- Submissions

Full Text
Surgical Medicine Open Access Journal
Postoperative Complications in Thyroidectomy Performed at Hospital Escuela Universitario and Hospital General San Felipe, Tegucigalpa MDC in 2018
Rosales FES* and Bueso HES
Department of Surgeon General, USA
*Corresponding author: Rosales FES, Department of Surgeon General, USA
Submission: July 14, 2021Published: August 18, 2021

ISSN 2578-0379 Volume4 Issue3
Abstract
Introduction: Specific complications of thyroid surgery include injury to the recurrent laryngeal nerve and the parathyroid glands, without being exempt from other complications such as infection of the surgical site, bleeding, surgical wound dehiscence, and others.
Methods: The present study is retrospective observational and aims to analyze the condition of thyroid surgery in the country, specifically in state hospitals in Tegucigalpa, its rate of complications and its relationship with associated factors before the procedure.
Result: A total of 92 patients undergoing thyroid surgery were studied at the Hospital Escuela and Hospital General San Felipe by reviewing the clinical record. The preoperative status, comorbidities and the surgical procedure performed were recorded and were related to the main complications mentioned above.
Conclusion: A global rate of complications related to laryngeal nerve injury of 15% and late hypocalcemia of 7% was found, which are higher than the incidences reported in international series, however these vary from 0% of recurrent laryngeal nerve injury in thyroidectomies subtotal up to 22% in radical dissections in patients with neo proliferative processes.
Keywords: Hypocalcemia; Parathyroid; Surgical complications; Thyroid; Thyroidectomy
Introduction
Postoperative complications in thyroid surgery constitute an important cause of morbidity in patients undergoing these procedures. Although the complication rates in international series are low, the associated morbidity and hospital costs justify their study [1]. Recurrent laryngeal nerve injuries and symptomatic hypocalcemia are the main complications inherent to thyroid surgery and these are associated with multiple factors specific to the patient and their pathology, as well as events related to the surgical procedure. In Honduras there are few studies related to thyroid disease and none studying their specific postoperative complications. The purpose of this study is to provide information on the status of endocrine surgery in the country and specifically on thyroid surgery and relate it to the global rates of postoperative complications [2]. Having an initial diagnosis will provide the option to planning and management of efforts to reduce the rate of postoperative complications in thyroid surgery. This study provides useful information for administrative decision making, implementation of management policies and protocols, benefiting the population served, and the institutions involved in an attempt to identify predisposing characteristics of postoperative complications [3].
Methodology
A review of the clinical records of patients who had undergone thyroid surgery was
carried out. Preoperative studies were compiled establishing thyroid function status and
calcium metabolism, determining levels of thyroid hormones, albumin, calcium, vitamin D,
thyroglobulin, albumin, thyroglobulin and levels of parathyroid hormone. Vocal cord function
was verified by preoperative nasofibroscopy. The existence of comorbidities and associated conditions such as the presence of goiter, and other associated
pathologies were verified. The suspicion or diagnosis of thyroid
cancer was determined through the use of ultrasonography, fine
needle aspiration biopsy or other diagnostic techniques such as CT,
scintigraphy and or magnetic resonance imaging [4-7].
A review was made of the surgical indication, the surgical
technique used, the operative findings, the visualization and
identification of structures of interest, intraoperative complications
and the biopsy result. The control measurements of thyroid
metabolism, calcium and the existence or not of complications
typical of the procedure in the immediate postoperative period and
the control carried out in the outpatient clinic were verified [8].
Symptomatic hypocalcemia was identified using serum calcium
reference values according to the laboratory used associated with
hypocalcemia symptoms such as tetany, cramps and / or paresthesia
and the need for intravenous calcium replacement administration.
Laryngeal nerve injury was identified with recurrent laryngeal nerve
palsy with its clinical manifestations. General data information,
admission diagnosis, procedure performed, postoperative evolution
notes and subsequent evaluations in the consultation are essential
for data processing [9-11].
Result
A total of 92 cases of patients who underwent thyroidectomy
in 2018 were studied, 30 at Hospital Escuela and 62 at Hospital
General San Felipe. In this study, 95% of the patients were women,
while 5% were male. More than a third of the patients were older
than 60 years (Table 1); [12].
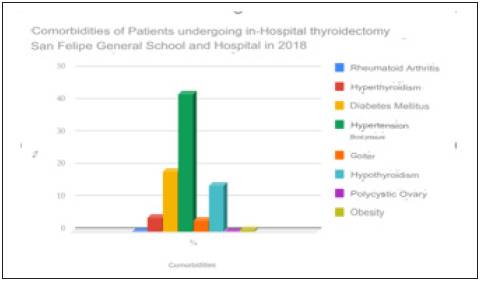
Regarding the origin, 71.43% of the cases lived in an urban
area, and 28.57% of the cases studied came from rural areas of
the country. Regarding the personal pathological antecedents
found in the patients of this study. Hypertension was present in
42% of the study participants, followed by obesity and diabetes
mellitus with 25% and 18% respectively [13]. Note that because
there are patients with multiple comorbidities, the sum of all the
percentages exceeds 100%. Tables [2-4] show the complication
index, of transient and permanent hypocalcemia, and recurrent
laryngeal nerve injury, respectively. The distribution by admission
diagnoses was made and a comparison was made with the
definitive postoperative histological diagnosis [14]. It is observed
that 11% of the patients with negative pathology presented
mediate hypocalcemia while 30% of the patients with positive
pathology due to malignancy presented transient hypocalcemia.
