- Submissions

Full Text
Surgical Medicine Open Access Journal
A Case of Obscure GI Bleed Associated with Non-ITP Thrombocytopenia
Viswanath Reddy D1*, Srinivas Rao GR1, Sri Karan Uddesh T2 and Karuna Kumar K3
1Department of Gastroenterology, Yashoda Hospital, Secunderabad, India
2Department of Internal Medicine, Yashoda Hospital, Secunderabad, India
3Department of Haematology, Yashoda Hospital, Secunderabad, India
*Corresponding author:Viswanath Reddy D, Department of Gastroenterology, Yashoda Hospital, Secunderabad, India
Submission: April 25, 2024;Published: May 28, 2024

ISSN 2578-0379 Volume5 Issue5
Abstract
Obscure Gastrointestinal (GI) bleeding, defined by persistent or recurrent GI bleeding with source not identified on bidirectional endoscopy and small bowel radiological imaging accounts for nearly 5% of cases of GI bleeding [1]. Dieulafoy’s lesion is a potentially life-threatening condition wherein persistent caliber submucosal arteriole can bleed torrentially [2]. If there is associated thrombocytopenia, it could be devastating combination. We hereby present a case of obscure overt GI bleeding (Melena) due to Dieulafoy’s lesion in jejunum. She require blood transfusions for the quantum of GI bleeding. She had a rare inherited platelet disorder-Bernard Soulier syndrome [3] with non-ITP thrombocytopenia which was managed using Enteroscopy and APC of the lesion and blood products. We would like to highlight the need to follow a proper approach in managing bleeding tendency with thrombocytopenia to rule out inherited disorders and not blindly labelling it as ITP in a case of thrombocytopenia.
Keywords:Thrombocytopenia; Obscure gastrointestinal; Hemoglobin; glycoproteins
Introduction
We commonly come across cases of thrombocytopenia with or without bleeding, labelled as Idiopathic Thrombocytopenic Purpura (ITP), but we hereby describe a case with Obscure GI (jejunal) bleeding from a Dieulafoy’s lesion in a patient with thrombocytopenia managed using Enteroscopy in a middle-aged female which was not due to ITP but an inherited Platelet function disorder. Proper evaluation is the key to diagnosing these rare bleeding disorders.
Case Details
A 50-year-old woman who presented with melena (black stools) and a significant drop in Hemoglobin levels necessitating a blood transfusion. A thorough investigation into her medical history revealed a background of thrombocytopenia. Importantly, there was no history of overt gastrointestinal bleeding since childhood, and the patient had only received platelet transfusions during delivery (Childbirth). Initial endoscopic examinations, including both upper endoscopy and colonoscopy, did not reveal any abnormalities.
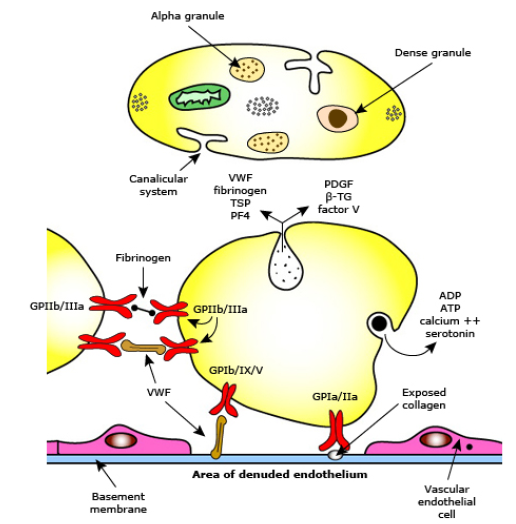
However, upon conducting capsule endoscopy, a proximal jejunal vascular lesion with active bleeding was identified. Subsequent push enteroscopy unveiled a? Dieulafoy’s lesion exhibiting active ooze. At the time of assessment, the patient’s platelet count was recorded at 40,000/cc. An APC (Argon Plasma Coagulation) procedure was performed on the vascular lesion as shown in Figure 1. Patient was doing well on 2 months follow up in OPD. This case was initially misdiagnosed as Immune Thrombocytopenia (ITP), further investigation was warranted in view of mild splenomegaly. Platelet aggregation studies played a pivotal role in arriving at an accurate diagnosis. These studies revealed a reduced response to Ristocetin. This clinical presentation raised suspicion of Bernard-Soulier Syndrome (BSS), a rare and severe bleeding disorder attributed to a deficiency in GPIb/IX/V3, a platelet complex responsible for binding von-Willebrand factor. As demonstrated in the Figure 2, there is a key role of Glycoprotein Ib/IX in binding to VWF. It is important to note that individuals with BSS may also exhibit pseudo thrombocytopenia due to the presence of giant platelets. Notably, the patient’s responses to ADP, collagen, and arachidonic acid were within the normal range.
