- Submissions

Full Text
Techniques in Neurosurgery & Neurology
Comparison of Montreal Cognitive Assessment (Moca) and Mini-Mental State Examination (MMSE) for the Detection of Cognitive Disorders
Román Esquivelb JV2, Cruz Rosalesa JL1,2,Hernándeza SP1,2, Medinaa JMS1,3and Leyvaa IR1,2*
1Faculty of Medicine, Mexico
2Service of Neurology, Central Hospital Dr. Ignacio Morones Prieto, Mexico
3Faculty of Medicine, Mexico
*Corresponding author:Avenida Venustiano Carranza, Los Filtros, CP 78210 San Luis Potosí, SLP México
Submission: July 03, 2019; Published: July 10, 2019

ISSN: 2576-9200 Volume2 Issue2
Abstract
Objective: To analyze the result of the application of two questionnaires for cognitive screening: Montreal Cognitive Assessment (MoCA) and Mini-Mental State Examination (MMSE) in patients that attended to the Neurology Department by assessing the effectiveness in the detection of Mild Cognitive Impairment (MCI) and Dementia.
Material and methods: A cross-sectional study was conducted to calculate the sample size considering a sensitivity of 80%, specificity of 90%, confidence interval of 95%, and a precision of 10%. The data was analyzed using RCMDR package of R 95% confidence interval. The sensitivity, specificity, positive and negative predictive values were calculated, taking the MoCA as the gold standard. A logistic regression analysis was done to evaluate the variables associated with the diagnosis.
Results: Two hundred and twelve subjects were evaluated according to the inclusion criteria. The variables age, gender, school years, independence, and illness were considered. The MoCA results showed 35 subjects with probable MCI, averaging 45 years old, basic scholar education 82.7% (n=29), and predominantly females. The MMSE results showed nine subjects with probable MCI, age ranged between 42-75 years old, and predominantly females (88%). A prevalence of 16.5% for cognitive deterioration was found. The MMSE reported a sensitivity of 23% and a specificity of 94.7% with a PPV of 88.9% and an NPV of 86.7%.
Conclusion: The MMSE was less sensitive compared to the MoCA which was more sensitive for the detection of cognitive impairment in a tested population. Outstanding schooling represents the most significant protective factor to develop Cognitive Impairment or Dementia.
Keywords: Montreal cognitive assessment (MoCA); Mild cognitive impairment (MCI); Montreal cognitive assessment spanish version (MoCA-S); Central nervous system (CNS); Cognitive impairment (CI)
Introduction
Human aging is associated to significant structural and functional changes in almost all organs and body systems including the Central Nervous System (CNS). Many years of research on brain aging indicate that there is a reduction in the weight and volume of the brain of around 2% after each decade. These changes occur even in healthy old adults who do not show significant cognitive function deterioration [1]. In recent years brain images (Magnetic Resonance) have shown that the CNS presents changes associated to age and that these changes are more evident in some areas of the brain than in others [2]. Specifically, the main changes that occur are in areas of the frontal, parietal and temporal cerebral cortex. Demographic aspects, lifestyle, health, and genetic characteristics significantly affect cognitive functions causing slow and continuous changes. The cognitive aspects in which aging leads to relevant changes are memory, attention, learning, speed of information processing, language, visuospatial, visuoperceptive and visuoconstructive abilities [3]. In general, the debate exists around two fundamental issues: On one side to establish which cognitive changes can be considered as part of healthy aging and on the other side the knowledge of whether brain aging and degenerative dementias constitute different processes. Neither of these questions has been completely answered but in recent years the interest on them has grown enormously due to the discovery that Alzheimer’s disease (AD), which is the most common type of degenerative dementia, has a long preclinical period. Therefore, there is the possibility of intervening and reversing or stopping the process before the onset of symptoms [4,5]. Brain aging does not necessarily have to be linked to overt cognitive impairment. However, a high percentage of people reaches elderly without presenting symptoms of dementia although their cognitive status is relatively low since adulthood. The principal need is to identify those subjects without dementia but with an increased risk of developing it.
