- Submissions

Full Text
Techniques in Neurosurgery & Neurology
Decompressive Craniectomy: A Review of the Adequacy of the Bony Decompression in a Single Institution
Haitham Ben Ali*, Hassan Othman, Andrew Jones and Paul Leach
Consultant Neurosurgeon, UK
*Corresponding author: Haitham Ben Ali, Consultant Neurosurgeon, UK
Submission: October 03, 2018;Published: November 26, 2018
ISSN 2637-7748
Volume2 Issue2
Abstract
Background: Decompressive craniectomy (DC) is a surgical procedure to remove part of the skull to accommodate brain swelling and hence control intracranial hypertension. We aimed in this study to retrospectively review the adequacy of the bony decompression for all decompressive craniectomies performed in our unit.
Method: This audit approved by the clinical audit department in the university hospital of Wales. Retrospective data collected for all patients identified as primary or secondary decompressive craniectomy between January 2011 and March 2014 within our institution.
Results: The total number of patients recruited was 33, the indications for surgery were traumatic brain injury 49% (n=16), subarachnoid haemorrhage 27% (n=9), stroke 15% (n=5) and intracerebral haemorrhage 9% (n=3). The vertical decompression was achieved in 57% (n=17) and the horizontal decompression achieved in 83% (n=25). While temporal bone removal was only achieved in 33% (n=11). An adequate bifrontal decompression was not achieved in any patient. The overall adequate decompression was achieved in 21% (n=7).
Conclusion: We achieved middle fossa decompression only in 33% of the cases and overall adequate decompression achieved only in 21% of the cases. We concluded that more focused training is needed. This work has been presented at our departmental audit meeting and we aim to prospectively repeat this audit and establish if our decompressions have subsequently improved. And we will also be looking at the clinical outcomes of our patients in relation to their decompression.
Keywords: Decompressive craniectomy; Traumatic brain injury; Intracerebral haemorrhage; Subarachnoid haemorrhage; Bifrontal craniectomy
Introduction
Decompressive craniectomy (DC) is a surgical procedure to remove part of the skull to accommodate brain swelling and hence control intracranial hypertension. Trephination was performed as early as 10,000BC, but Hippocrates in his book “injury of the head”, written around 400BC, was the first to systematically describe skull fractures and discuss which types of injury should be treated with trephination. He also recognized that trephination could treat visual loss, perhaps due to raised ICP [1,2].
Theodor Kocher in 1901 stated that: “if there is no cerebrospinal fluid (CSF) pressure, but brain pressure exists, then pressure relief must be achieved by opening the skull”. Following that in 1908 Harvey Cushing, who worked earlier in the lab of Theodor Kocher, presented a case series of patients with head injuries, specifically skull fracture, who were treated with sub-temporal DC. Cushing reported a surgery-associated reduction in mortality from 50% to less than 15% (2 out of 15 patients), and he asserted that the brain oedema and swelling that accompany severe cerebral contusions were best managed with a sub-temporal DC [3].
There are two types of decompressive craniectomy, bifrontal and unilateral (hemicraniectomy). The bifrontal DC extends from the floor of the anterior cranial fossa inferiorly to the coronal suture posteriorly and to the pterion laterally. This type of DC is usually performed in patients with diffuse brain swelling [4,5]. However, a unilateral DC is usually performed in cases with predominantly unilateral hemispheric swelling and/or intracranial haematoma. This involves the fronto–temporo-parietal bone [5,6], with the minimum diameter of 11-12 centimetres [7-10].
The DC could be primary when the decompression is performed at the time of evacuation of a haematoma, or secondary when the decompression performed for intracranial hypertension refractory to medical treatment.
Methods and Material
Patients were retrospectively identified from our emergency and elective theatre logbooks. We searched for all patients entered as undergoing either craniotomy or craniectomy between January 2011 and March 2014. The patients case notes and operation notes were reviewed to identify all the patients whom underwent a primary or secondary DC. The post-operative images of all these patients were reviewed with regards to the adequacy of their decompression. Patients, who had bone removal performed without the aim of decompression (e.g. infected bone flap) or had the removal of a bone flap that had been tailored in previous craniotomy and operated for the 2nd time for removal of the bone flap, were excluded. The adequacy of the decompression identified using the horizontal diameter (anterior to posterior) (Figure 1), the vertical diameter (superior to inferior) (Figure 2) and the temporal fossa decompression (Figure 3).
Figure 1:Horizontal diameter (anterior to posterior).

Figure 2:Vertical diameter (superior to inferior).
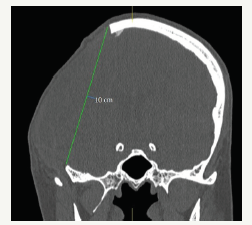
Figure 3:Temporal fossa decompression.