Figure 1:Bleeding spot in Jejunum-APC being done.
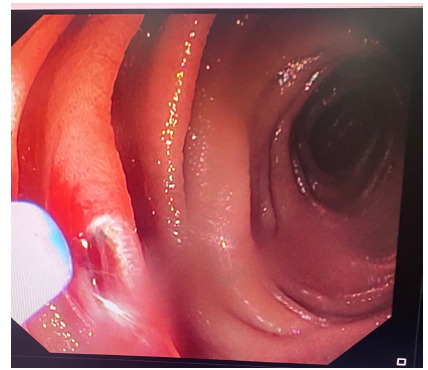
Figure 2:Platelet and the interactions. Bernard-Soulier syndrome(BSS) has defect at the level of GP Ib/IX.
Bernard-Soulier Syndrome (BSS) is an inherited platelet function disorder [3-5], Autosomal recessive in inheritance, confirmed through flow cytometry analysis of platelet glycoproteins.
It is imperative for clinicians to differentiate BSS from ITP, as
the treatment approaches differ significantly. Key differentiating
factors include:
a. Family History: While ITP may have a familial component [3],
a comprehensive family history of ITP can provide valuable
insights into the diagnosis.
b. Response to First-Line Treatment: Patients with BSS typically
do not respond to first-line interventions such as Intravenous
Immunoglobulin (IVIG) and steroids [3-5], in contrast to ITP
patients who may show improvement with these treatments.
c. Diagnostic Tests: Both light aggregation studies and flow
cytometry [3-5] are essential diagnostic tools in distinguishing
between the two conditions.
Conclusion
In conclusion, this case highlights the importance of management of obscure GI bleed with a stepwise approach and also underscores the importance of an appropriate diagnostic approach when encountering patients with bleeding disorders and thrombocytopenia. The differentiation between Bernard-Soulier syndrome and immune thrombocytopenia is pivotal for selecting the most appropriate treatment strategy. The line of treatment varies among the two different disorders.
References
- Raju GS, Gerson L, Das A, Lewis B (2007) American Gastroenterological Association (AGA) institute technical review on obscure gastrointestinal bleeding. Gastroenterology 133(5): 1697-1717.
- Nojkov B, Cappell MS (2015) Gastrointestinal bleeding from Dieulafoy’s lesion: Clinical presentation, endoscopic findings, and endoscopic therapy. World J Gastrointest Endosc 7(4): 295-307.
- Love G (2023) Inherited platelet function disorders (IPFDs).
- Bourguignon A, Tasneem S, Hayward CPM (2022) Update on platelet procoagulant mechanisms in health and in bleeding disorders. Int J Lab Hematol 44(1): 89-100.
- Boeckelmann D, Hengartner H, Greinacher A, et al. (2017) Patients with Bernard Soulier syndrome and different severity of the bleeding phenotype. Blood Cells Mol Dis 67: 69-74.
© 2024 Viswanath Reddy D. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