Currently, the first evaluation of a patient suspected of having cognitive impairment was performed through cognitive screening tests or screening tests. These are low-influenced by sociocultural factors [6]. However, the screening tests are indicative tests, not clinical diagnoses. A diagnose should be based on a detailed study of cognitive functions by a specialist. The cognitive screening tests with higher international recognition in primary care and validated are Mini-Mental State Examination (MMSE), Test Clock, Short Portable Mental Status (SPMSQ), Seven minutes test, Montreal Cognitive Assessment (MoCA), Leganés cognitive test (LCT), and Abbreviated Mental Test (AMT). From old previous tests, the most used worldwide and known is the Mini-Mental State Examination (MMSE) which was developed by Folstein et al. [7] and is internationally the most widely used instrument to provide a general measure of cognitive impairment in the clinic. It requires approximately 5 to 10 minutes and consists of 11 items that sum a maximum score of 30 points: High, individually assessing orientation (10 points), fixation (3), concentration and calculation (5), memory (3), language (8) and constructional function (1). The disadvantages are that this test cannot be applied to illiterates, it has a reduced sensitivity in the mild stages of dementia, and the patient’s cultural level requires corrections [8]. Another test is the Montreal Cognitive Assessment (MoCA), reported by Nasreddine et al. in 2005. This test is a simple tool to assess mild cognitive impairment and mild Alzheimer’s diseases. This was designed after difficulties imposed found for the Mini-Mental State Examination (MMSE) in the diagnosis and differentiation of mild Alzheimer’s disease and MCI [9]. The test evaluates multiple cognitive domains briefly (10 minutes): Episodic memory, visuospatial ability, executive function, attention-concentration, language, and orientation. The original study showed excellent values of testretest reliability and constructed validity and better capacity than the MMSE for the detection of mild AD (100% versus 78%) [10]. MoCA’s translation into Spanish (MoCA-S) was published by Lozano et al. in 2009. This article provides preliminary data in favor of the questionnaire suggesting that it is useful for detecting of dementia but less practical for diagnosing of MCI. Early identification and intervention for mild cognitive impairment can help to detect, prevent and slow the development of dementia.
An on-time diagnosis of the mild cognitive impairment helps to improve cognitive performance. Thus, it delays or even prevents the onset of dementia. Currently, there is no known “cure” for significant degenerative cognitive impairment but some treatments may delay cognitive and functional impairment, or reduce behavioral and psychiatric symptoms. Therefore, an early detection is paramount [9]; mainly if the type of dementia was treatable (metabolic, infectious, immunological, deficiency, and others.). Ideally, a screening test should be well-accepted by subjects and should evaluate in a simple, brief and psychometrically effective way, the different cognitive domains with high sensitivity for detection. However, the influence of sociocultural variables and protective factors prevent the development of cognitive impairment (physical exercise, cognitive training, and sleep hygiene). Therefore, it is necessary to investigate if these tests are adequate for this population, which one is more sensitive, and if both are suitable or not to our practice. If confirmed, it would be ideal to use tests that help us in the detection of these diseases [11-16] to generate information that until now is subjectively known in our services, such as the incidence of Mild Cognitive Impairment and Dementia. In this study, we used the MoCA and the MMSE tests as screening. The objective of this study was to compare the results of two cognitive screening tests (MoCA and MMSE) for the detection of Mild Cognitive Impairment and Dementia.
Material and Methods
The study was conducted at the Neurology Department of the Hospital Central “Dr. Ignacio Morones Prieto”. A total of 212 subjects participated in the study according to the inclusion criteria. Data was obtained from March 2015 to October 2016. The control sheet contained the following information: date of recruitment, name and surname of the participant, age, gender, school years, independence and diagnosis. The MoCA and MMSE questionnaires were applied following the main control sheet only if the patient agreed his/her participation in the study. Subjects were divided in healthy individuals (without a diagnosis of disease) and ill patients (with a known diagnosis for Parkinson’s disease, headache, cerebrovascular event or epilepsy). The exclusion criteria considered subjects that did not want to participate in the study. We eliminated those patients whose applied tests were lost or could not be recovered. The sample size calculation was done using the Epidat statistical program using sensitivity of 80% and specificity of 90% with a confidence interval of 95% and an accuracy of 10%. This gave us 62 ill subjects and 35 healthy subjects a total of 97%, which were matched by age. The sample size was calculated considering patients who attend to the Neurologic Department at the Hospital Central “Dr. Ignacio Morones Prieto”. We used a nonprobabilistic sampling.