14% of the patients with a positive biopsy result for malignancy
presented permanent hypocalcemia. Only 4% of the patients
undergoing thyroidectomy with a negative pathological anatomy
result had some type of recurrent laryngeal nerve injury (Figure 1);
[15-18]. Tables 5 & 6 show the incidence of transient, permanent
hypocalcemia and recurrent laryngeal nerve injury according to
the surgical procedure performed [19]. It can be seen that subtotal
thyroidectomy had 0% complications, total thyroidectomy had 20%
and 6% transient and permanent hypocalcemia respectively. Total
thyroidectomy has 15% recurrent laryngeal nerve injury, while
when radical dissection was performed, 21% of patients developed
unilateral or bilateral recurrent laryngeal nerve injury [20].
Figure 1: Comorbidities of patients undergoing thyroidectomy at Hospital Escuela and Hospital General San Felipe in 2018.
A significant percentage of the laboratory studies under study were not performed or were not recorded in the clinical record. Figure 2 shows that only T4 was performed in 100% of the cases and that Albumin, Calcium, Vitamin D and Parathyroid hormone were not performed in more than 50% of the cases. Similarly, preoperative and postoperative laryngoscopy was performed only in 1% and 24% respectively, thus making a complete analysis of the collected data impossible [21-23].
Figure 2: Laboratory studies performed in post-operative thyroidectomy patients at Hospital General San Felipe and Hospital Escuela in 2018. N: 92.
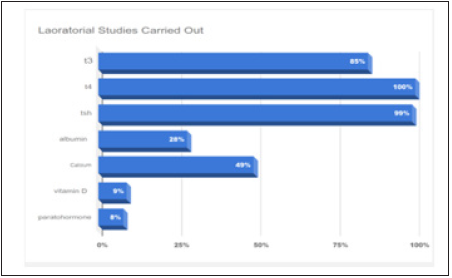
Table 1. Age distribution in post-thyroidectomy patients at Hospital General San Felipe and Hospital Escuela in 2018. N: 92.
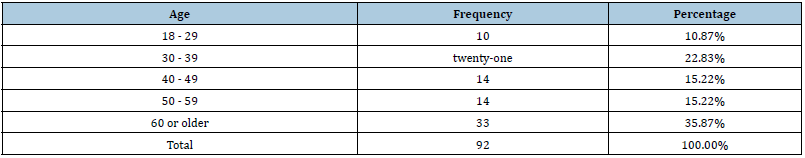
Table 2. Transient hypocalcemia according to admission diagnosis in post-operated thyroidectomy patients at Hospital General San Felipe and Hospital Escuela in 2018. N: 92.
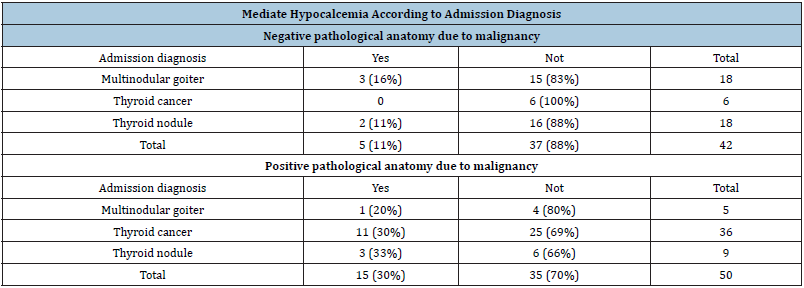
Table 3. Permanent hypocalcemia according to admission diagnosis in post-operated thyroidectomy patients at Hospital General San Felipe and Hospital Escuela in 2018. N: 92.
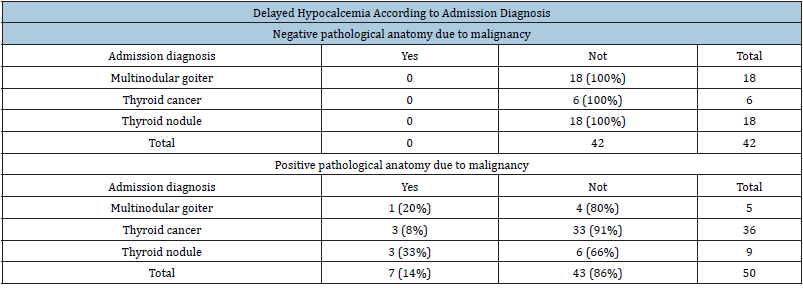
Table 4. Laryngeal nerve injury according to admission diagnosis in post-operated thyroidectomy patients at Hospital General San Felipe and Hospital Escuela in 2018. N: 92.
