- Submissions

Full Text
Surgical Medicine Open Access Journal
Thymoma-A Giant Thymoma in a 9 Years Old Girl: Case Report
Enrique Tomé1, Claudia Cortés2 and Allan Delcid2*
1Pediatric Surgeon, Honduras
2General Surgeon, Doctor of Medicine and Surgery, National Autonomous University of Honduras, Honduras
*Corresponding author: Allan Delcid, General Surgeon, Doctor of Medicine and Surgery, National Autonomous University of Honduras, Honduras
Submission: November 26, 2021Published: December 08, 2021

ISSN 2578-0379 Volume4 Issue4
Abstract
Thymomas is a rare mediastinal mass in children. The 2-9% of all thymic tumors are a thymolipoma, an usnusual benign mediastinal mass composed of thymic and adipose tissue, they are usually present in young adults. In this paper we report a case of 9 years old girl with a giant intrathoracic left- sided mass, involving all compartments of the mediastinum. Left posterolateral toracothomy was performed and the mass was complete resected. The patient was discharged 6 days postoperative with a good evolution.
Keywords: Thymoma; Thymolipoma; Mediastinal; Adipose Tissue; Posterolateral; Radiotherapy; Toracothomy; Chemotherapy
Abbreviations: TN: Thymic Neoplasm; WHO: World Health Organization
Introduction
Thymomas are epithelial neoplasms with variable amount of lymphocytes. There are infrequent in the pediatric population, representing only 1-2% of mediastinal tumors [1]. Only one third of patients have symptoms, being an accidental discovery. They are typically classified as noninvasive or invasive tumors [1]. The benign type has an excellent prognosis and complete surgical resection is the solution. For invasive thymomas radiotherapy and chemotherapy offers survival advantage.
Case Report
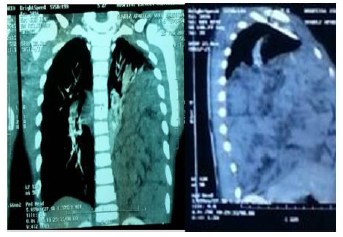
A nine year old girl was admitted for evaluation after presenting 3 days of abdominal pain, in right iliac fosse, five episodes of diarrhea and one episode of fever. Also she referred one week of cough and one day of breathing difficulty. She had a history of Asthma since the age of 4 year, with unknown management. The physical examination revealed fever and normal vital signs. On chest auscultation right crackles and left hypoventilation. The abdomen was soft with level pain in right iliac fosse. White blood cells count was normal, an abdominal ultrasound reported right-sided hypoechoic ovoid adenopathy of 1x0.8cm compatible with a mesenteric adenitis. A chest x-ray was done and this revealed a left homogenous opacity (Figure 1). A left lateral chest x-ray showed the opacity involved anterior, medial and posterior mediastinum (Figure 2). Further evaluation by a TC scan of the thorax revealed a mix density mass (cystic and solid) involving 80% of the left hemithorax, with dimension of 14.6x7.6x13cm, approximately volume of 750ml, in contact with the diaphragm (Figure 3).
Figure 1: Chest X ray showed left homogenous opacity.

Figure 2: Left lateral chest X-ray showed the opacity involved anterior, medial and posterior mediastinum.

Figure 3: Computerized Tomographic. Mix density mass (cystic and solid) involving 80% of the left hemithorax.
The ultrasound guided biopsy reported cytomorphology suggestive of epithelial neoplasia probable teratoma without exclude others germinal neoplasia or a thymoma. Before surgery, cardiology evaluation was reported as normal. Normal Alpha-fetoprotein and slight elevation of Beta human chorionic gonadotropin hormone (2.55 (<2mUl/ml)). We performed a posterolateral thoracotomy, finding a intrapleural mass of 25x10cm (Figure 4-6) in contact with the thymus, practicing a complete resection of the mass and the thymus was done, with minimal blood loss. The two initial postoperative days were in the ICU, with 60ml and 50ml drainage in the left chest tube per day. On day four the chest tube was removed, chest x ray showed a complete expansion of the lung (Figure 7). The patient discharged the hospital on the 7th day after surgery, in well general state. Pathology reported a neoplasm process with proliferation of epithelial cells, rounded by small lymphocytes and macrophages. No capsular invasion, concluding a thymoma B1.
Figure 4,5,6: Finding in thoracotomy. Intrapleural mass of 25x10cm in contact with the thymo.