Results
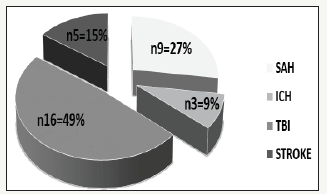
The total number of patients recruited was 33. The median age was 39 years (range 15-70 years) and the female to male ratio was 1:2 (F=11, M=22) (Figure 4). The indications of surgery were traumatic brain injury in 49% (n=16), subarachnoid haemorrhage in 27% (n=9), stroke in 15% (n=5) and intracerebral haemorrhage in 9% (n=3) (Figure 5).
Figure 4:Gender distribution.
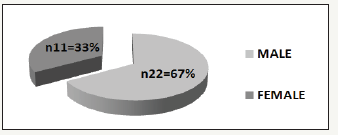
Figure 5:The distribution of the cases underwent decompressive craniectomy. (SAH = Subarachnoid haemorrhage, ICH = Intracerebral haemorrhage, TBI = Traumatic brain injury).
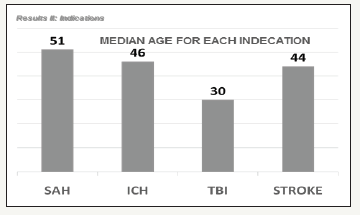
The median age based on indication showed that the traumatic brain injury group represented the youngest with the median age of 30 years (range 15-63 years) (Figure 6). The median age was higher in the other groups; stroke= 44 years (range 37-63 years), ICH = 46 years (range 38-70 years) and SAH = 51 years (range 38-70 years).
Figure 6:The median age for each category. (SAH = Subarachnoid haemorrhage, ICH = Intracerebral haemorrhage, TBI = Traumatic brain injury).
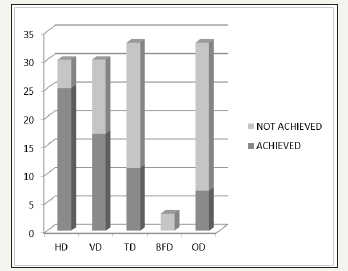
Primary decompression was performed in 52% of the patients and was secondary in 48% (n=17 and n=16 respectively). The side of surgery was found to be on the right side in 55% (n=18), which included the entire stroke group and on the left side in 36% (n=36). Bifrontal decompression occurred in 9% (n=3) and were all from the head injury group. The vertical decompression was adequately achieved in 57% (n=17) and the horizontal decompression in 83% (n=25). The temporal bone was removed only in 33% (n=11). The bifrontal decompression was not adequately achieved in any patient. The overall adequate decompression was achieved in only 21% (n=7) (Figure 7). The dura was opened in all cases and augmented either by dura substitute or pericranium. And most of the operations were performed by the on-call middle grade neurosurgical trainee in various levels of training.
Figure 7:Adequacy of decompression, HD (horizontal diameter), VD (vertical diameter), TD (temporal decompression), BFD (bifrontal decompression), OD (over all decompression).
Discussion
There is strong evidence to suggest that the DC can be used to reduce the ICP [7], however the exact indication and timing for DC remain unclear [7] In this regard, extensive work on DC has been performed mainly on head injury with no clear evidence that DC is superior to medical management [4,5,8,11]. However, The DECRA trial, which aimed to assess early DC with the trigger being an ICP>20 mmHg for 15minute within one hour, found that DC leads to shorter duration of mechanical ventilation and ITU stay in compression to medical management [7]. The RESCUEicp trial is published recently after conducting our audit, and it aimed to assess the effectiveness of DC offered as last tier treatment in TBI with ICP>25 mmHg for 1-12 hour despite the maximum medical management. They found; using the extended Glasgow outcome score; that DC lowered mortality but caused higher rates of vegetative state, lower sever disability and upper sever disability than medical care, the rates of moderate disability and good recovery were similar in the two groups [12]. Similarly, DC in stroke patients did improve overall survival, but increased the proportion of individuals with moderately severe or severe disability [13,14]. A new ongoing trial is the RESCUE-ASDH with the hypothesis that primary DC may be more effective than craniotomy for patients undergoing evacuation of an acute subdural haematoma [15].
The evidence supporting other indications for DC is limited and obtained from uncontrolled case series and case reports, e.g. aneurysmal subarachnoid haemorrhage (SAH), spontaneous intracerebral haemorrhage (ICH), viral and bacterial encephalitis, acute disseminated encephalomyelitis (ADEM) and cerebral venous and sinus thrombosis [7].
