- Submissions

Full Text
Surgical Medicine Open Access Journal
Urgent Myocardial Revascularization after Previous Surgery for Gunshot Wounds to the Heart and Lungs
Lazoryshynets VV, Rudenko AV, Krykunov OA, Kupchinsky OV, Salo SV*, Levchyshyna OV, Yu Hladun A, Tokhtarov VV, Bondarets DV and Vitovsky AR
National Amosov Institute of Cardiovascular Surgery of the National Academy of Medical Sciences of Ukraine, Ukraine
*Corresponding author: Salo SV, National Amosov Institute of Cardiovascular Surgery of the National Academy of Medical Sciences of Ukraine, Kyiv, Ukraine
Submission: April 18, 2022Published: May 26, 2022

ISSN 2578-0379 Volume5 Issue1
Abstract
Due to the full-scale invasion of the Russian Federation in Ukraine, many patients with injuries of various nature and severity appeared. Damage to the heart and blood vessels is the biggest threat to human life. Patients with injuries of this nature have been treating in Amosov National Institute of Cardiovascular Surgery since the first day of the war. One of them was young man with elevation of the ST segment after surgery for gunshot wounds to the heart and lungs. After non-invasive research methods, coronary angiography was performed followed by an attempt of endovascular revascularization. Due to the impossibility of complete blood-flow restoration and dye extravasation patient was directed to urgent surgical treatment [1].
Keywords: Acute coronary syndrome; LAD artery; Gunshot wound; Urgent surgical revascularization; Mechanical occlusion
Case Description
Figure 1: ECG, ST segment elevation.
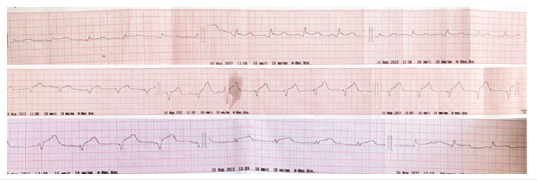
Figure 2: CT, mechanical occlusion of the middle segment of the LAD artery.

Figure 3: Transthoracic echocardiography, apical 2-chamber view (zoom), showing the affected area (white arrow) - anterior septal LV, LV, left ventricle.
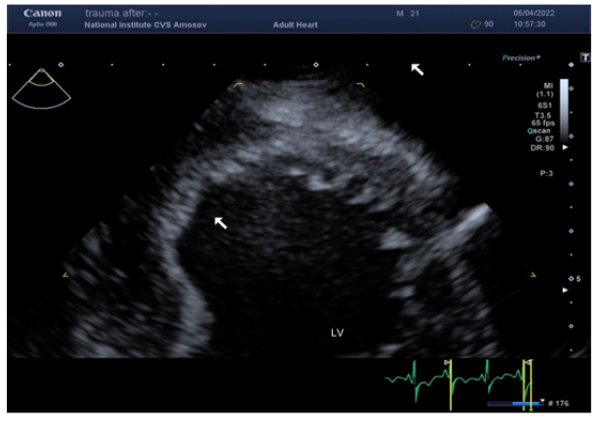
30.03.22, Patient D, 21 y.o., was taken to the Amosov National Institute of Cardiovascular Surgery with a diagnosis of Acute coronary syndrome with elevation of the ST segment after surgery for gunshot wounds to the heart and lungs (Figure 1). From the anamnesis: Gunshot wound to the left half of the chest with damage to the heart, left lung, ribs; gunshot wound to the left shoulder in the upper third with a fragmentary fracture of the humerus, damage to the radial nerve [2,3]. During hostilities, in one of the district hospitals urgently performed left lateral thoracotomy, suturing of the left lung, suturing of the heart wound in the projection of the LAD artery. Primary surgical treatment of a shoulder wound, application of an external fixation device. During the operation, autohemotransfusion was performed in a volume of 900 ml. Erythrocyte mass transfusion was performed. The patient was directed to the Amosov National Institute of Cardiovascular Surgery. Upon admission to the institute, the following examinations were performed: ECG, echocardiography, chest CT with contrast, coronary angiography. According to the ECG revealed acute ischemia of the anterior-membranous-apical-lateral part of the left ventricle (acute coronary syndrome with ST elevation of the anterior wall of the left ventricle) [4]. CT examination with gadolinium contrast revealed signs: CT signs of penetrating injury of the left hemithorax with the presence of mechanical occlusion of the middle segment of the LAD artery (bone / metal fragment), the presence of squamous lesions S10 of the left lung (Figure 2). Subtotal contusion of the left lung. Large left pneumothorax, small left hydrothorax. Small pneumomediastinum. CT signs of anemia. Echocardiography examination of the pathology of the heart valves and intracardiac structures did not reveal (Figure 3). Attention was drawn to the hypokinesia of the apical-membranous part of the left ventricle [5].