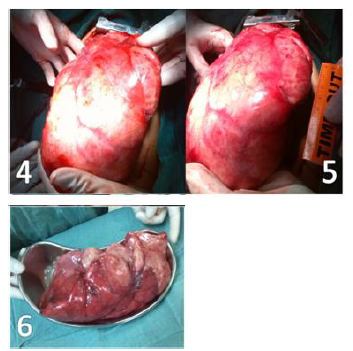
Figure 7: Posoperative chest x ray. Total reexpansion of the lung.

Discussion
Table 1. Health Organization histologic classification [15].
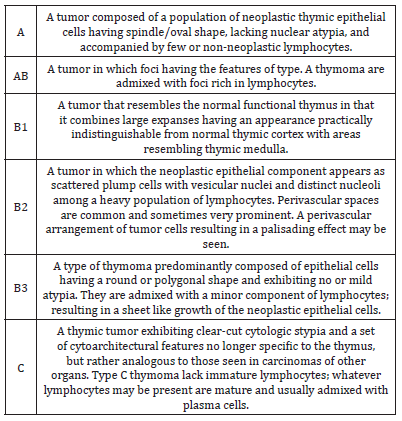
The mediastinum is demarcated by the pleural cavities laterally, the thoracic inlet superiorly, and the diaphragm inferiorly. It is further compartmentalized into anterior, middle, and posterior divisions based on structural landmarks seen on the lateral X ray. Even though two thirds of mediastinal tumors are benign, the mass location, patient age and the presence or absence of symptoms are the three factors that determine the likelihood of malignancy [2]. The masses in anterior compartment are more likely to be malignant. The presentation between the second and the fourth decade of life, is a predictor of malignancy. In addition, 85% of the patients with malignancy had a symptomatic presentation [2]. In the pediatric population the mediastinum is the most common location of the chest masses. Mediastinal masses are usually assigned to a single mediastinal compartment (based on the Fraser classification) to limit the differential diagnosis [1]. Thymic Neoplasm (TN), thymoma and thymic carcinoma, are rare, with an overall incidence of 0.13 per 100,000 person years [3]. Thymic carcinoma is much rarer than thymoma, with a five year survival rate of 40% [3]. Thymomas are the most common primary anterior mediastinal mass, with an incidence of 1.5 cases per million [3], but in children represent only 1-4% of mediastinal masses [4]. The thymoma preserve the thymus histological characteristics, on the other hand, the thymic carcinoma presents with anaplasia [5]. The World Health Organization (WHO), in 1999, proposed a consensus classification of the thymic epithelial tumor. These classification may help to determine if tumors can be treated by surgical resection only or if they require preoperative or postoperative adjuvant treatment [6]. The TN are now stratified into five thymomas entities Type A, AB, B1,B2, B3, and the more heterogenous group of thymic carcinoma (type C) [7,8] (Table 1). The thymomas are evaluated on the combined basis of the morphologic appearance of the neoplastic epithelial cells (spindle, oval, and so forth) and the relative number of these cell the non-neoplastic lymphocytes, representing a prognostic value [9]. Surgery is the gold standard of treatment [5]. Thymic tumors represent 1.5% of mediastinal masses in children [10]. Thymoma represents only 1-2% of mediastinal tumors in pediatric population. They are usually an incidental finding, but 40% debut as a paraneoplastic syndrome like myasthenia gravis. They are classified as noninvasive (well-defined) or invasive (those extending beyond its fibrous capsule) [1].
