- Submissions

Full Text
Surgical Medicine Open Access Journal
Intracranial Ependymomas in Children the Role of Surgery and the Adjuvant Therapy
Bouaita K*, Atroune L, Selmane T and Habchi N
Neurosurgery Department, Neuroplasticity and Glial Tumors Laboratory, Algeria
*Corresponding author: Bouaita K, Neurosurgery Department, Neuroplasticity and Glial Tumors Laboratory, Algeria
Submission: October 25, 2021Published: January 17, 2022

ISSN 2578-0379 Volume4 Issue4
Abstract
The purpose: The management of intracranial ependymomas represents a real challenge and the perfect treatment modality remains controversed. The goal of this study is to highlight the role of tumour removal and the adjuvant therapy in the survival rate of children presenting with intracranial ependymomas. Patients and methods: This retrospective study of 56 children presenting with non-metastatic intracranial ependymomas treated in the period between 2015 and 2020. The age varies from 3 months to 15 years while the mean age was 8 years. The infra tentorial location was found in 67.8%. Result: The total resection of the tumour was achieved in only 42.8% of cases, whereas the subtotal resection was performed in 35.7%. More than 50% of tumours were grade I and II of the Who classification (grade I: 12 cases, grade II: 18 cases). 44.6% were anaplasique ependymomas (grade III: 25 cases). More than half of our cases had initial adjuvant radiotherapy (55.3%) and 21.4% had chemotherapy. 4 children had both radiotherapy and chemotherapy. Complications that were found in our serie were 6 cases of CSF fistula in the origin of 4 cases of meningitis, 9 cases of neurological deterioration with 2 cases of postoperative seizures and 2 other cases of intra ventricular haemorrhage. The mortality rate after 38 months was 7.1% (4 cases). The Follow-up length was 5 years. Conclusion: The role of surgery and the extent of resection in the intracranial ependymomas in children remains the most important factor in the global management of this type of intracranial tumour. adjuvant radiotherapy helps achieving a survival rate for the anaplastic types and recurrences.
Keywords: Anaplastic ependymomas; Ependymomas; Radiotherapy
Introduction
Ependymomas are neuro epithelial tumours derived from a neoplastic transformation of ependymal cells that line the ependymal cavity and take part in the glial group of tumours representing 2-9% of all intra cranial tumours and more than 12% of intra cranial tumours in children. 75% of these tumours are located in the posterior cerebral fossa [1-3]. The first histological description of ependymomas was performed by Virchow in 1864. Bailey and Cushing in 1926 classified ependymomas among the glial tumours [1]. Ependymomas of the posterior cerebral fossa affect particularly young infants, whereas the supra tentorial location affects older children, adolescents and adults [1-3]. These tumours manifest clinically with a high intra cranial pressure cerebellar syndrome and focal neurological symptoms. The insertion of posterior fossa ependymomas adhere to the floor of the 4th ventricle (in 80%) and more precisely in the bulbar triangle in contact with vital neurological structures. In this location, ependymomas can develop through the magendie hole to gain size in the cervical subarachnoid space or toward the ponto cerebellar angle and distal cranial nerves through the luschka hole. The upward extension toward the 3rd ventricle is exceptional through the sylvius aqueduct. Their treatment is surgical and can be completed by radiotherapy and/ or chemotherapy as an adjuvant therapy [2-5]. In addition to the problem of the extent of resection, which is usually incomplete due to their location, the prognostic of ependymomas is difficult to predict due to their risk of recurrence and the possibility of distant metastatic implantation through CSF pathways [5]. Radiotherapy has an important role in the treatment of recurrent ependymomas as well as the anaplastic types [2,6].
Patients and Methods
We are presenting a retrospective study of 56 patients operated in the period between 2015 and 2020 at cherchell specialized hospital in Algiers. Female predominance was found in our serie (29 females and 27 males). The mean age was 8 years with extremes varying from 3 months to 15 years.
