk Neurosurg 21(4): 680-684.
- Hettiaratchy S, Ning C, Sabin I (1998) Nontraumatic atlanto-occipital and atlantoaxial rotatory subluxation: case report. Neurosurgery 43(1): 162-165.
- Lopes DK, Li V (1998) Midcervical postinfectious ligamentous instability: a variant of Grisel's syndrome. Pediatr Neurosurg 29(3): 133-137.
- Park SW, Cho KH, Shin YS (2005) Successful reduction for a pediatric chronic atlantoaxial rotatory fixation (Grisel syndrome) with long-term halter traction: Case report. Spine 30(15): E444-E449.
- Beyazal MS, Demirok D, Çapkın E, Usul H, Tosun M (2011) Grisel’s syndrome: a case report. Turkish Journal of Rheumatology 26(3): 243-247.
- Bocciolini C, Dallolio D, Cunsolo E, Cavazzuti PP, Laudadio P (2005) Grisel's syndrome: a rare complication following adenoidectomy, Acta Otorhinolaryngologica Italica 25(4): 245-249.
- Ortega EG, Alcon JJ, Alvarez PJ, Sebastia V, Juncos M, et al. (2011) Eponym: Grisel syndrome. European Journal of Pediatrics 170(8): 965-968.
- Harma A, Firat (2008) Grisel syndrome: nontraumatic atlantoaxial rotatory subluxation. Journal of Craniofacial Surgery 19(4): 1119-1121.
- Martínez L, Morales T, Cornejo VF (2003) Inflammatory C2-3 subluxation: a Grisel’s syndrome variant. Archives of Disease in Childhood 88(7): 628-629.
- Deichmueller CM, Welkoborsky HJ (2010) Grisel's syndrome-a rare complication following small operations and infections in the ENT region. European Archives of Oto-Rhino-Laryngology 267(9): 1467-1473.
- Youssef K, Daniel S (2009) Grisel syndrome in adult patients. Report of two cases and review of the literature. Canadian Journal of Neurological Sciences 36(1): 109-113.
- Grisel P (1930) Enucleation de latlas et toricollis nasopharyngien. Presse Medicale 38: 50-53.
- Wilson BC, Jarvis BL, Haydon RC (1987) Nontraumatic subluxation of the atlantoaxial joint: Grisel’s syndrome. Ann Otol Rhinol Laryngol 96(6): 705-708.
- Bocciolini C, Dallolio L, Cunsolo E, Cavazzuti PP, Laudadio P (2005) Grisel’s syndrome: a rare complication following adenoidectomy, Acta otorhinolaryngol Ital 25(4): 245-249.
- Spennato P, Nicosia G, Rapanà A (2015) Grisel syndrome following adenoidectomy: surgical management in a case with delayed diagnosis. World Neurosurgery 84(5): 7-12.
- Per H, Canpolat M, Tümtürk A (2014) Different etiologies of acquired torticollis in childhood. Child Nerv Syst 30(3): 431-440.
- Salem KMI, Radhakrishnan A, Behrbalk E, Boszczyk BM (2016) The surgical management of atlanto-axial subluxation in juvenile rheumatoid arthritis. European Spine Journal 25(7): 2108-2114.
- Iaccarino C, Francesca O, Piero S (2019) Grisel’s syndrome: non-traumatic atlantoaxial rotatory subluxation-report of five cases and review of the literature. Acta Neurochirur Suppl 125: 279-288.
- Yu KK, White DR, Weissler MC, Pillsbury HC (2003) Nontraumatic atlantoaxial subluxation Grisel syndrome: a rare complication of otolaryngological procedures. Laryngoscope 113(6): 1047-1049.
- Akbay A, Bilginer B, Akalan (2014) Closed manual reduction maneuver of atlantoaxial rotatory dislocation in pediatric age. Child’s Nervous System 30(6): 1083-1089.
- Lee SC, Lui TN, Lee ST (2002) Atlantoaxial rotatory subluxation in skeletally immature patients. Br J Neurosurg 16(2): 154-157.
- Agarwal J, Tandon MS, Singh D, Ganjoo P (2013) Quadriplegia in a child following adenotonsillectomy. Anaesthesia 68(5): 523-526.
- Osiro S, Tiwari KJ, Matusz P, Gielecki J, Tubbs RS (2012) Loukas, Grisel’s syndrome: a comprehensive review with focus on pathogenesis, natural history, and current treatment options. Child’s Nervous System, 28(6): 821-825.
- Fath L, Cebula H, Santin MN, Coca A, Debry C (2018) The Grisel’s syndrome: a non-traumatic subluxation of the atlantoaxial joint. Neurochirurgie, 64(4): 327-330.
- Battiata AP, Pazos G (2004) Grisel’s syndrome: the two-hit hypothesis-a case report and literature review. Ear Nose Throat J 83(8): 553-555.
- Deichmueller CMC, Welkoborsky HJ (2010) Grisel’s syndrome-a rare complication following small operations and infections in the ENT region. Eur Arch Otorhinolaryngol 267(9): 1467-1473.
© 2022 Ata Mahdkhah. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






