- Submissions

Full Text
Techniques in Neurosurgery & Neurology
Multisensory Environments and the Patient with Alzheimer’s Disease: An Evidence-based Review
Hassan Izzeddin Sarsak*
Department of Occupational Therapy, University of Jordan, Jordan
*Corresponding author:Hassan Izzeddin Sarsak (PhD, OT), Department of Occupational Therapy, School of Rehabilitation Sciences, Batterjee Medical College, Jeddah, KSA, Saudi Arabia
Submission: October 11, 2018;Published: October 26, 2018

ISSN 2637-7748
Volume2 Issue2
Abstract
Background: Effects of environment on behavior have been studied. Manipulations of environmental sensory stimulation and environmental modifications have been used to enhance functional performance for patients with dementia.
Objectives:< this study was conducted to examine and review the evidence available regarding the effectiveness of environmental modifications and multisensory stimulation on functional performance and ability to engage in activities of daily living (ADLs) for patients with dementia.
Results: our review revealed that environmental modifications and multisensory stimulation for patients with dementia can improve functional performance and may increase engagement in meaningful ADLs.
Conclusion: environmental modifications and multisensory stimulation are effective and can improve functional performance and increase engagement in meaningful ADLs for patients with dementia.
Keywords: Multisensory; Environment; Modification; Behavior; Functional performance and engagement; Activities of daily living (ADLs); Dementia alzheimer type (DAT); Occupational therapy (OT)
Introduction
Dementia is a group of disturbances of memory associated with multiple cognitive deficits, such as aphasia, apraxia, agnosia, and disturbance of executive function. Alzheimer’s is the most common type of dementia (Dementia Alzheimer Type; DAT). The signs of dementia generally include, but are not limited to, decreased short term memory, decreased problem solving skills, decreased perceptual skills, and personality changes. The onset of dementia is gradual, and the course of the disease spans several years or more. In Alzheimer’s disease, the person progresses through several stages with those in the final stages being completely dependent on others. Cognitive losses in DAT can lead to inability to process stimuli accurately [1]. Occupational therapists (OTs) evaluate persons with dementia to determine their strengths, impairments, and performance areas needing intervention. Although remediation of cognitive performance is not likely, the person may demonstrate improved function through compensation or adaptation. Occupational therapy (OT) practitioners also assist caregivers to help them cope with difficulties associated with dementia to ensure safe and supportive environment. Effects of environment on behavior have been widely studied. Effects of environment can be neutral, facilitative, or restrictive. Manipulation of environmental sensory stimulation has been used since the 1960s to promote increased function with patients with dementia [2]. The purpose of this study was to examine the evidence available regarding the effectiveness of environmental and sensory modifications on functional performance and ability to engage in meaningful activities of daily living (ADLs) for patients and older adults with dementia. For the purpose of this study, we created a clinical/ research PICO question (Population, Intervention, Comparison, and Outcome), a key to evidence-based decision [3]. The PICO formed for our study is as follows:
(P) In patients with dementia
(I) Does environmental/sensory modification
(C) Compared to no environmental/sensory modification
(O) Increase/improve/result in ability to engage in activities?
Methods
Review of literature and search strategy
A research has been made in the following databases: Ovid (MEDLINE, PsychINFO, and Global Health), and PubMed. Keywords and Search items used to search articles for our study were multisensory, environment, modification, behavior, functional performance and engagement, activities of daily living (ADLs), dementia Alzheimer type (DAT), and occupational therapy (OT).
Results
By combining the search results we found articles on Tai Chi that discuss the relationship between Tai Chi and fear of falling among older adults. Based on the format of PICO question, four most relevant articles were selected for our study. Studies cited in the reference of the four articles along with other articles were also used to collect important information. The four selected articles were related to the effect of environmental modifications and multisensory stimulation on functional performance and engagement in ADLs for patients with dementia.
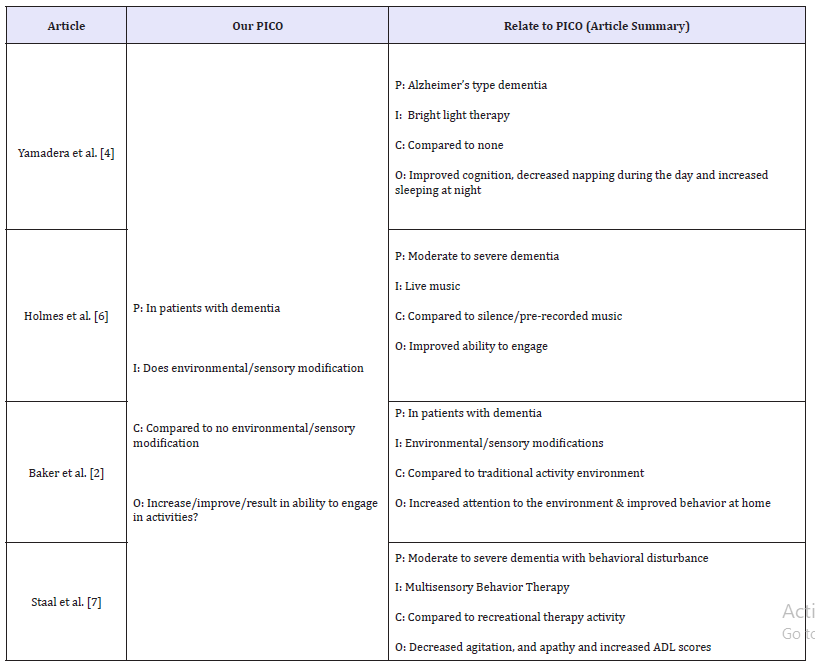
Yamadera et al. [4] examined the effect of bright light therapy on sleep/wake cycles. Based on the hierarchy of levels of evidence in evidence based practice, this study was a level III pre- postcomparison of cohort/ diagnostic groups [5]. This study measured level of dementia, cognition, number of naps and nap time during the day, sleep time and number of awakenings at night. Holmes et al. [6], studied the effect of live music versus pre-recorded music versus silence on apathy. Subjects had moderate to severe dementia with apathy. This was a level III, randomized placebo controlled trial with blinded observer rating. In this study, they used the Dementia Care Mapping tool median scores to measure engagement. Also they measured the percentage of subjects showing positive engagement. In Baker et al. [2], they investigated the effects of Multi-Sensory Stimulation (MSS) on behavior, mood, and cognition. This was a level II, randomized control. They used MSS as treatment group and activity intervention as control group. Multiple time points, including baseline, before, during, after each session, after 4 sessions, after 8 sessions and then one month after the last session were conducted. In Staal et al. [7], they studied the effects of Multisensory Behavior Therapy (MBST) on agitation, apathy, and ADL performance. It was a level II, randomized attention controlled single blinded study. Multiple time points were applied at baseline, and after each of 6 treatment sessions. All articles were related to our PICO question. A summary of the four articles in relation to our PICO is as follows (Table 1).