Statistical Analysis
Data was analyzed using R software Rcmdr package (version 3.2.2) using a 95% confidence interval. A descriptive analysis of the variables was carried out. Continuous variables were expressed as mean (± standard deviation) or median [range IQ1-IQ3] according to the distribution of the variables and the certain ones as frequencies. For the inferential statistics of the continuous variables (Table 1), a bivariate analysis with student’s t-test and Mann-Whitney U test was done according to the distribution of the variables. For the categorical Chi-square and Fisher’s exact test was done considering p values below 0.05 as significant. To simplify calculations, subjects were grouped by age ranges of 10 years interval. Sensitivity, specificity, positive and negative predictive values were calculated. MOCA Deterioration (presence/absence)~Years of schooling+Age+ Independence. The final model was: MOCA Deterioration (Table 2) (presence/absence)~Years of schooling+Age.
Table 1:MOCA deterioration (presence/absence)~years of schooling+age.
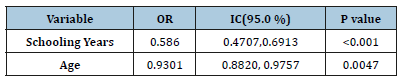
Table 2:Mini-mental deteriosssration (presence/ absence)~years of schooling.
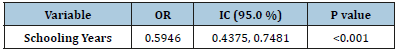
MMSE Deterioration (presence/absence)~Years of schooling+Age+INDEPENDENT. The final model was:
Mini-Mental Deterioration (presence/absence)~Years of schooling.
Gender
Most participants were females with 70.7% (150 out of 212).
Age
The age of the participants ranged between 40 and 84 years. The median age was 56.5 years (55.5±10 for females and 57±11 for male). The range of participation (Table 3) was similar in the four groups, being lower in the group of subjects older than 70 years with 9.91% (n=21).
Table 3:Characteristics of the population.
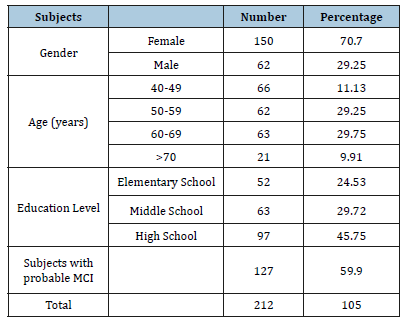
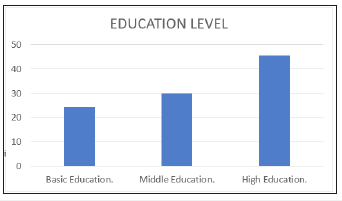
Education level
Most of the participants studied high school (more than 13 years) with a proportion of 45.7%. The average number of school years was 11±5 (Figure 1).
Figure 1:Distribution of the Population according to education level.
Independence
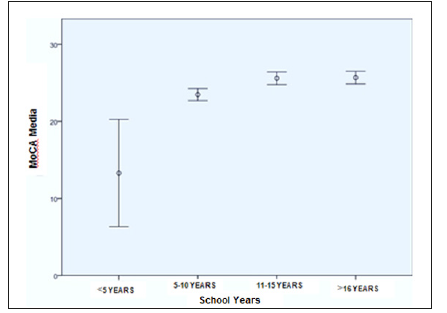
85.4% (n=181) of the patients were independent according to the Lawton IADL Scale with an average score of 21 points. The applied questionnaires reported for MoCA an average of 24.21±4.23. MMSE recorded an average of 26.91±3.02 (Table 4). Subjects with a probability of cognitive impairment (Figure 2) considering the MoCA test was 48.6% and for MMSE 11.3%. It is noteworthy that the lower score in both was observed in subjects with lower education level and illiterate (Figures 3 & 4). We observed 59.9% (n=127) patients with a probability of Cognitive Impairment.
Table 4:Descriptive statistics.
