- Submissions

Full Text
Surgical Medicine Open Access Journal
Colorectal Surgical Site Infection: How can we Decrease it?
Aldara Faria1,2, Teresa Pereira1,2, Sara Fernandes1,2, Daniel Jordão1,2, Carlos Ferreira1,2, Rui Esteves1,2, João Malaquias1, Fernanda Quirino1,2, Luís Miranda1,2 and Álvaro Ayres Pereira2,3*
1Department of General Surgery, Lisbon North University Hospital Center, Portugal
2Faculty of Medicine, University of Lisbon, Portugal
3GCL-PPCIRA coordinator, Lisbon North University Hospital Center, Portugal
*Corresponding author:Álvaro Ayres Pereira, Avenida Gomes Pereira, GCLPPCIRA coordinator, Hospital de Santa Maria, Centro Hospitalar Universitário Lisboa Norte, Lisbon, nº13. 1500-328 Lisboa, Portugal
Submission: July 07, 2023;Published: January 25, 2024

ISSN 2578-0379 Volume5 Issue4
Abstract
Introduction: Surgical Site Infection (SSI) is one of the most common postoperative complications in
surgery, with high morbidity. In our terciary-center we had a significant rate of surgical site infection.
Because of that we created a care bundle of measures in order to improve our outcomes.
Methods: Prospectively we implemented a care bundle with retrospective analysis, to decrease SSI. The
superficial, deep and organ/space infections were evaluated and compared before and after care bundle
implementation.
Result: Between January 1, 2016 and December 31, 2020, 1139 patient records relating to surgical
incisions were submitted for analysis. Until November 2017, we included 427 patients, 24,1% with SSI
in the post-operative period. From December 2017 on, we begun the implementation of all the measures
of our care bundle, which incorporate wound protector device, mechanical bowel preparation and
antibiotics. Until December 2020, we included 712 patients, with an SSI of 9,6%.
Conclusion: Surgical Site Infection (SSI) is the most frequent postoperative complication in colorectal
surgery and our terciary-center had an elevated surgical site infection. With the implementation of our
care bundle of measures, we significantly decreased SSI and since 2017 we’re keep going on that way.
Keywords:Surgical site infection; Colorectal surgery
Abbreviations:SSI: Surgical Site Infection; CDC: Center for Disease Control and Prevention; GCL-PPCIRA: Local Coordination Group-Prevention and Control Infections and Antimicrobial Resistance Program; HAISSI: Health-associated Infections-Surgical Site Infections; ECDC: European Centre for Disease Prevention and Control; IV: Intravenous; HSM: Hospital de Santa Maria
Introduction
Surgical Site Infection (SSI) is an infection of the incision or organ/space[1] that occur within 30 days after surgery if no implant is left in place or within one year if implant is in place [2]. According on the depth of involvement SSI is classified as superficial incisional, deep incisional or organ/space [2]. Surgical site infections are one of the most common complications that occur after a gastrointestinal surgery [2-8], with colorectal surgery reports rates up to 26-40% [5,9,10].
This health problem increases patient’s morbidity with important prolonged length of stay-up to 10 days [7], increased readmission rate, antibiotic use and higher costs and decreased quality of life [3,6-9]. In order to decrease surgical site infection in colorectal surgery the Center for Disease Control and Prevention (CDC) created a guideline to provide updated evidence-based recommendations [1]. Based on literature we created, in our tertiary center, a “care bundle” for patients undergoing colorectal surgical interventions that includes CDC measures plus wound protector device, mechanical bowel preparation and prophylactic antibiotics. The primary purpose of this study is to describe whether our “care bundle” resulted in decrease in SSI when used during the perioperative period of colorectal surgery.
Endocrinal (such as hyperthyroidism), drugs and toxins such as (caffeinated beverages, nicotine, hydralazine, atropine, adenosine, verapamil, salbutamol, ecstasy, cocaine, amphetamines alcohol, and digoxin toxicity), cardiovascular; structural heart disease such as (myocardial infarction, Ebstein anomaly, pericarditis, myocarditis, cardiomyopathy, pulmonary embolism, rheumatic heart disease, and mitral valve prolapse), chest diseases such as (pneumonia, chronic lung disease, chest wall trauma, and hypoxia), psychiatric such as (anxiety), vascular such as hypovolemia) are probable implicated factors for PSVT [8]. If patients are hemodynamically stable, vagal maneuvers, intravenous adenosine, diltiazem, or verapamil will be suggested treatment. However, if patients are hemodynamically unstable, cardioversion will be the choice of therapeutic option. Patients with symptomatic and recurrent PSVT can be treated with long-term drug treatment or catheter ablation [5].