Table 1:A summary of Reviewed Articles in Relation to our PICO.
Discussion
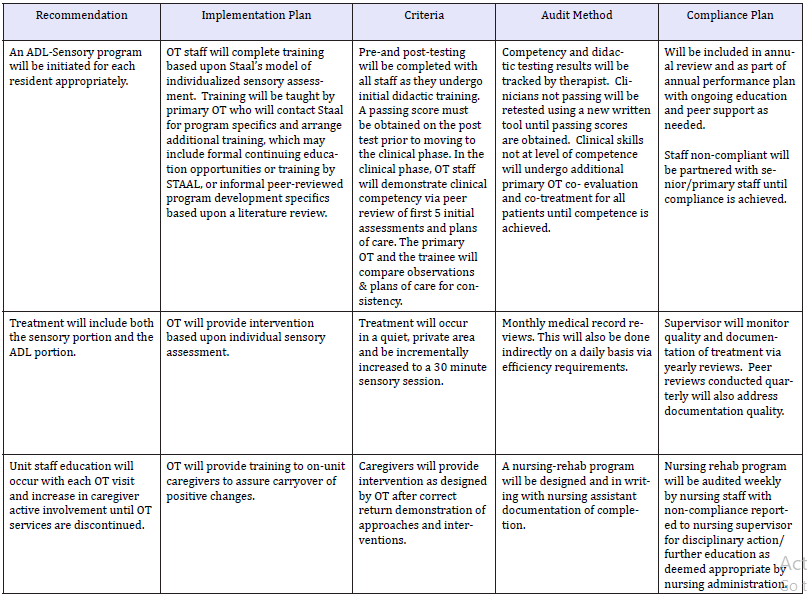
In all reviewed studies, environmental modifications and multisensory stimulation for patients with dementia improved functional performance, enhanced cognition and attention, and increased engagement in ADLs. Thus clinical guidelines, recommendations, a plan and audit tool have been developed in our study to implement environmental modifications and multisensory stimulation in clinics (Table 2).
Table 2:A summary of Recommendations, Plan, and Audit Tool
Conclusion
Our review confirmed that environmental modifications and multisensory stimulation are effective and can improve functional performance and increase engagement in meaningful ADLs for patients with dementia. Thus clinical guidelines, recommendations, a plan and audit tool have been created in our study to implement environmental modifications and multisensory stimulation in clinics. The clinical guidelines for recommended intervention, the plan, and the audit tool recommend therapists (i.e., OT) to apply environmental modifications and multisensory stimulation with patients and older adults with dementia.
Conflict of Interest
Author declares that there is no conflict of interest.
References
- American Psychiatric Association (2002) Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC, American Psychiatric Association, USA.
- Baker R, Bell S, Baker E, Gibson S, Holloway J, et al. (2001) A randomized controlled trial of the effects of the multi- sensory stimulation (MSS) for people with dementia. British Journal of Clinical Psychology 40(Pt 1): 81-96.
- Richardson WS, Wilson MC, Nishikawa J, Hayward RS (1995) The wellbuilt clinical question: A key to evidence-based decision. ACP Journal Club 123(3): A12-3.
- Yamadera H, Takao I, Hideaki S, Kentaro A, Ritsuko I, et al. (2000) Effects of bright light on cognitive and sleep-wake (circadian rhythm) disturbances in Alzheimer-type dementia. Psychiatry and Clinical Neurosciences 54(3): 352-353.
- Hughes I (2006) Action research in healthcare: what is the evidence? ALAR Journal 11(1): 29-39.
- Holmes C, Knights A, Dean C, Hodkinson S, Hopkins V (2006) Keep music live: Music and the alleviation of apathy in dementia subjects. International Psychogeriatrics 18: 623-630.
- Staal J, Sacks A, Mathies R, Coller L, Calia T, et al. (2007) The effects of Snoezelen (Multisensory Behavior Therapy) and psychiatric are on agitation, apathy, and activities of daily living in dementia patients on a short term geriatric psychiatric inpatient unit. International Journal of Psychiatry in Medicine 37(4): 357-370.
© 2018 Hassan Izzeddin Sarsak. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