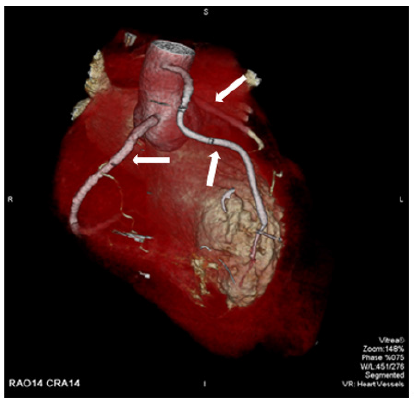
The patient was taken to the catheterization laboratory. Coronary angiography was performed by distal transradial access. Occlusion of mid. LAD artery and DIA1, TIMI 0 blood flow were detected (Figure 4). With technical difficulties, the coronary guidewire was introduced through the occlusion zone into the distal part of the LAD artery. Gradual angioplasty of the stenosis zone was performed with high-pressure balloons (diameters of 2.5, 3.0, 3.5) by pressure of up to 28 atmospheres (Figure 5). Angiographic pattern during balloon inflation is characteristic of suturing the artery with suture material. After angioplasty, blood flow was restored, TIMI 2 (Figure 6). Extravasation of contrast in the area of the Ellis-2 ligature was detected. Therefore was made a decision to perform urgent surgical treatment. The patient was taken to the operating room in an emergency. In aseptic conditions after treatment of the operating field with Ethanol solution (7 times) under combined endotracheal anesthesia performed a longitudinal median sternotomy. The pericardium was dissected [6,7]. A large subcutaneous vein was isolated from the left leg. Hematoma in the area of LAD artery was visualized. The beating-heart technique was used. Collapse of the left lung was eliminated. A hematoma was visualized on the anterior wall of the chest [8,9]. No sources of active bleeding were identified. The left pleural cavity was sutured tightly. Opening of LAD artery in the middle third, diameter 1.2mm. LAD artery was anastomosed with aorta by venous autographt. Hemostasis control. Drainage in the pericardium, thoracic. Steel seams on the sternum. Layer-stitched wound. Leather seam. Aseptic dressing. Blood loss 150ml. Postoperative period was without complications. Angiography was performed (Figure 7). 3D CT was performed (Figure 8) [10,11].
Figure 4: Angiography Occlusion of mid LAD artery and DIA1, TIMI 0 blood flow.
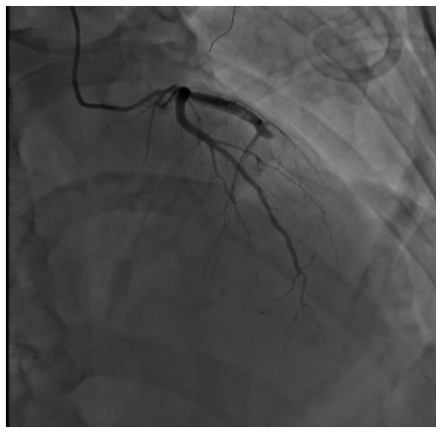
Figure 5:Angiography angioplasty of the stenosis zone with high-pressure balloon.
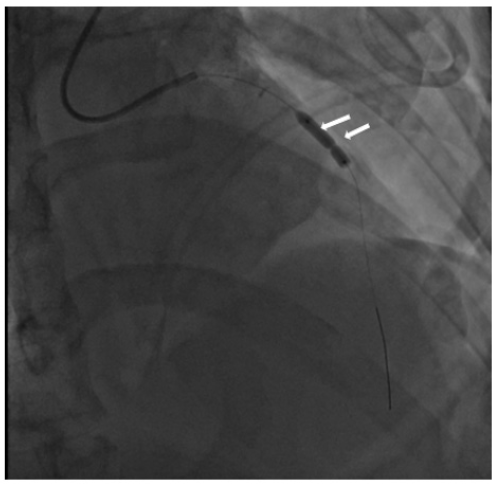
Figure 6: Angiography blood flow after angioplasty and dye extravasation.