Materials and Methods
Based in a proposal of STOP Hospital Infection, a Gulbenkian Foundation Project in collaboration with Portuguese Local Coordination Group - Prevention and Control Infections and Antimicrobial Resistance Program (GCL-PPCIRA) and the Institute for Healthcare Improvement (IHI), we create a prospective study with retrospective analysis of an implementation of a “care bundle of measures” in order to reduce the rate of SSI in our surgery department. We evaluate all patients who underwent elective open colorectal surgical procedures during a period of almost five years- May 5, 2016, to December 31, 2020.
Data from this period was collected by nurses and surgeons included in GCL-PPCIRA. The data was collected prospectively from the preoperative, intraoperative and 30 days postoperative periods based on Health-associated Infections-Surgical Site Infections (HAISSI) protocol from ECDC (European Centre for Disease Prevention and Control). Surveillance of surgical site infections and prevention indicators in European hospitals-HAI-Net SSI protocol, version 2.2. Stockholm: ECDC; 2017 [11]).
Why “care bundle” to prevent SSI?
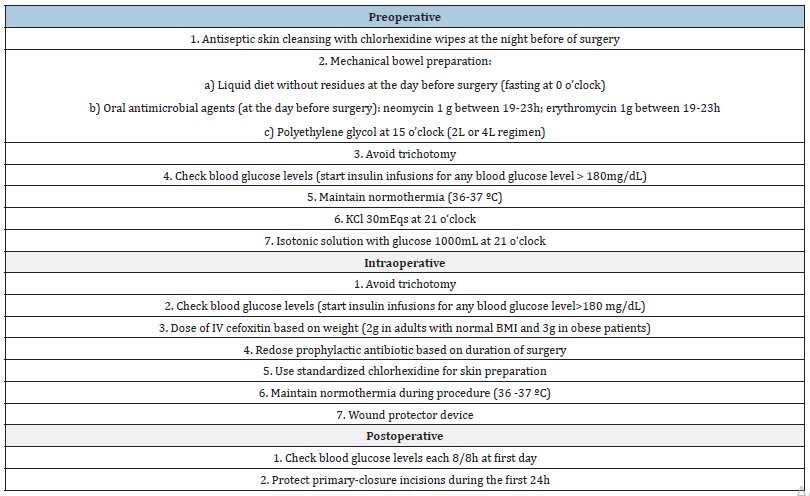
Colorectal surgery has a higher SSI rate compared with other surgeries [10] and since 2016 we reported all data from colorectal elective operations to GCL-PPCIRA program and rates of SSI were extremely high. So, inspired in CDC measures plus wound protector device, mechanical bowel preparation and prophylactic antibiotics reported in literature we proposed a “care bundle” table 1-our care bundle - to prevent surgical site infections. In July 2017 we introduce O-ring retractor to protect surgical incision and in November 2017 we introduce mechanical bowel preparation and antibiotics during the pre-operative period.
Data collection and analysis
Previously we established the definition of surgical site infections - superficial incisional, deep incisional or organ/spaceaccording to the literature [9,11,12]. All the staff involved in program was informed about all measures before its implementation. The colorectal team was responsible for 2, 6 and 7 of preoperative measures and 5 and 7 of intraoperative measures table 1 and the nurses and anaesthetic team were responsible for the others.
Table 1:Coloretal surgery care bundle.
We use definitions of the HAI-SSI protocol to superficial, deep and organ/space SSI’s which include microbiology study (during the first 30 days after surgery) and if the result was positive, we reported to GCL-PPCIRA. The SSI rates were reported every month to colorectal team and each semester we developed a chart, comparing each semester with the previously. Every month the total number of documented SSI’s was divided by the total number of patients undergoing colorectal elective operations. Rates for superficial, deep and organ/space SSIs were calculated similarly.