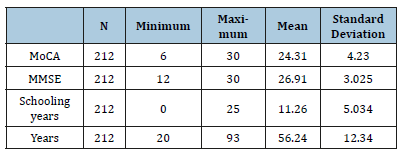
Figure 2:Relationship of schooling years with MoCA score.

Figure 3:Relation of schooling years with the MMSE score.
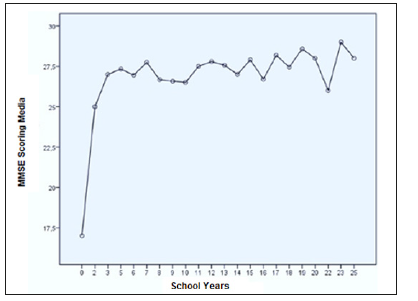
Figure 4:MoCA’s effectiveness in relation to school years.
Montreal Cognitive Assessment (MoCA)
There were 148 patients with a score below 26 points. Most of them were female representing 69.5% (103). Of these patients 49.32% had basic education (n=73). In the group of women 59 had with primary education, 20 middle education and 25 high education. Five subjects were illiterate. In the male group 14 subjects had basic education, five middle education and most of them high education (22 subjects). Of these subjects, nine women and five men were dependent according to the Lawton scale which represents a probability of Dementia mostly below 20 points.
Mini-Mental State Examination (MMSE)
We found 20 subjects with probable Cognitive Impairment (42 to 75 years). Eleven were female (88%) with a range of 40-49 years. Most of them had basic education (N=11), a total of 5 dependent
subjects were found.
Using a contingency table, a prevalence of 16.5% was obtained for cognitive deterioration. The MMSE test reported a sensitivity of 16.8%, a specificity of 99%, a PPV of 99%, and a NPV of 51% (Table 5). School years influence the MMSE and MoCA score with a P =0.0001. Higher school education lowers the risk of cognitive deterioration. School years can be considered a protective factor (Figures 2 & 3). We observed a statistically significant difference in the result when comparing less than five years with more than five years of school years. For those subjects under five years of education, the test has a lower score (Figure 4).
Table 5:School years influence the MMSE and MoCA score with a P=0.0001.

Discussion
The Spanish version of MoCa (MoCA-S) has higher probability of detecting subjects with mild cognitive disorder compared to MMSE. However, this must be corroborated with neurological and neuropsychological assessment in a population with cognitively healthy subjects. Until 2013 no MoCA-S validations had been conducted in the Spanish-speaking countries of Latin America. Until that same year in Colombia, it was compared in a population above 60 years old with low education level, reporting that a cut-off point ≥ 23 had a sensitivity of 89% for MCI and Mild Dementia with a specificity of 79.8% with a strong association with the educational level, so our data have to be validated according to our educational level. Because the MoCA-S is designed as a screening test its most important purpose is to identify those people with memory complaints who have cognitive impairment (high sensitivity) and guide them to complete neuropsychological tests and be valued by the neurology service, avoiding expensive tests, optimizing resources and reducing unnecessary costs for the health system. False positives do not have a detrimental impact on the health of the subjects since they would later be ruled out with the followup evaluation. In a multivariate logistic regression analysis, two models were evaluated to know which variables were related to the cognitive impairment diagnosis given by the different tests, for the MoCA test, the most independent years of schooling in which we obtained that to a greater degree than schooling is a protective factor for dementia.
In the execution of MOCA, the educational level has an essential effect as previously established [17-19]. In subjects with a low level the MoCA-S shows a decrease in performance because the scores are correlated with the educational level; adding a point to the final score improves this effect, but the results in a low-level test must be carefully examined. Despite this limitation, the MoCA-S presents a better performance for the detection of MCI and mild Dementia than the MMSE. However, the MMSE is better in the evaluation of Dementia with a specificity of 90 %. Therefore, both tests are complementary.