Result
Location
The infratentorial location of intracranial ependymomas in
children was found in 36 cases (67.8%) whereas the supra tentorial
location concerned 18 patients (32.2%). In detail, the infra tentorial
location reflects many precise locations of these tumours (Table 1):
a. 18 cases of ependymomas of the floor of the 4th ventricle
(Figure 1).
b. 4 cases of ependymomas with extension toward the bulbo
medullar junction and the second cervical vertebra.
c. 12 cases of the roof of the 4th ventricle.
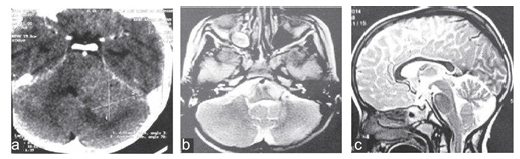
d. 7 cases of the lateral recess with extension toward the
homolateral cerebellar pontine angle (Figure 2).
Table 1. Number of the main clinical symptoms. Clinical features are multiform.
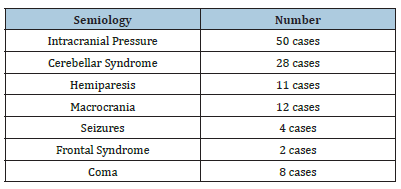
Figure 1: a, b: Preoperative MRI in sagittal and axial views show an important ependymomas of the Posterior cranial fossa with cisternal extension. c: Early post-operative CT scan showing the extent of the tumour removal after Radiotherapy. d: Image of cervical MRI in sagittal view show a cervical ependymoma in the same patient after 3years follow-up.
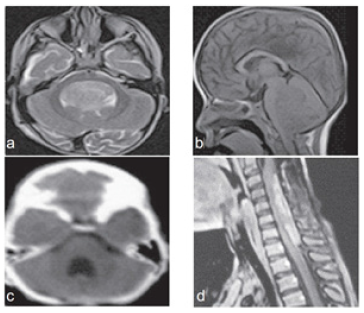
Figure 2: a, b: preoperative CT scan showing an ependymoma of the roof of the 4th ventricle with extension toward the cerebello pontine angle. c: MRI in sagittal view showing the quality of resection after radiotherapy and two years follow up.
The supra tentorial location involved
i. 11 cases of lateral ventricle (Figure 3).
ii. 1 case was para ventricular.
iii. 6 cases were para and intra ventricular (Figure 4).
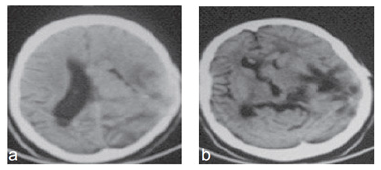
Figure 3: CT scan of intraventricular ependymoma (a) and the extent of the resection after 4 years follow up (b).
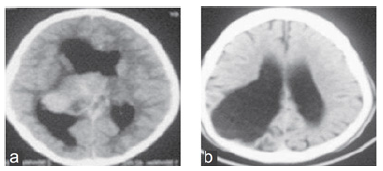
Figure 4: Preoperative CT scan (a) of an intra ventricular ependymoma and post-operative image showing the resection quality (b).
Extent of tumour removal
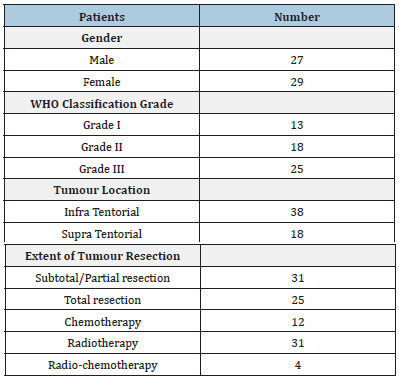
Post-operative imaging (CT scan and MRI) were used to assess the extent of the tumour removal. The majority of our patients underwent CT scan immediately after surgery (Table 2). MRI was performed after a few weeks to evaluate the extent of the tumour resection. The Gros total resection was achieved in 42.8% of patients (25 cases), whereas 25 others had a subtotal resection of infra tentorial locations of the studied ependymomas in Children.