Result
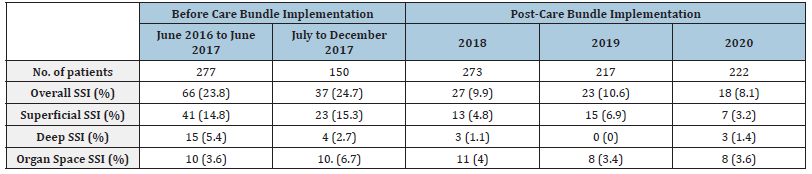
Between January 1, 2016 and December 31, 2020, 1139 patients record relating to surgical incisions were submitted for analysis. All patients were from HSM, Lisbon, and the surgery was performed in the main operating room of General Surgery by the same team. SSI rates were calculated according to global guidelines for the prevention of surgical site infection of World Health Organization [13]. During this period, a surgical safety checklist based on “our care bundle” was implemented and checked monthly and we observed a significant decrease of surgical site infections. Before care bundle intervention, our study included 427 patients, 103 of them with SSI (24.1%). After care bundle, 712 patients were submitted to surgical procedure and we reported an overall SSI of 9.6%, which confers a significantly decrease in SSI Table 2.
Table 2:Care bundle implementation: past and present.
Discussion
Surgical site infection is the most frequent complication after colorectal surgery and continues to be a major source of morbidity [3-8,12-16]. In the literature we reported a surgical site infection up to 40% [10,16], 50-60% of them could be preventable with evidence-based guidelines [1,12]. Length of hospital stay is three times longer for patients with SSI and there is two to eleven times higher risk of death [12,16]. On the other hand, the economic burden of SSI is associated with a 35% increase in direct healthcare costs [14]. The bowel-derived organisms are the most common involved in SSI and more than 20% are resistant to the prophylactic antibiotics [16]. An implementation of a SSI bundle with a multidisciplinary work pattern shows, in several relevant studies, a significantly reducing of SSI [14,17], with the most notable difference being the rate of superficial SSI [14]. Primary prophylaxis, which means the prevention of an initial infection, aims to prevent the development of SSI and/or improving SSIassociated morbidity [18] and gastrointestinal tract has numerous opportunistic pathogens that could easily contaminate the surgical site. Because of that, it is recommended preventive antibiotic treatment in colorectal surgery [19]. The infection rate was significant lower with oral plus i.e. antibiotics when compared with oral or i.e. antibiotics alone [20]. So it is recommended regimens that include oral neomycin and erythromycin plus a single dose of second-generation cephalosporin with aerobic and anaerobic activities (for example cefoxitin) or cefazolin plus metronidazole i.e. [21].
Despite of that the efficacy of oral antibiotic regimen has been proven only when Mechanical Bowel Preparation (MBP) was used [21,22], with osmotic agents, laxatives or a combination of them [22]. Based on evidence, in our department we use a polyethylene glycol, an osmotic agent, which is a not absorbed balanced solution, and an antibiotic regimen a like the one shown in table 1. Despite of all the measures we describe before and with literature review we include a wound protector device in our care bundle in order to improve our results.
Wound retractors/protectors are devices created to protect abdominal wall edges from trauma and bacterial contamination during surgery. Some studies suggest a decrease risk of SSI [6-8,23] - up to 45%-when the wound retractor is used [3] with a lower length of hospital stay [24]. In our series we perceived a statistically significant SSI reducing with the introduction of oral antibiotics and mechanical bowel preparation and a wound retractor.
In our study we analysed more than one thousands of patients submitted to colorectal surgery, most of them by median laparotomy, and we verified that with our care bundle implementation we significantly reduced the surgery’s morbidity and costs by reducing SSI. Since the final of 2020 we have continued to implement these measures and progressively switch from open to laparoscopic approach, hence having the sustained decrease of SSI as a primary goal in colorectal surgery.
Conclusion
During many years we observed an increase of surgical site infections secondary to colorectal surgery in our terciary-center. After the implementation of our reviewed care bundle measures in 2017, the reported overall rate of SSI was significantly reduced. Because of our results we believe that the global implementation of our care bundle will improve health care and we conclude that the time to prevention is before, during and post-surgery.
Acknowledgement
We would like to acknowledge all the department of GCLPPCIRA committee for all the support, namely nurses Sónia Albano, Teresa Amores and Paula Gil.
References
- Berriós-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, et al. (2017) Centers for disease control and prevention guideline for the prevention of surgical site infection. JAMA Surg 152(8): 784-791.
- Anderson DJ (2011) Surgical Site Infections. Netter’s Infect Dis 25(1): 135-53.
