- Submissions

Full Text
Techniques in Neurosurgery & Neurology
Transvenous Endovascular Embolization of Ruptured AVM, Two Cases Report
Islam E*
Department of Neurology, Egypt
*Corresponding author:Islam E, Department of Neurology, Tanta University, Egypt
Submission: March 22, 2019; Published: April 30, 2019

ISSN 2637-7748 Volume2 Issue2
Abstract
Cerebral arteriovenous malformations (AVMs) are the most common congenital cerebrovascular diseases with high risk of intracranial hemorrhage (2% annually) and mortality (1-1.5%). Currently, there are three directions in the treatment of this disease: endovascular embolization, microsurgical removal, and radio surgical therapy. We present two cases of AVM treated by endovascular transvenous approach.
Introduction
Cerebral arteriovenous malformations (AVMs) are the most common congenital cerebrovascular diseases with high risk of intracranial hemorrhage (2% annually) and mortality (1-1.5%) [1]. Currently, there are three directions in the treatment of this disease: endovascular embolization, microsurgical removal, and radio surgical therapy [2]. Trans arterial N-butyl cyanoacrylate (NBCA)/Onyx embolization, as practiced currently, is performed in most arteriovenous malformations (AVMs) [1].
There are those AVMs not amenable to trans arterial embolization, usually because of the distal location of the nidus, the small size of the arterial pedicles, or the involvement of associated branches to the adjacent normal brain. Transvenous embolization was designed as an alternative to conventional trans arterial embolization in cases when the latter is possible, while macro surgery and radiosurgery are associated with high risk [2]. The following is our first experience with this technique in the treatment of a complex deep arteriovenous malformation.
Case No 1
History and clinical examination at presentation
A 23 years old female without medical history presented with sudden onset of headache, vomiting with noticed difficulty to move right side of the body. By examination the patient has: neck rigidity, right sided spastic weakness (grade 2) and left sided ataxia; mRS 4. Noncontrast CT brain was done and showed hematoma in the left lateral wall of pons and midbrain; extending to the 4th, 3rd and both anterior horns of lateral ventricles. CT angiography showed cisternal AVM drained by enlarged deep vein (mostly the left basal vein of Rosenthal). MRI brain showed cisternal hematoma (ambient and quadrigeminal) elevating the tentorium (Figure 1).
Diagnostic angiogram was done and showed a cisternal AVM that has the following angioarchitecture criteria:
A. Nidal size: 3,5cmx2.4cm with 2 initial venous compartments.
B. Arterial feeder: multiple large pontine perforators arising from the most proximal long circumferential branch and many short circumferential branches.
C. Draining veins: Two venous tributaries draining into the left basal vein of Rosenthal; the most tortuous is the lateral mesencephalic vein (Figure 2).
Endovascular treatment
Trans-arterial endovascular embolization was impossible as the feeders of the AVM were pontine perforators that carried a very high risk; so, a transvenous approach was decided.
The right Internal Jugular vein was punctured and the diagnostic catheter, 5f vertebral was navigated over term 0,035 wire to the sigmoid sinus, transverse sinus, confluence, straight sinus and then to the enlarged vein of Galen. Detachable tip micro catheter Sonic® 1.2F was navigated over a Hybrid 0,008 microwire till it reached the straightest one of the two draining veins; a super selective venography of the drainage vein delineated precisely its nidal compartment.
Figure 1:O(A) CT brain and CT angiography showing hematoma in the left lateral pons and midbrain extending to the 4th, 3rd and anterior horns of lateral ventricles as a result of ruptured cisternal AVM that is drained by enlarged deep vein. (B) MRI brain showed hematoma in the ambient and quadrigeminal cisterns; elevating the tentorium cerebelli.