Table 2. Patients features with treatment modality.
Histological grade
More than half of tumours were ependymomas myxopapillary or sub ependymomas of grade I and II of the WHO classification of CNS tumours. 12 cases were grade I and 18 were grade II. The grade III anaplastic ependymomas were found in 44.6% of cases (25 cases).
Adjuvant treatment
More than half of our patients (55.3%) have had radiotherapy as a complementary treatment initially, whereas 21.4% of them received chemotherapy. 4 children received both radiotherapy and chemotherapy.
Morbidity
In the post-operative period, we have recorded complications
listed below:
i. 6 cases of CSF fistula after surgery of 6 cases of infra
tentorial ependymomas. 4 cases presented meningitis and
were treated with targeted antibiotics.
ii. One case presented with a cervical metastasis was réoperated
few months after the first surgery with anatomo
pathological finding showed an ependymoma.
iii. Two patients presented with post-operative intra cranial
pressure due to mal function of VP shunt, they improved after
revision.
Prognostic
All our patients were followed up regularly after 36 months especially those for which the tumour removal was nor complete and who have had radiotherapy or chemotherapy. The residual tumour was unchanged and was followed up by oncologists and neurosurgeons. Two cases of supratentorial ependymomas show a late recurrence and were re operated on with an adjuvant chemotherapy. 4 cases of mortality were recorded in the period of 38 months after surgery.
Discussion
The intra cranial ependymomas represent the third more frequent tumour of the central nervous system in children. Although these tumours can affect patients of every age, 50% of intra cranial ependymomas involve children under 5 years old affecting particularly the infra tentorial compartment in 70-80%. The intracranial ependymomas affects the supra tentorial compartment in adults [6-8]. In our Serie, the infratentorial location was found in 67.8%. in the infancy, Ependymomas are particularly malignant which is different from tumours diagnosed in older children of 10- 15 years of age which have a lower grade. The surgical removal of ependymomas is difficult due to its close relationship to the brainstem, cranial nerves. This feature reflects a dilemma between a total resection with a high risk of morbidity and partial resection with high risk of recurrence and a good post-operative outcome. Many studies argue that the total resection offers a better longterm control. Ikezaki [9] consider that the location and the size of infra tentorial ependymomas were important factors for long term prognosis. The infratentorial ependymomas are then classified into: ependymomas of the roof, floor and the lateral recess of the fourth ventricle. In the latter, the tumour encases cranial nerves IX, X, XI, XII and adhere to the brainstem [10].
The majority of authors agree that the anaplastic type has a poor prognosis whereas the prognosis is variable for the other types of ependymomas. Also, less than 5% of ependymomas are infiltrative at the time of diagnosis which was not taken into account in the classification of patients. In the other hand biomarkers under study could be good prognosis predictors. One of the most important challenges in the management of intra cranial ependymomas is to determine the most optimal multimodal therapy for these tumours. Surgery has an important role in the treatment of intracranial ependymomas and the extent of resection influence highly the overall prognosis. Nowadays, majority of authors agree to perform surgery on these patients and tend to achieve the most complete resection followed by radiotherapy. In series published by Sutton et al., the survival rate after 5 years was 60% for patients who had a total or subtotal removal against 21% for children who had partial removal or biopsy [11]. However, surgery is rarely curative and recurrences are mainly local.