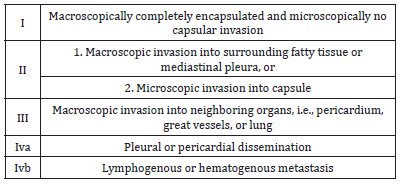
The thymoma, like the other mediastinal masses, are discovered incidentally on chest radiographs [11]. Usually they are assigned to a single mediastinal compartment limiting the differential diagnosis. The normal thymus appears on chest radiography as a prominent soft tissue density in the anterosuperior mediastinum of infants and toddlers. The most frequent radiographic appearance of thymoma is a variable sized, soft and lobulated tissue mass in the anterior mediastinum [11], this in the 45-80% of the patients [12]. With CT evaluation, thymomas are generally seen as a homogeneous, oval, rounded, or lobulated soft tissue masses, occasionally with areas of necrosis and hemorrhage, with well-defined contour, but it usually grows asymmetrically to one side [11,12]. A general consensus has been reached in the recent years that four factors play a role in the management and outcome of thymomas: the completeness of resection, the Masaoka stage, the WHO histologic classification and Myasthenia gravis [13]. The Masaoka Clinical stage is based in the grade of the tumor [7,14], and is the most important determinant of survival in the thymoma patients [9,15] (Table 2). Although 95% of thymomas could be classified using WHO criteria [15] most series agree that a survival decrement occurs when proceeding from A to B3 types, some authors argued that the slight survival difference between some subgroups, notably A and AB and B1 and B2, would justify a simpler classification into three histologic groups, A/AB, B1/B and B3 [13]. In others series, the WHO histologic classification reflects the oncologic behavior of thymoma. Types A and AB thymomas may be treated as benign tumors, and types B1 and B2 thymomas are the borderline between benign and malignant tumors. On the other hand, type B3 thymoma has a malignant behavior, and type C thymoma has more aggressive behavior as a cancer [15]. After the 1980s, Myasthenia gravis was no longer considered an adverse prognostic factor, and many reports agreed that thymoma patients with Myasthenia gravis have an equal or even better survival than those without it [13].
Table 2.Masaoka clinical staging system [15].
Thymolipoma is an unusual benign mediastinal mass composed of thymic and adipose tissue accounting in 2-9% of all thymic tumors [12]. There is no sex predilection, and the tumor occurs at any age but is more common in young adults [16]. They are lobulated, encapsulated tumors with large sizes. On chest X ray, a typically bulky, pendulous, teardrop-shape, radiolucent mass occupying the anterior inferior mediastinum can be observed. CT findings correspond to fat containing mass with strands, whorls, or rounded areas of soft tissue embedded in this fat. They usually contain equal amounts of fat and soft tissue. Although calcifications have been seen in histological examination of thymolipomas, it is unusual to visualize on radiologic examinations [12]. Surgical excision should be considered for patients with a gigantic intrathoracic lipomatous mass [16]. The literature available about the topic contain few case reports. Aydin et al. (2012) report a case of a 23 years old female patient, with a giant mass in the right hemithorax, practicing a total resection. Histopathological examination of the mass, report a stage IIA lipofibroadenoma, without recurrence in one year of follow-up [17].
Guimaraes [16] reported a 49-year-old man. A chest radiograph showed almost complete opacification of the right hemithorax, with a contralateral shift of mediastinal structures and inferior displacement of the right hemidiaphragm. CT scan demonstrated a large heterogeneous mediastinal lesion involvement of the anterior mediastinum and right hemithorax. The lesion was entirely resected, consisting in encapsulated fatty of 4.1kg. Microscopically 50% unremarkable mature adipose tissue and approximately 50% of normal thymic parenchyma. The patient was discharged 1 week later in excellent condition. No further therapy was given [18]. The others 3 case reports are of patients older than 50 years. Kitada [19] report a 50-year-old Japanese woman with a plaine chest x-ray showed a giant tumor shadow measuring 15×13cm in the right lower lung field, and chest computed tomography showed a solid tumor measuring 15×10×8cm in the right thoracic cavity. The mass (5x10x8cm, 430g) was resected. Histopathological diagnosis was a lymphocyte-predominant thymoma (type B1 thymoma). The postoperative course was good, and the patient has shown no evidence of recurrence as at the time of writing [19].
Limmer [18] report a 52-year-old man in who the posteroanterior and lateral chest X-ray revealed a huge circular dense mass obscuring the left lower hemithorax. Contrastenhanced multiplanar CT-scan of the thorax demonstrated a well-defined left intrathoracal mass. A CT-scan guided biopsy showed a mixed thymoma type AB. The team performed an anterolateral thoracotomy. On resection the tumor was completely encapsulated, according to Masaoka stage I. Histologically an organotypic thymic epithelial neoplasm was found with features of type A thymoma. The patient was discharged nine days after tumor resection. Radiotherapy was not indicated following complete resection of the well-encapsulated thymoma. Thirty six months postoperatively, the patient was well and asymptomatic and had no clinical evidence of recurrence [19]. Takenaka [20] report a case of a 61-year-old male presented with a Chest CT revealed a well enhanced giant mass, approximately 18cm in diameter in the right thoracic cavity. A surgical resection was performed finding A well-defined giant mass measuring 18×14.5×11cm was found in the right thoracic cavity. The histopathological findings indicated that the tumor was a type AB thymoma according to the World Health Organization classification and Masaoka stage IIB. The postoperative course was uneventful, and there has been no evidence of recurrence 6 months after the surgery [20]. This is a case of thymolipoma in children, a rare type of thymoma, that based in the case reports in adults have a good evolution after the surgical resection.