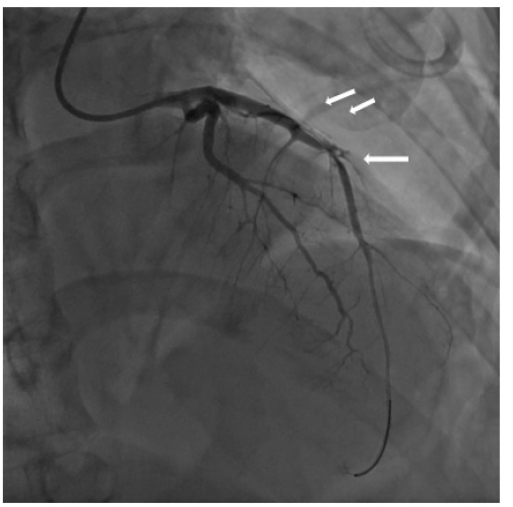
Figure 7: Angiography after venous autographt anastomosis: a) LAD artery occlusion b) Visualization of the venous autographt anastomosis.
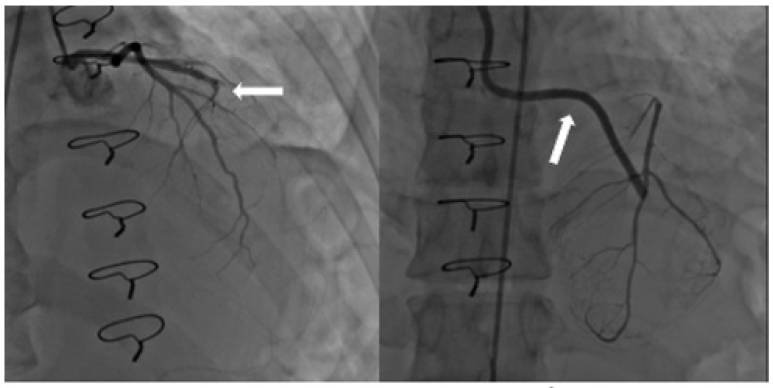
Figure 8: 3D CT after venous autographt anastomosis. Arrows show: RCA, venous autographt anastomosis, LAD artery (from the left to the right).
Conclusion
A system of timely evacuation of victims must be established during hostilities. After the initial surgical treatment, patients with severe injuries should be taken to specialized care centers for further highly qualified treatment.
References
- Benstoem C, Stoppe C, Liakopoulos OJ, Ney J, Hasenclever D, et al. (2017) Remote ischaemic preconditioning for coronary artery bypass grafting (with or without valve surgery). Cochrane Database of Systematic Reviews 5(5).
- Zhao DF, Edelman JJ, Seco M, Bannon PG, Wilson MK, et al. (2017) Coronary artery bypass grafting with and without manipulation of the ascending aorta: A network meta-analysis. J Am Coll Cardiol 69(8): 924-936.
- Reynolds AC, King N (2018) Hybrid coronary revascularization versus conventional coronary artery bypass grafting: Systematic review and meta-analysis. Medicine 97(33).
- Benedetto U, Raja SG, Albanese A, Amrani M, Biondi-Zoccai G, et al. (2015) Searching for the second best graft for coronary artery bypass surgery: A network meta-analysis of randomized controlled trials. Eur J Cardiothorac Surg 47(1): 59-65.
- Nuffield Trust & Health Foundation (2015) Indicator: International comparisons of surgical procedures. Quality watch, United Kingdom.
- Shibata T, Kawakami S, Noguchi T, Tanaka T, Asaumi Y, et al. (2015) Prevalence, clinical features, and prognosis of acute myocardial infarction attributable to coronary artery embolism. Circulation 132(4): 241-250.
- Violi F, Soliman EZ, Pignatelli P, Pastori D (2016) Atrial fibrillation and myocardial infarction: A systematic review and appraisal of pathophysiologic mechanisms. J Am Heart Assoc 5(5).
- Raphael CE, Heit JA, Reeder GS, Bois MC, Maleszewski JJ, et al. (2018) Coronary embolus: An underappreciated cause of acute coronary syndromes. JACC: Cardiovascular Interventions 11(2): 172-180.
- Baker JB, Marc Northern MD, Frament C, Aaron Baker D, Remick K, et al. (2020) Austere resuscitative and surgical care in support of forward military operations-joint trauma system position paper. Mil Med.
- Edwards MJ, Edwards KD, White C, Shepps C, Shackelford S (2016) Saving the military surgeon: Maintaining critical clinical skills in a changing military and medical environment. J Am Call Surg 222(6): 1258-1264.
- Tadlock MD, Carr M, Diaz J, Rhee P, Cannon JW, et al. (2021) How to maintain the readiness of forward deployed caregivers. J Trauma Acute Care Surg 90(5): e87-e94.
© 2022 Salo SV. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