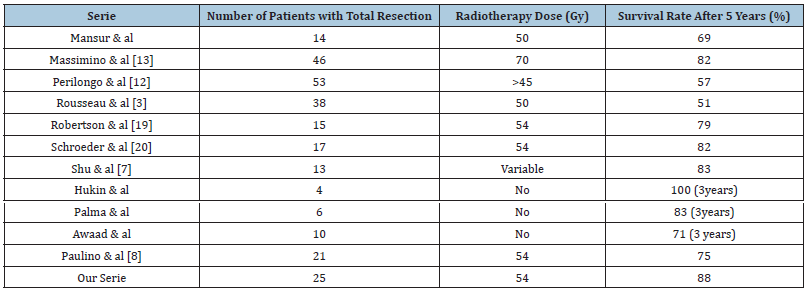
In our Serie the total resection was achieved in 42.8% of cases (25 cases) with a partial resection in 35.7%. The survival rate after 5 years was 88% after surgery followed by radio therapy. Shu et al. [7] report a survival rate of 40.7-66.2% with a mean survival length of 110.2 months according to a Serie of 49 infants treated at university hospital in Pennsylvania [10]. Mansur, et al. followed up 60 patients in 10 years and had a survival rate of 49.5-55% at Washington university school of medicine with a mean survival length of 12.5 years [12]. Paulino [8] followed up 49 children for 9.6 years and had a survival rate of 60.3-71.4% with 5 years of local control. The conventional radiotherapy has good tumour control after total resection. Radiotherapy should include brainstem and cervical medulla and has less effects on neurocognitive function according to the literature [13-16]. There is no consensus concerning the age to receive radiotherapy, certain authors used radiotherapy in children of 1 year. The benefit of chemotherapy is far from being proved. Some studies suggested that there is no benefit to add chemotherapy concomitant or after radiotherapy. On the other hand, other studies show the efficiency of chemotherapy in anaplastic ependymoma before radiotherapy [17]. Other authors tried to use chemotherapy to delay the need of radiotherapy particularly for vulnerable patients who cannot handle the effect of radiotherapy such as children younger than 3 years old. Ependymomas in children is one of the most frustrating pathologies that the neurosurgeon face from the prognosis point of view. Factors such as age, location, extend of the resection, histological type and the efficiency of complementary treatment are not sufficient to predict the prognosis. Nowadays, molecular biology is interesting for many authors and can identify a group of a poor prognosis with poor global survival. The therapeutic strategy could be then targeted better [18].
Conclusion
Ependymomas are relatively aggressive and resistant to adjuvant therapies. The severity observed during evolution of ependymomas is related to risk of recurrence and CSF metastasis. The total removal of ependymomas is particularly difficult due to their situation inside the ventricular cavity but that remains the best option to achieve a long survival [19-23] (Table 3). In the opposite, the attempt to a total resection exposes the patient to serious morbidity. Adjuvant radiotherapy for patients with a low risk who had complete resection is reasonable option.
Table 3. Survival rate of children after surgical resection followed by radiotherapy according to different series of the literature.
References
- Boop FA, Sgouros S (2009) Intracranial ependymoma in children: Current status and future trends on diagnosis and management. Childs Nerv Syst 25: 1163-1165.
- Sunanda P, Mei-Yin P, Rosenberg-Wohl S, Chennupati S, Prados MD, et al. (2012) Pediatric intracranial ependymoma: The roles of surgery, radiation and chemotherapy. J Neurooncol 106(2): 367-375.
- Rousseau P, Habrand JL, Sarrazin D, Kalifa C, Terrier-Lacombe MJ, et al. (1994) Treatment of intracranial ependymomas of children: Review of a 15-year experience. Int J Radiat Oncol Biol Phys 28(2): 381-386.
- Tamburrini G, D'Ercole M, Pettorini BL, Caldarelli M, Massimi L, et al. (2009) Survival following treatment for intracranial ependymoma: A review. Childs Nerv Syst 25(10): 1303-1312.
- Andrew SL, Sheean T, Manoharan R, Darbar A, Teo C (2009) The management of completely resected childhood intracranial ependymoma: The argument for observation only. Childs Nerv Syst 25(3): 281-284.
- David BM, Arie P, Veena R, Jeff MM, Park TS, et al. (2005) Postoperative radiation therapy for grade II and III intracranial ependymoma. Int J Radiat Oncol Biol Phys 61(2): 387-391.