- Edwards JP, Ho AL, Tee MC, Dixon E, Ball CG (2012) Wound protectors reduce surgical site infection: a meta-analysis of randomized controlled trials. Ann Surg 256(1): 53-59.
- Tanishima H, Tamagawa K (2007) Randomized controlled investigation of the anti-infective properties of the alexis retractor/protector of incision sites. J Traum 62(1): 212-215.
- Dornfeld M, Lovely JK, Huebner M, Larson DW (2017) Surgical site infection in colorectal surgery: A study in antibiotic duration. Dis Colon Rectum 60(9): 971-978.
- Mohan HM, Mcdermott S, Fenelon L, Fearon NM, Connell PRO, et al. (2012) Plastic wound retractors as bacteriological barriers in gastrointestinal surgery : a prospective multi-institutional trial. J Hosp Infect 81(2): 109-113.
- Cheng KP, Roslani AC, Kueh JH, Law CW, Chong HY, et al. (2012) ALEXIS O-Ring wound retractor vs conventional wound protection for the prevention of surgical site infections in colorectal resections (1). Colorectal Dis 14(6): 346-351.
- Reid K, Pockney P, Draganic B, Smith SR (2010) Barrier wound protection decreases surgical site infection in open elective colorectal surgery : A randomized clinical trial. Dis Colon Rectum 53(10): 1374-1380.
- Lutfiyya W, Parsons D, Breen J (2012) A colorectal ‘care bundle’ to reduce surgical site infections in colorectal surgeries: a single-center experience. Perm J 16(3): 10-16.
- Chen M, Song X, Chen LZ, Lin ZD, Zhang XL (2016) Comparing mechanical bowel preparation with both oral and systemic antibiotics versus mechanical bowel preparation and systemic antibiotics alone for the prevention of surgical site infection after elective colorectal surgery: a meta-analysis of randomized controlled clinical trials. Dis Colon Rectum 59(1): 70-78.
- (2017) ECDC. Surveillance of surgical site infections and prevention indicators in European hospitals HAISSI protocol.
- Anderson DJ, Podgorny K, Berrı SI, Bratzler DW, Dellinger EP, et al. (2014) Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol 35(6): 605-627.
- Global guidelines for the prevention of surgical site infection. World Heal Organ. Switzerland pp. 1-186.
- Falconer R, Ramsay G, Hudson J, Watson A (2021) Reducing surgical site infection rates in colorectal surgery-a quality improvement approach to implementing a comprehensive bundle. Color Dis 23(11): 2999-3007.
- Fry DE (2016) Infection control in colon surgery. Langenbeck’s Arch Surg 581-597.
- Collaborative G (2018) Surgical site infection after gastrointestinal surgery in high-income, middle-income, and low-income countries: a prospective, international, multicentre cohort study. Lancet Infect Dis 18(5): 516-525.
- Guerrero MA, Anderson B, Carr G, Snyder KL, Boyle P, et al. (2021) Adherence to a standardized infection reduction bundle decreases surgical site infections after colon surgery: A retrospective cohort study on 526 patients. Patient Saf Surg 15(1): 15.
- Ongom PA, Kijjambu SC (2013) Antibiotic prophylaxis in colorectal surgery: evolving trends. Journal of Molecular Pharmaceutics & Organic Process Research 1(3): 109.
- Min BW (2015) Efforts to prevent surgical site infection after colorectal surgery. Ann Coloproctol. 31(6): 21-212.
- Nelson RL, Glenny Am, Song F (2009) Antimicrobial prophylaxis for colorectal surgery 21(1): CD001181.
- Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, et al. (2013) Clinical practice guidelines for antimicrobial prophylaxis in surgery. Surg Infect (Larchmt)14(1): 73-156.
- Kumar AS, Kelleher DC, Sigle GW (2013) Bowel preparation before elective surgery. Clin Colon Rectal Surg 26(3): 146-152.
- Ahmed K, Bashar K, Connelly TTM, Fahey T, Walsh SR (2016) Reducing surgical site infections in abdominal surgery: Are ring retractors effective? A systematic review and meta-analysis. Surg Infect (Larchmt) 17(2): 138-151.
- Capolupo GT, Lauricella S, Mascianà G, Caricato C, Angeletti S, et al. (2019) O-ring protector in prevention of SSIs in laparoscopic colorectal surgery. J Soc Laparoendosc Surg 23(4): e2019.00048.
© 2024 Álvaro Ayres Pereira. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