When decompressive surgery is considered, there is some controversy in the selection between the two types of DC. However, there is no controversy about the extent of the bony decompression. The bifrontal DC extends from the floor of the anterior cranial fossa inferiorly to the coronal suture posteriorly and to the pterion laterally. This type of DC is usually performed in patients with diffuse brain swelling [4,5]. On the other hand, a unilateral DC is usually performed in cases with predominantly unilateral hemispheric swelling or intracranial haematoma (usually SDH), and it involves the fronto-temporo-parietal bone [4,6], with the minimum diameter of 11-12 centimetres [7-10]. If the bone flap is too small, the swollen brain can herniate through the craniectomy window, with resultant compression of the bridging veins and venous infarction [10,11] this can lead to further brain injury, a further rise in ICP and poorer outcome [16]. It is important to remove the inferior part of the temporal bone, to the floor of the middle cranial fossa, in both types of DC.
We aimed to study the adequacy of bony decompression in our patients. As the published literature showed better outcomes in patients undergoing the accepted standard craniectomy and worse outcomes when a small craniectomy is performed [17]. We did not look at clinical outcome in this study, however it will be the subject for further research within our department.
Conclusion
In our series, we achieved middle fossa decompression in only 33% of the cases and overall adequate decompression was achieved in 21%. This study has been presented at our unit Neuroscience audit meeting, and we concluded that more focused training is needed. We plan to repeat this audit prospectively in the future to show an improved decompression for our patients undergoing DC, and we will also be looking at the clinical outcomes of our patients in relation to their decompression.
Funding
No funding was received for this research
Conflict of Interest
All authors certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patentlicensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- Kolias AG, Kirkpatrick PJ, Hutchinson PJ (2013) Decompressive craniectomy: past, present and future. Nat Rev Neurol 9(7): 405-415.
- Symeon Missios MD (2007) Hippocrates, galen and the uses of trepanation in the ancient classical world. Neurosurg focus 23(1): E11.
- Cushing H (1908) Sub-temporal decompressive operations for the intracranial complications associated with bursting fractures of the skull. Ann Surg 47(5): 641-644.
- Hutchinson P, Timofeev I, Kirkpatrick P (2007) Surgery for brain edema. Neurosurg Focus 22(5): E14.
- Polin RS, Shaffrey ME, Bogaev CA (1997) Decompressive bifrontal craniectomy in the treatment of severe refractory posttraumatic cerebral edema. Neurosurgery 41(1): 84-92.
- Timofeev I, Santarius T, Kolias AG, Hutchinson PJ (2012) Decompressive craniectomy-operative technique and perioperative care. Adv Tech Stand Neurosurg 38: 115-136.
- Cooper DJ, Rosenfeld JV, Murray L (2011) Decompressive craniectomy in diffuse traumatic brain injury. New Engl J Med 364(16): 1493-1502.
- Li LM, Kolias AG, Guilfoyle MR (2012) Outcome following evacuation of acute subdural haematomas: a comparison of craniotomy with decompressive craniectomy. Acta Neurochir 154(9): 1555-1561.
- Tagliaferri F, Zani G, Iaccarino C, Ferro S, Ridolfi L, Basaglia N (2012) Decompressive craniectomies, facts and fiction: a retrospective analysis of 526 cases. Acta Neurochir 154(5): 919-926.
- Wagner S, Schnippering H, Aschoff A, Koziol JA, Schwab S, et al. (2001) Suboptimum hemicraniectomy as a cause of additional cerebral lesions in patients with malignant infarction of the middle cerebral artery. J Neurosurg 94(5): 693-696.
- Stiver SI (2009) Complications of decompressive craniectomy for traumatic brain injury. Neurosurg Focus 26(6): E7.
- Hutchinson PJ, Wilson HM, Critchley G (2016) Trial of decompressive craniectomy for traumatic intracranial hypertension. New Engl J Med 375(12): 1119-1130.
- Cruz-Flores S, Berge E, Whittle IR (2012) Surgical decompression for cerebral oedema in acute ischaemic stroke. Cochrane Database Syst Rev 1: CD003435.
- Jauch EC, Saver JL, Adams HP (2013) Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 44(3): 870-947.
- Kolias AG, Scotton WJ, Belli UK (2013) Surgical management of acute subdural haematomas: current practice patterns in the United Kingdom and the Republic of Ireland. Brit J Neurosurg 27(3): 330-333
- Jiang JY, Xu W, Li WP (2005) Efficacy of standard trauma craniectomy for refractory intracranial hypertension with severe traumatic brain injury: a multicenter, prospective, randomized controlled study. J Neurotraum 22(6): 623-628.
- Torres R (2012) DECRA, Where do we go from here?. Surg Neurol Int 3: 54.
© 2018 Haitham Ben Ali. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