- Shu HG, Sall WF, Maity A, Tochner ZA, Janss AJ, et al. (2007) Childhood intracranial ependymoma: twenty-year experience from a single institution. Cancer 110(2): 432-441.
- Paulino AC, Wen B, Buatti JM, Hussey DH, Zhen WK, et al. (2002) Intracranial ependymomas: An analysis of prognostic factors and patterns of failure. Am J Clin Oncol 25(2): 117-122.
- Ikezaki K, Matsushima T, Inoue T, Yokoyama N, Kaneko Y, et al. (1993) Correlation of microanatomical localization with post-operative survival in posterior fossa ependymomas. Neurosurgery 32(1): 38-44.
- McGuire CS, Sainani KL, Fisher PG (2009) Both: Location and age predict survival in ependymoma: A SEER study. Pediatr Blood Cancer 52(1): 65-69.
- Sutton LN, Goldwein J, Perilongo G, Lang B, Schut L, et al. (1990) Prognostic factors in childhood ependymomas. Pediatr Neurosurg 16(2): 57-65.
- Perilongo G, Massimino M, Sotti G, Belfontali T, Masiero L (1997) Analysis of prognostic factors in a retrospective review of 92 children with ependymomas: Italian pediatric neuro-oncology group. Med Pediatr Oncol 29(2): 79-85.
- Massimino M, Gandola L, Giangaspero F, Sandri A, Valagussa P, et al. (2004) Hyperfractionated radiotherapy and chemotherapy for childhood ependymomas: Final results of the first prospective AIEOP. Int J Radiat Oncol Biol Phys 58(5): 1336-1345.
- Mulhern RK, Merchant TE, Gajjar A, Reddick WE, Kun LE (2004) Late neurocognitive sequelae in survivors of brain tumours in childhood. Lancet Oncol 5(7): 399-408.
- Copeland DR, Demoor C, Moore BD, Ater JL (1999) Neuro cognitive development of children after a cerebellar tumor in infancy: A longitudinal study. J Clin Oncol 17: 3476-3486.
- Riva D, Giorgi C (2009) The neuro developmental price of survival in children with malignant brain tumours. Childs Nerv Syst 16(10-11): 751-754.
- Spiegler BJ, Bouffet E, Greenberg ML, Rutka JT, Mabbott DJ (2004) Change in neuro cognitive functioning after treatment with cranial radiation in childhood. J Clin Oncol 22(4): 706-713.
- Richard GG, Sophie AW, Claire LW, Kath R, Linda SL, et al. (2007) Primary postoperative chemotherapy without radiotherapy for intracranial ependymoma in children: The UKCCSG/SIOP prospective study. Lancet Oncol 8(8): 696-705.
- Robertson PL, Zeltzer PM, Boyett JM, Rorke LB, Allen JC, et al. (1998) Survival and prognostic factors following radiation therapy and chemotherapy for ependymomas in children: A report of the children’s cancer group. J Neurosurg (1998) 88(4): 695-703.
- Schroeder TM, Chintagumpala M, Okcu MF, Chiu JK, Teh BS, et al. (2008) Intensity-modulated radiation therapy in childhood ependymomas. Int J Radiat Oncol Biol 71(4): 987-993.
- Grill J, Deley MC, Gambarelli D, Raquin MA, Couanet D, et al. (2001) Post-operative chemotherapy without irradiation for ependymoma in children under 5 years of age: A multi center trial of the French Society of Pediatric Oncology. J Clin Oncol 19(5): 1288-1296.
- Matthew K, Shayna R, Thomas EM, Usama M, William FR (2011) Post-operative radiation improves survival in children younger than 3 years with intracranial ependymoma. J Neuro oncol 105(3): 583-590.
- Kim J-H, Huang Y, Griffin AS, Rajappa P, Greenfield JP (2013) Ependymoma in children: Molecular considerations and therapeutic insights. Clin Transl Oncol 15(10): 759-765.
© 2022 Bouaita K. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






