- Submissions

Full Text
Techniques in Neurosurgery & Neurology
Tumor Darkening Sign: Image Finding that May Correspond to a Successful Pre-Surgical Embolization in Meningiom
Segura Hernández Andrés1, Robles Robles Vanesa2*, Fonnegra Pardo Julio Roberto1,3, Fonnegra Caballero Andrés1,3 and Diez Palma Juan Carlos1,3
1Neurosurgery Residency Program; Neurosciences Institute, Colombia
2School of Medicine, Colombia
3Department of Neurosciences, Colombia.
*Corresponding author: Vanesa Robles Robles, School of Medicine, Colombia
Submission: November 10, 2021;Published: December 01, 2021

ISSN 2637-7748
Volume4 Issue4
Abstract
Objective: The present work seeks to describe the change in imaging characteristics in brain magnetic resonance in pre- and post-embolization studies in meningiomas in the plan of being taken to surgical resection.
Justification: The pre-surgical embolization of intracranial meningiomas has shown benefits related mainly to less intra-operative bleeding and length of hospital stay, as well as greater technical ease in resection due to changes due to liquefactive necrosis suffered by the tumor.
Method: A representative case is presented with pre- and post-embolization imaging studies performed on a patient who was subsequently taken to surgical resection of a meningioma of the posterior third of the sickle, in which there is a marked decrease in signal intensity in MRI study, especially in images with information in T1, sequence with contrast medium, possibly related to vascular and microvascular obstruction that is achieved after embolization of the arteries afferent to the lesion.Conclusion: The loss of enhancement after the administration of contrast medium (Gadolinium) in the images by cerebral magnetic resonance with information in post-embolization T1, evidences the vascular and microvascular lesion that is sought with the administration of embolization material, which serves as an imaging sign of successful or satisfactory embolization prior to being taken to surgery.
Keywords:Meningiomas; Embolization; Magnetic resonance; Contrast enhancement; Surgical resectio
Introduction
Meningiomas are the most frequent intracranial tumors in general population [1-4], according to their histological characteristics they can be divided into three groups: typical, atypical and anaplasic according to the fourth WHO classification, being the most frequent ones the typical type [4]. Within the management options, it should be individualized according to location, size, age, comorbidities, functional status and desire of the patient, with surgery as the first option, additionally stereotactic radiosurgery, fractional radiotherapy and systemic treatment [4]. When surgical management is indicated, pre-operative embolization has shown to influence positively the decrease in intra-operative bleeding and the length of hospital stay, as well as greater technical ease at the time of resection due to the processes of ischemia and Endo tumoral liquefactive necrosis [4]. In the present work, a representative case of a meningioma of the brain sickle was chosen, which was surgically managed, and a pre-operative embolization was performed one day before surgery, 12 hours after the embolization, it was taken to brain magnetic resonance imaging to perform of the complement. with neuro-navigation protocol to obtain images with information in T1, sequence with contrast medium, where a poor enhancement with it is shown, an effect that we have named tumor darkening and that possibly corroborates an adequate embolization.
Case Presentation
A 44-year-old male patient, a systems engineer, with no significant disease history, who initially consults to Otorhinolaryngology for 6 months of right tinnitus, associated with occasional vertigo, the neurological examination is normal, they request simple cerebral magnetic resonance imaging where evidence extra-axial occipital right para-sagittal lesion adjacent to the tentorial surface, hypointense in 1T1, isointense in T2, without associated vasogenic edema, subsequent study with the administration of gadolinium evidence high enhancement, with Dural pedicle in relation to the right surface of the posterior third of the brain sickle. There is an indication of surgery previous embolization which was performed with micro-particles at the level of the afferent vessel from the posterior meningeal artery branch of the occipital artery which emerges from the left external carotid artery, procedure performed one day before surgery. In the course of the night after tumor embolization, brain magnetic resonance imaging is performed with a neuro-navigation proto test in T1 sequences with administration of Gadolinium, where the low signal intensity in almost the entire lesion is striking. The next day the patient is taken to surgery without incidents with minimal intra-operative bleeding, is taken to intensive care unit for 24 hours, with subsequent transfer to the general hospital ward for another 24 hours and subsequent discharge (Figure 1-6).
Figure 1: Magnetic resonance prior to tumor embolization. Extra-axial lesion adjacent to the posterior third of the
right para-sagittal brain sickle that shows intense enhancement with the administration of the contrast medium.
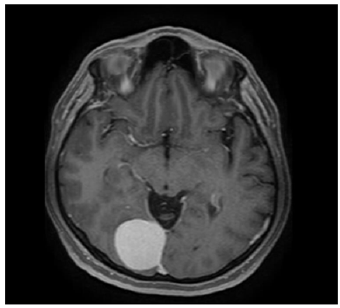
Figure 2:Magnetic resonance after tumor embolization. Extra-axial lesion adjacent to the posterior third of the right
para-sagittal brain sickle showing poor and irregular enhancement with the administration of the contrast medium.