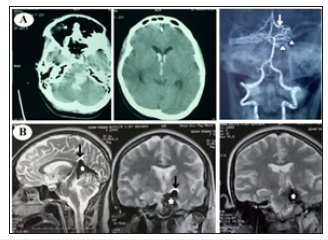
Figure 2:Diagnostic angiography: AP left vertebral arteriogram. (A) Arterial phase: showing multiple pontine perforators feeding the AVM; arising mainly from the most proximal long circumflex branch. (B) Early venous phase: showing two draining veins; the most tortuous of them is the lateral mesencephalic vein. Both of them are drained by the left basal vein of Rosenthal.
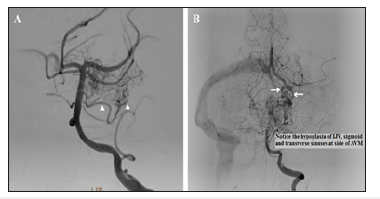
Figure 3:(A) Lateral (B) Oblique views of a super selective venography delineating the targeted nidal compartment of the AVM. (C&D) Lateral and oblique non-subtracted images “the same as in A&B” after final Onyx injection. The targeted compartment was totally occluded, with extension of Onyx toward small part of another compartment
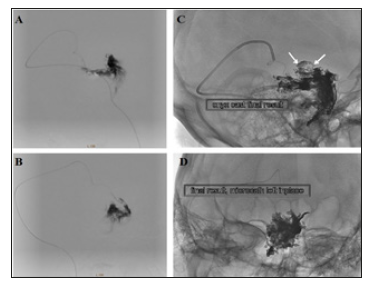
Injection of Onyx® 18 was started by making a plug to occlude the vein to allow progress of Onyx into the nidus. The Onyx partially diffused also toward the other compartment. Finally, a sufficient occlusion of the nidus is reached. The other draining vein is left to act as a safety valve and drains the remaining part of the nidus (Figure 3).
To avoid the risk of venous rupture during pulling on the micro catheter, it was cut at the neck after applying some traction and left in situ. After recovery from anaesthesia, the patient had difficulty in mastication due to weakness of left masseter and pterygoids with facial pain (trigeminal nerve affection) mostly from basilar perforators ischemic insult, MRI with diffusion was done but the ischemic insult couldn’t be seen because of Onyx artifact
Follow-up
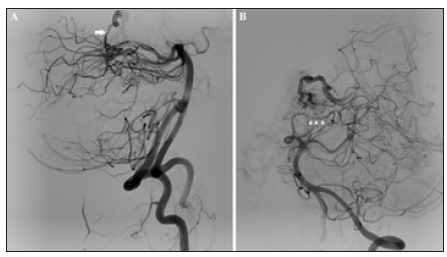
Follow-up control angiogram was done after 3 months that showed increasing nidal occlusion (about 90% closure). Also, the clinical status of the patient was improved, motor power improved (mRS 2) and total improvement of trigeminal nerve affection. showed the patient was advised to see gamma knife consultation (Figure 4)
Figure 4:Follow-up after 3 months of right vertebral angiogram in case No.7 (A) Oblique (B) Lateral views showing incomplete closure of the AVM nidus and the patient was advised to consult gamma knife for the remaining nidus.

Case No.2
History and clinical examination at presentation
A 33 years old male without a medical history presented with sudden onset of severe agonizing occipital headache, followed by nausea, vomiting and blurring of vision. By examination, the patient was conscious, with neck rigidity and bilateral grade-I papilledema mRS 1. Non-contrast CT brain was done and showed right occipital horn hematoma with extension to the 3rd ventricle and both anterior horns. CT angiography shows small AVM in the right occipital region (Figure 5).
Figure 5:(A) CT brain shows R.t occipital horn hematoma extending to body of R.t lateral ventricular body, both anterior horns of lateral ventricle and third ventricle. (B) CT angiography shows small AVM in the R.t occipital horn.

When the patient′s mRS became 0, diagnostic catheter was done and showed small AVM that had the following angioarchitecture criteria:
∎ Nidus: small triangular compact nidus (about 1cm).
∎ Arterial feeder: en passage feeding by right parietooccipital branch of PCA (P4).