Conclusion
The results obtained confirm those reported in the literature, being MoCA more useful for the detection of cognitive disorders in early stages, being protective factor schooling in years. The average score was 24 points with a level of schooling of 11.5 years. However, this has to be confirmed according to the criteria established in a patient with preserved cognitive function and a similar educational level, involving neuropsychology, psychiatry, and neurology specialists. According to the data obtained MoCA may be more useful as a screening test in the general population when comparing it with MMSE, although the MMSE is useful in the monitoring of Dementia, in addition to which it is suggested to perform a series of tests instead of an isolated test. Do not forget that the fundamental diagnosis is purely clinical, but there is a battery of diagnostic tests that help us to detect early and timely cognitive disorders, which offers us a full window of opportunity for their intervention, mainly if we determine a treatable cause for the cognitive problem presented by the patient who comes to our office. Our study corroborates that schooling is the most important preventive measure for cognitive deterioration.
References
- Raz N (2001) Ageing and the brain. Encyclopedia of Life Sciences, Nature Publishing Group 1-6.
- Raz N, Gunning DF, Head D, Rodrigue KM, Williamson A, et al. (2004) Aging, sexual dimorphism, and hemispheric asymmetry of the cerebral cortex: Replicability of regional differences in volume. Neurobiology of Aging 25(3) :377-396.
- Goméz L, Estudio N (2010) Rating scale-2 in a spanish population sample over 60 years old (doctoral thesis). Salamanca, Spain.
- Braak H, Braak E (1996) Evolution of the neuropathology of Alzheimer ́s disease. Acta Neurologica Scandinava 165: 3-12.
- Linn RT, Wolf PA, Bachean DI, Knoefel JE, Cobb JL, et al. (1995) The preclinical phase of probable Alzheimer ́s disease. A 13-year prospective study of the Framingham cohort. Arch Neurol 52(5): 485-490.
- Perea MV, Ladera V, Morales F (1999) Predictive value of short tests on the cognitive situation in cranio-encephalic traumatisms. Rev Neurol 29(12): 1099-1103.
- Bermejo PF (2003) Reflections on the screening of neurological diseases. Neurology 18(2): 29-38.
- Blesa R, Pujol M, Aguilar M, Santacruz P, Bertran SI,et al. (2001) Normalisation of cognitive and functional instruments for dementia: Clinical validity of the mini-mental state for spanish communities. Neuropsychologia 39(11): 1150-1157.
- Bischkopf J, Busse A, Angermeyer MC (2002) Mild cognitive impairment-A review of prevalence, incidence and outcome according to current approaches. Acta Psychiatr Scand 106(6): 403-414.
- Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, et al. (2005) The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 53(4): 695-699.
- Angevaren M, Aufdemkampe G, Verhaar HJ, Aleman A, Vanhees L (2008) Physical activity and enhanced fitness to improve cognitive function in older people without known cognitive impairment. Cochrane Database Syst rev (3): 3.
- Lautenschlager NT, Cox K, Cyarto EV (2012) The influence of exercise on brain aging and dementia. Biochim Biophys Acta 1822(3): 474-481.
- Hall KS, Gao S, Unverzaght FW, Hendrie HC (2000) Low education and childhood rural residence. Risk for Alzheimer’s disease in African Americans. Neurology 54(1): 95-99.
- Scarmeas N, Zarahn E, Anderson KE, Habeck CG, Hilton J, et al. (2003) Association of life activities with cerebral blow in Alzheimer disease. Implications for the cognitive reserve hypothesis. Arch Neurol 60(3): 359-365.
- Wilson RS, Mendes CF, Barnes LL, Schneider JA, Bienias JL, et al. (2002) Participation in cognitively stimulating activities and risk of incident Alzheimer disease. JAMA 287(6): 742-748.
- Verghese J, Lipton RB, Katz MJ, Hall CB, Derby CA, et al. (2003) Leisure activities and the risk of dementia in the elderly. N Engl J Med 348(25): 2508-2516.
- Rodríguez M, Sánchez JL (2004) Cognitive reserve and dementia. Annals of Psychology 20: 175-186
- Gómez F, Zunzunegui M, Lord C, Alvarado B, García A (2013) Applicability of the MoCA-S test in populations with little education in Colombia. Int J Geriatr Psychiatry 28(8): 813-820.
- Rosselli D, Ardila A, Pradilla G, Morillo L, Bautista L, et al. (2000) The mini mental state examination as a screening test for the diagnosis of dementia: A colombian population study. Rev Neurol 30(5): 428-432.
© 2019 Leyvaa IR. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