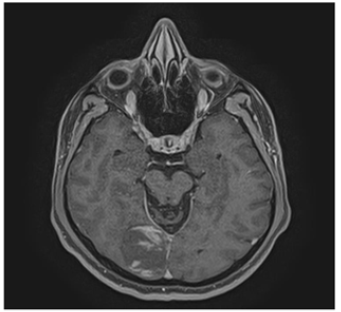
Figure 3: Magnetic resonance after tumor embolization. Extra-axial lesion adjacent to the posterior third of the right
para-sagittal brain sickle showing poor and irregular enhancement with the administration of the contrast medium.
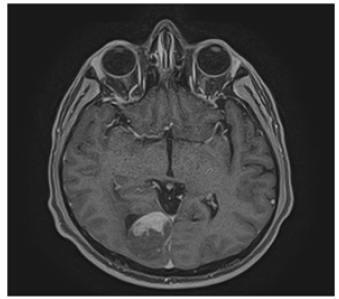
Figure 4: Cerebral arteriography. Irrigation from the posterior meningeal artery, branch of the occipital artery,
branch of the external carotid artery.
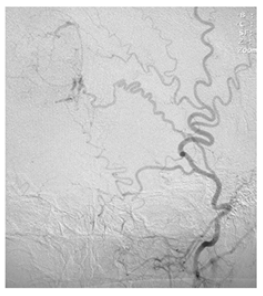
Figure 5: Cerebral arteriography. Supraselective embolization with microparticles of the posterior meningeal artery,
branch of the occipital artery, branch of the external carotid artery.

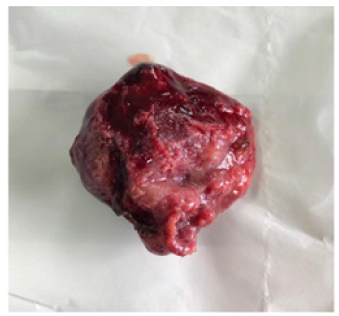
Figure 6: Ex vivo tumor. Anatomo-pathological specimen of meningioma of the resected cerebral sickle.
Discussion
Classically, meningiomas have been described as highly vascularized tumors, which give them an important risk of bleeding, transfusion requirement and increased complications after surgical resection, especially in patients older than 70 years, with an index Karnofsky under 70 and in those surgeries that exceed four Hours [5]. Therefore, performing a previous embolization suggests a decrease in morbidity associated with surgical treatment. The preoperative embolization of this type of tumors has shown a reduction in surgical time, a decrease in bleeding and a greater probability of success with respect to their complete resection; so far different materials have been used during embolization (particles of polyvinyl alcohol PVA, ethylene-vinyl alcohol ONIX, Coils, Fibrin, among others), which is done by introducing microcatheters to the main blood vessels that supply meningiomas, frequently branches of the external carotid artery (middle meningeal, accessory meningeal, ascending pharyngeal, occipital) and others of the internal carotid [6]. Some of the recommendations for preoperative embolization of meningiomas include size (>4cm in diameter), irrigation from the external carotid (at least 50% due to easy access), hyper-vascular tumors, located in eloquent areas and not calcified [6]. Other studies show that completes embolization of these tumors is greater in those meningiomas located at the parasagittal level, in the convexity, or with irrigation from the ascending pharyngeal artery [7]
The complications described secondary to the embolization of meningiomas include ischemic strokes, intracranial hemorrhages, cerebral edema and cranial nerve paralysis, which could reach an incidence according to the literature up to 16%; other nonneurological complications include arteriovenous fistulas, inguinal hematomas and scalp necrosis; the surgical complications of patients who were previously embolized in contrast to those who were taken only to surgical resection, are significantly less in the first group, with respect to the decrease in the time of surgery and reduction of bleeding [8,9]. Additionally, in a follow-up carried out up to two months after embolization of meningiomas that were not surgically resected after endovascular therapy, it has been shown that there is a decrease in tumor volume and associated perilesional edema, which on the one hand would facilitate surgical treatment and on the other, it would indicate usefulness of embolization of meningiomas in palliative therapies [10]. However, in the vast majority of cases, the time that elapses from embolization to resection of meningioma is usually less than 24 hours, which is mainly related to lower bleeding rates, but also a decrease in tumor volume. Performing surgery after 7 days of embolization may result in revascularization and the appearance of collateral circulation in meningioma [11].
Preoperative embolization of meningiomas can decrease intraoperative blood loss as mentioned above, which is estimated between 200 milliliters to 2.2 liters, so the calculation of such loss has a fundamental clinical value; several studies have found a relationship between the extent of contrast in Brain Magnetic Resonance Imaging (MRI) and blood loss during surgery, concluding that in a successful tumor embolization there is a decrease in the contrast medium that enhances the tumor in a neuroimaging of post control; this translates into a percentage measurement of the improvement in enhancement with the administration of contrast in MRI being : mild (<30%), moderate (30% -60%), extensive (60% -90%) and complete (>90%), it should be noted that the significant result of bleeding reduction is in the latter category [12]. Therefore, the presence of contrast media in the tumor and the volume fraction thereof that enhances after embolization correlates with vascularization and therefore with intraoperative blood loss. In addition to this, a significant volume of the tumor and male patients have also been linked to a much greater blood loss [12]. Other findings that can be found in Magnetic Resonance after meningioma embolization that indicate tumor necrosis are tumor size increase associated edema and of course decrease in enhancement with the contrast medium, even being less than 90% (mild, moderate, or extensive) also has an important effect in reducing bleeding during surgical resection [13].