References
- Ranganath SH, Lee EY, Eisenberg RL, Ricardo R (2012) Mediastinal masses in children. AJR 198(3): 197-216.
- Duwe BV, Sterman DH, Musani AI (2005) Tumors of the mediastinum. Chest 128(4): 2893-2909.
- Rashid OM, Cassano AD, Tazabe K (2013) Thymic neoplasm: A rare disease with a complex clinical presentation. J Thorac Dis 5(2): 173-183.
- Wright CD (2009) Mediastinal tumors and cyst in the pediatric population. Thorac Surg Clin 19(1): 47-61.
- González R, Santolaya R, Jadue A, Rafael PM, Mordojovich GR, et al. (2012) Epithelial neoplasms of the thymus: Thymoma and thymic carcinoma. Characterization, treatment and variables associated with survival. Rev Chilena de Cirugía 64(6): 535-545.
- Jeong YJ, Lee KS, Kim J, Shim YM, Jungho H, et al. (2004) Does CT of thymic epithelial tumors enable us to differentiate histologic subtypes and predict prognosis? AJR 183(2): 283-289.
- Chen G, Marx A, Wen-Hu C, Jiang Y, Bernhard P, et al. (2002) New WHO histologic classification predicts prognosis of thymic epithelial tumors. Cancer 95(2): 420-429.
- Okumura M, Ohta M, Tateyama H, et al. The World Health Organization Histologic Classification System Reflects the Oncologic Behavior of Thymoma. CANCER 2002; 94(3): 624-632.
- Kim DJ, Yang WI, Choi SS, Kim KD, Chung KY (2005) Prognostic and clinical relevance of the World Health Organization schema for the classification of thymic epithelial tumors : a clinicopathologic study of 108 patients and literature review. Chest 127(3): 755-761.
- Yaris N, Nas Y, Cobanoglu U, Melek NY (2006) Thymic carcinoma in children. Pediatr Blood Cancer 47(2): 224-227.
- Franco A, Mody NS, Meza MP (2005) Imaging evaluation of pediatric mediastinal masses. Radiol Clin N Am 43(2): 325-353.
- Restrepo CS, Pandit M, Rojas IC, Villamil MA, Gordillo H, et al. (2005) Imaging findings of expansile lesions of the thymus. Curr Probl Diagn Radiol 34(1): 22-34.
- Ruffini E, Filosso PL, Mossetti C, Bruna MC, Novero D, et al. (2011) Thymoma: Inter-relationships among World Health Organization histology, masaoka staging and myasthenia gravis and their independent prognostic significance: A single-centre experience. European Journal of Cardio-thoracic 40(1): 146-153.
- Duhalde I, Jiménez LV, Carpio DP (2002) Timomas. About a clinical case. Cuad Cir 16(1): 58-63.
- Kondo K, Yoshizawa K, Tsuyuguchi M, Suguru K, Masayuki S, et al. (2004) WHO histologic classification is a prognostic indicator in thymoma. Ann Thorac Surg 77(4): 1183-1188.
- Guimaraes M, Benveniste MF, Bitencourt AG, Victor PA, Liliana PS, et al. (2013) Thymoma originating in a giant thymolipoma: A rare intrathoracic lesion. Ann Thorac Surg 96(3): 1083-1085.
- Aydin Y, Sipal S, Celik M, Omer A, Ulas AB, et al. (2012) A rare thymoma type presenting as a giant intrathoracic tumor: Lipofibroadenoma. Eurasian J Med 44(3): 176-178.
- Limmer S, Merz H, Kujath P (2010) Giant thymoma in the anterior-inferior mediastinum. Interactive Cardio Vascular and Thoracic Surgery 10(3): 451-453.
- Kitada M, Sato K, Matsuda Y, Satoshi H, Yoshihiko T (2011) Ectopic thymoma presenting as a giant intrathoracic tumor: A case report. World Journal of Surgical Oncology 9:
- Takenaka T, Ishida T, Handa Y, Shinichi T, Hiroyuki M (2012) Ectopic thymoma presenting as a giant intrathoracic mass: A Case Report. Journal of Cardiothoracic Surgery 7: 68.
© 2021 Allan Delcid. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