∎ Draining vein: Dilated right medial atrial vein, one of tributaries of the ICV (stenosis distal to the foot of draining vein is noticed that increases the risk of hemorrhage) (Figure 6).
Figure 6:(A) Lateral view of right vertebral angiogram showing a small triangular compact nidus drained by right medial atrial vein (a tributary of right ICV). (B) Oblique views of left vertebral angiogram showing that the nidus has an en-passage feeding by right P4 part of PCA.
Super selective injection of the right parieto-occipital branch of PCA was done, showed that the feeder was end passage, so transvenous approach was decided.
Endovascular treatment
The right Internal Jugular vein was punctured and Chaperon 6f guiding catheter was navigated over terumo 0,035 wire was navigated to the sigmoid sinus, transverse sinus, Eclipse® double lumen -micro catheter was navigated over a Hybrid 0,008 micro wire till the foot of right medial atrial vein (Figure 7).
Pressure cooker technique
Careful inflation of the balloon proximal to the slowly injected Onyx 18 was done to make the Onyx diffuse toward the nidus and prevents its reflux toward the right Internal cerebral vein. The injection of onyx was stopped when complete occlusion of the nidus, draining vein and the distal feeder (Figure 8).
Figure 7:Transvenous approach toward the nidus. (A) Road-map showing the navigation of the J-tip microwire) through the straight sinus, vein of Galen, right Internal cerebral vein and its medial atrial vein. (B) Non-subtracted image showing the 3 markers of the double lumen balloon-microcatheter.
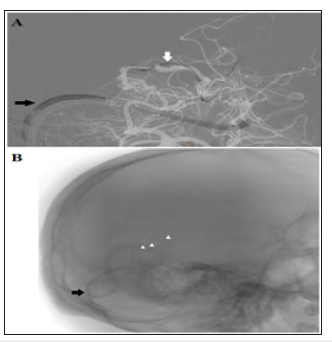
Figure 8:Onyx injection by pressure cooker technique. (A) Begin of reflux of the Onyx in the draining vein. (B) After inflation of the balloon Onyx is pushed toward the nidus. (C&D) Onyx is still pushed to fill the nidus. (E) Onyx reaches the arterial side. (F) Onyx obliterates the foot of the draining vein and the nidus completely and no longer seen.
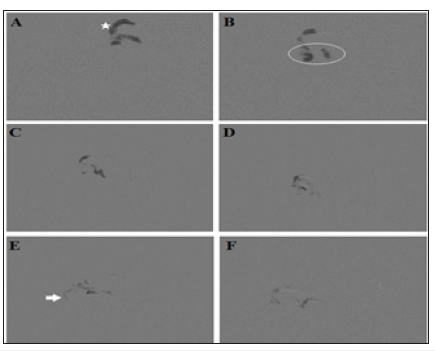
Figure 9:Follow-up AP (A) Lateral (B) Views of vertebrobasilar system showing complete curative occlusion of the AVM.
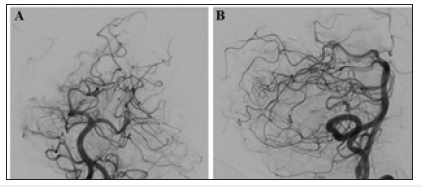
Follow-up
Follow-up diagnostic catheter was done 3 months later and shows complete curative occlusion of the nidus. The mRS of the patient is now zero (Figure 9).
The 2 cases had been approved by our institutional research and quality committee.
Discussion
The first mention of the use of venous approach for AVM embolization refers to 1999 and belongs to Massoud T & Hademenos G [3]. They used transvenous approach for embolization of malformation models in pigs under controlled hypotension. In 2010, Nguyen T et al. [4] published the results of their first successful transvenous embolization of ruptured malformations in a human. A year later, Kessler I et al. [5] presented a series of five cases. In 2013, Pereira et al. [6] used a balloon catheter in the transvenous embolization for temporary occlusion of malformation afferents. This allowed both preventing non-target embolization of the main vessels and reducing the blood flow through the AVM, facilitating penetration of adhesive composition into the node.