Histopathological studies performed on resected meningiomas, that were previously embolized, demonstrate ischemic cell changes and vascular fibrinoid necrosis, which in Magnetic Resonance result in a significant signal decrease in the apparent diffusion coefficient ADC, relative cerebral blood volume rCBV, and relative cerebral blood flow rCBF that will often be present from 6 hours to 48 hours post-embolization [14]. In addition to MRI, cranial computed tomography (CAT) and angiography are useful for assessing devascularization post-embolization; the angiography demonstrates the absence of tumor staining with the contrast medium; on the other hand, CT and MRI with contrast also show some focal defects compatible with areas of tumor infarction. The advantage of MRI is that it allows the evaluation of tumor blood flow before and after embolization with multiple techniques, in which it is evident that there is a decrease in tumor perfusion after endovascular therapy.
Conclusion
The loss of enhancement after the administration of contrast medium (Gadolinium) in the images by cerebral magnetic resonance with information in post- embolization T1, evidences the vascular and microvascular lesion that is sought with the administration of embolization material, which serves as an imaging sign of successful or satisfactory embolization prior to being taken to surgery, however more studies evaluating its frequency and correlation with both post-embolization angiography and intraoperative bleeding should be carried out.
References
- Brastianos PK, Galanis E, Butowski N, Chan JW, Dunn IF, et al. (2019) Advances in multidisciplinary therapy for meningiomas. Neuro Oncol 21(1): 18-31.
- Chen L, Li D, Lu Y, Hao B, Cao Y (2019) Literature review preoperative embolization versus direct surgery of meningiomas: A+ meta-analysis. World Neurosurg 128: 62-68.
- Louis DN, Perry A, Reifenberger G, Von Deimling A, Figarella BD, et al. (2016) The 2016 world health organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131(6): 803-820.
- Ostrom QT, Gittleman H, Truitt G, Boscia A, Kruchko C (2018) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2011-2015. Neuro Oncol 20(4): 1-86.
- Bartek J, Sjåvik K, Förander P, Solheim O, Gulati S, et al. (2015) Predictors of severe complications in intracranial meningioma surgery: a population-based multicenter study. World Neurosurg 83(5): 673-678.
- Raper DMS, Starke RM, Henderson F, Ding D, Simon S, et al. (2014) Preoperative embolization of intracranial meningiomas: Efficacy, technical considerations, and complications. AJNR 35(9): 1798-1804.
- Barros G, Feroze AH, Sen R, Kelly CM, Barber J, et al. (2019) Predictors of preoperative endovascular embolization of meningiomas: Subanalysis of anatomic location and arterial supply. J Neurointerv Surg Neurintsurg 2019-015129.
- Singla A, Deshaies EM, Melnyk V, Toshkezi G, Swarnkar A, et al. (2013) Controversies in the role of preoperative embolization in meningioma management. Neurosurg Focus 35(6): E17.
- Nakajima N, Fukuda H, Adachi H, Sasaki N, Yamaguchi M, et al. (2017) Long-term volume reduction effects of endovascular embolization for intracranial meningioma: preliminary experience of 5 cases. World Neurosurg 105: 591-598.
- Chun JY, McDermott MW, Lamborn KR, Wilson CB, Higashida R, et al. (2002) Delayed surgical resection reduces intraoperative blood loss for embolized meningiomas. Neurosurgery 50(6): 1231-1237.
- Nguyen HS, Janich K, Doan N, Patel M, Li L, et al. (2017) Extent of T1+C intensity is a predictor of blood loss in resection of meningioma. World Neurosurgery 101: 69-75.
- Ali R, Khan M, Chang V, Narang J, Jain R, et al. (2016) MRI pre- and post-embolization enhancement patterns predict surgical outcomes in intracranial meningiomas. J Neuroimaging 26(1): 130-135.
- Gruber P, Schwyzer L, Klinger E, Burn F, Diepers M, et al. (2018) Longitudinal imaging of tumor volume, diffusivity, and perfusion after preoperative endovascular embolization in supratentorial hemispheric meningiomas. World Neurosurg 120: e357-e364.
- Kawaji H, Koizumi S, Sakai N, Yamasaki T, Hiramatsu H, et al. (2013) Evaluation of tumor blood flow after feeder embolization in meningiomas by arterial spin-labeling perfusion magnetic resonance imaging. J Neuroradiol 40(4): 303-306.
© 2021 Robles Robles Vanesa. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






