- Submissions

Full Text
Techniques in Neurosurgery & Neurology
A Different Approach to Papillae Edema: CaseReport
Gamze Maden1*, Şeyma Gülcenur Özturan1, Akın Çakır1, Mehmet Egemen Karataş2, Mustafa Nuri Elçioğlu1
1 Department of Ophthalmology, Okmeydani Training and Research Hospital, Turkey
2 Department of Ophthalmology, Sisli Hamidiye Etfal Training and Research Hospital, Turkey
*Corresponding author: Gamze Maden, Department of Ophthalmology, Okmeydani Training and Research Hospital, İstanbul,Turkey
Submission: March 25, 2018;Published: May 14, 2018

ISSN 2637-7748
Volume1 Issue4
Abstract
Papillae edema is not a disease by itself, but it is a finding which can be seen with various diseases. Ocular, orbital, intracranial and systemic diseases can cause papillae edema. For this reason, a good differential diagnosis should be determined and the treatment should be applied accordingly. A Vogt Koyanagi Harada patient was presented to emphasize the awareness of eye diseases with neurological findings.
keywords Vogt Koyanagi Harada; Corticosteroids; Papillae edema; Pseudotumor cerebri
Introduction
Optic disc edema is defined as ophthalmologic swelling of the optic nerve [1,2]. For differential diagnosis of optic disc edema, the age of the patient, the presence of systemic disease, the onset of complaints, the unilateral or bilateral occurrence of optic disc edema, decreasing of visual acuity is very important. A multidisciplinary approach is required for the patients who have a papillae edema because there can be ocular, orbital, intrcranial and systemic reasons.
Case Presentation
Figure 1: Pre-treatment: Right Eye OCT.
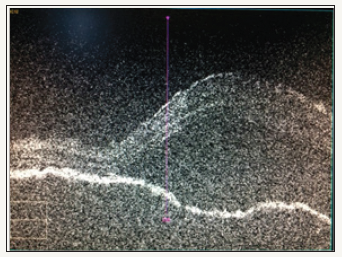
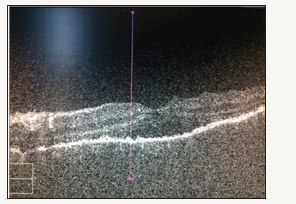
A 60-year-old male patient was admitted to the emergency room with complaints of headache and blurred vision in both eyes for 3 days. The visual acuity at the arrival of the patient is bilaterally 0.1 (Snellen equivalent). Anterior segment examination; natural on the right eye, posterior synechia on the left eye at 7 o’clock. Intraocular pressure (IOP) was bilaterally 16 mmHg. Bilateral optic disc edema was observed on fundus examination. The patient was admitted to the neurology clinic with a preliminary diagnosis of pseudotumor cerebri, and advanced examination purpose. Neurological imaging methods, multiple lumbar punctures and visual fields tests were completed in the clinic of neurology and neurological pathology which could explain the picture was not detected. The patient was re-consulted to the ophthalmology clinic for interpreting the patient’s visual field. Bilateral ‘clover leaf’ finding was observed in the visual field test of the patient, and the patient’s eye examination was repeated, which was not compatible with neurological diagnosis. The bilateral visual acuity of the patient was fingercounting from 2 meters. Anterior segment examination; natural on the right eye, posterior synechia at 7 o’clock on the left eye. IOP bilaterally was 14 mmHg. Bilateral optic disc edema and numerous serous detachments in the posterior pole and peripheral retina were observed. Bilateral diffuse choroidal thickening and serious detachments were seen in optic coherent tomography (OCT). Vogt- Koyanagi-Harada (VKH) syndrome was considered. Systemic steroid therapy (pulse 1 gram/day methylprednisolone) was initiated and after three days the patient’s visual acuity was increased to bilaterally 0.5, anterior segment examination; natural on the right, natural on the left except posterior synechia at 7 o’clock. Bilateral optic disc edema persisted on fundus examination, but serous detachments’s regression was seen and treatment was continued with reducing systemic steroid (intravenous 250 milligram (mg) methylprednisolone). After three days, the patient’s visual acuity was bilaterally 0.7. The anterior segment findings were the same, while bilateral optic disc edema persisted at the fundus, serous detachments were further reduced. The patient was discharged with oral systemic steroid (64 mg oral methylprednisolone). The patient was directed to our uvea department for follow-up (Figures 1-4).
Figure 2: Pre-treatment: Left Eye OCT.
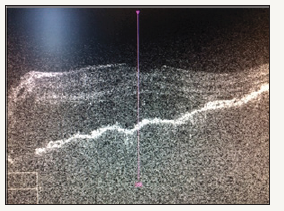
Figure 3: Three days after treatment: Right Eye OCT.
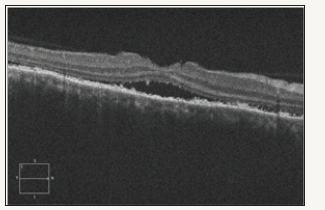
Figure 4: Three days after treatment: Left Eye OCT.
Discussion
Vogt-Koyanagi-Harada syndrome is a rare, inflammatory disease with manifestations affecting the ocular, central nervous, auditory-vestibular systems. It affects pigmented individuals between 20-50 years old [3,4]. Vogt-Koyanagi-Harada (VKH) syndrome affects various organs which containing melanocytes [5]. VKH syndrome is accompanied by cutaneous, neurological and auditory abnormalities in addition to bilateral uveitis. Various neurological signs such as headache, dizziness, tinnitus, optic neuritis, hemiparesia, ataxia are usually resolved with minimal sequelae. Dermatological findings include alopecia, poliozis, vitiligo appear several years after the beginning of the disease [6].
In our case, clinical manifestations have been presented with headache and blurred vision complaints. For this reason, VKH syndrome should be considered in the differential diagnosis of pseudotumor cerebri which can be seen with headache and papillary stasis. A detailed examination of patients with neurological complaints (especially similar neurological signs of VKH), in the presence of unexplained pathologies, is great importance in the diagnostic and prognostic sense. As a result, the diagnosis of VKH syndrome in these cases can be determined lately. The fact that progressive visual findings respond well to steroid treatment indicates the importance of early treatment.
References
- Ehlers JP, Shah CP (2008) Papilledema. In: The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. (5th edn). Lippincott Williams & Wilkins, Baltimore, Md, USA, pp. 252-254.
- Miller NR, Newman NJ, et al. (2008) Walsh & Hoyt’s Clinical Neuroophthalmology: The Essentials. (2nd edn), Lippincott Williams & Wilkins, USA, pp. 122-145.
- Gutteridge IF (1981) Optic nerve drusen and pseudopapilledema. Am J Optom Physiol Opt 58(8): 671-676.
- Rajendram R, Evans M, Rao NA (2005) Vogt-Koyanagi-Harada disease. Int Ophthalmol Clin 45: 115-134.
- Park S, Albert DM, Bolognia JL (1992) Ocular manifestations of pigmentary disorders. Dermatol Clin 10(3): 609-622.
- Read RW, Holland GN, Rao NA, Tabbara KF, Ohno S, et al. (2001) Revised diagnostic criteria for Vogt-Koyanagi-Harada disease: report of an international committee on nomenclature. Am J Ophthalmol 131(5): 647-652.
© 2018 Gamze Maden. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