The first case reported in this paper is our first experience of the use of transvenous access to malformation. Given a history of hemorrhage from the AVM in this patient, there was a significant risk of re-rupture, which is an absolute indication for treatment. During the initial planning of its tactics, direct surgical intervention was obviously impossible due to AVM location. Radiosurgery was also considered to be unsuitable due to the large total size of malformation nodes (which exceeded the limit of this method of 3cm) and high risk of damage to functionally important brain structures. Thus, endovascular technique was the method of choice in this patient.
In view of the fact that malformation filled through thin perforators of the terminal part of the Basilar artery, trans arterial catheterization proved to be technically impossible, since the diameter of these afferents was below the minimum diameter of the catheter. However, the features of AVM angioarchitecture (smallsized malformation and draining through two separate veins) enabled transvenous embolization with less risk to the patient. The use of navigation of the diagnostic catheter very distal up to the vein of Galen, helped to achieve stable position of the microcatheter for safer and more efficient catheterization of the malformation draining vein.
The second case reported in this paper showed ruptured small AVM with small feeder from end passage artery, drained by single vein from the deep system, trans arterial embolization was carrying the risk of occlusion of the feeder ,while transvenous embolization had the chance of occlusion of foot of the draining vein, nidus and the small branches from the end passage artery without the risk of occlusion of the parieto occipital branch of posterior cerebral artery, using the double lumen micro catheter with injection of Onyx during inflation of the balloon enabled the Onyx to diffuse to the nidus without marked reflux to the large calibre draining vein and ultimately to the Internal cerebral vein, careful very slow inflation of the balloon was important to avoid rupture of the draining vein, successful obliteration of the AVM with small amount of Onyx 0,7ml with minimal reflux was achieved using the pressure cooker technique done by double lumen DMSO compatible micro catheter.
Summary
Transvenous embolization can be used in AVM treatment. Indications for use include small size of malformation node, single draining vein, difficult catheterization of afferents of the malformation (small diameter and significant tortuosity) as in the first case supplied from basilar perforators ,the high risk with surgery and radiosurgery, trans arterial perforators navigation made transvenous treatment is the only option, the outcome was occlusion of one compartment of AVM ,decreasing its size for radiosurgery, in the second case AVM supplied by artery end passage with high risk of reflux ,the draining vein was large and near to the straight sinus that is why pressure cooker technique using double lumen balloon was used which is rarely used, good outcome was achieved with total occlusion of AVM leaving both the feeder and the great cerebral vein of Galen patent.
References
- Maryashev SA, Golanov A V, Konovalov AN, Yakovlev SB, Il’yalov SR, et al. (2013) Radio surgical treatment of patients with arteriovenous malformations of the brain using (Gamma Knife) instrument. Voprosy neirokhirurgii 5: 16-29.
- Lv X, Wu Z, Li Y (2013) Arteriovenous malformation in the brain: A theoretical study explaining the behavior of liquid embolic agents during endovascular treatment. Neuroradiol J 26(6): 661-668.
- Massoud TF (2013) Transvenous retrograde nidus sclerotherapy under controlled hypotension (TRENSH): Hemodynamic analysis and concept validation in a pig arteriovenous malformation model. Neurosurgery 73(2): 332-342.
- Nguyen TN, Chin LS, Souza R, Norbash AM (2010) Transvenous embolization of a ruptured cerebral arteriovenous malformation with en passage arterial supply: initial case report. J Neurointerv Surg 2(2):150-152.
- Kessler I, Riva R, Ruggiero M, Manisor M, Khawaldeh MA, et al. (2011) Successful transvenous embolization of brain arteriovenous malformations using Onyx in five consecutive patients. Neurosurgery 69(1): 184-193.
- Pereira VM, Marcos GA, Radovanovic I, Bijlenga P, Narata AP, et al. (2013) Transvenous embolization of a ruptured deep cerebral arteriovenous malformation. A technical note. Interv Neuroradiol 19(1): 27-34.
© 2019 Islam E. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