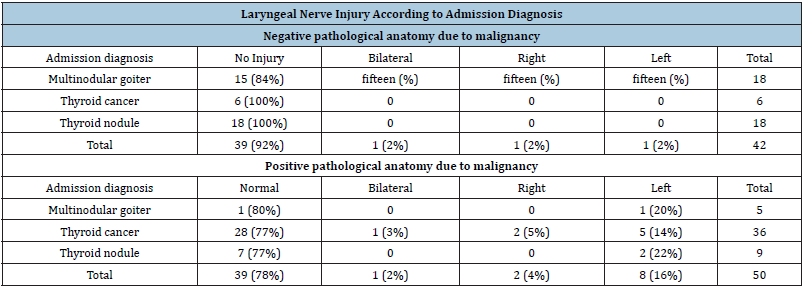
Table 5. Hypocalcemia according to procedure performed in post thyroidectomy patients at Hospital General San Felipe and Hospital Escuela in 2018. N: 92.
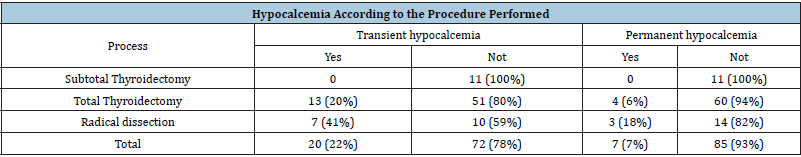
Table 6. Recurrent laryngeal nerve injury according to Procedure Performed in post-operated thyroidectomy patients at Hospital General San Felipe and Hospital Escuela in 2018. N: 92.

Discussion
In the present study, 92 clinical records of patients undergoing
thyroid surgery at Hospital Escuela and Hospital General San Felipe
in 2018 were analyzed. The indications for surgery were multiple,
including thyroid nodules, goiter, cancer, among others, and the
procedures varied according to the etiology ranging from subtotal
thyroidectomies to radical neck dissections [24].
The sociodemographic distribution has a marked inclination
since the majority of patients studied are women in 98.39%
compared to the male sex, representing only 1.61% of the total
sample. The age distribution shows that the patients treated for
thyroid disease are, for the most part, elderly, since 50% of the
sample is over 50 years of age. 71% of the patients studied came
from urban areas. The profile of a patient undergoing thyroid
surgery at the Hospital Escuela y Hospital General San Felipe is an
elderly woman from an urban area.
Comorbid states have a decisive influence on the diagnosis
and treatment of thyroid disease, be it medical or surgical. In our
study, the main pathologies found were recorded in which arterial
hypertension was predominant, since 58.06% of the patients in
the study were hypertensive, diabetes mellitus is found in 18% of
patients. These, although it is true, do not directly affect the thyroid
pathology, they condition and limit the surgical action since it
increases the index of trans and postoperative bleeding as well as
alters the subsequent inflammatory process. It was found that 3%
of the sample had hyperthyroidism and hypothyroidism in 14.52
[25].
The main complications were related to the admission diagnosis
of each patient, and later it was separated into 2 groups. The first
was the one in which, regardless of their admission diagnosis, they
obtained a negative pathological study for malignancy, and the
second group those in which the pathological study was positive
for malignancy. The first data that is pertinent to note is that not
all cases admitted with a diagnosis of thyroid cancer have positive
biopsies for malignancy in the postoperative period. Of the patients
admitted with a diagnosis of thyroid cancer, 6 obtained a negative
biopsy due to malignancy, these cases represent a false positive.
Hypocalcemia is a complication that can occur mediate and
be temporary in most cases or be permanent. It is said that it is
permanent hypocalcemia when there is serum hypocalcemia
associated with its symptoms, it is generally worth calcium intake.
The patients who were admitted with a diagnosis of multinodular
goiter were the ones who showed the most hypocalcemia in a
mediate and transitory way (16%), since it was not necessary
to continue the therapy for more than 6 months in the follow-up
visits. None of the patients with a diagnosis of thyroid cancer on
admission and negative postoperative biopsies showed transient
hypocalcemia [26,27].
Regarding permanent hypocalcemia, none of the patients with
negative postoperative biopsies showed permanent hypocalcemia,
even those admitted with a diagnosis of thyroid cancer 7 of the
patients studied showed permanent hypocalcemia, all of them with
postoperative biopsies positive for malignancy, this represents 7%
of the total sample and 14% of the patients with postoperative
biopsies positive for malignancy [28].
Hypocalcemia can manifest as a complication due to the
complexity of the surgical procedure or due to a distorted anatomy.
This is reflected in the data obtained, since none of the patients who
underwent subtotal thyroidectomy suffered from hypocalcemia,
only 6% of those who underwent total thyroidectomy, and 18%
of the patients who underwent radical dissection had permanent
hypocalcemia. Likewise, we observed that no injury to the RLN was
found in the subtotal thyroidectomies, however, 16% of the RLN
injury was observed in the total thyroidectomies and 24% of the
radical dissections, which means that 1 in 4 patients underwent
Radical neck dissection due to surgical pathology presents a degree
of injury to the RLN. It was also shown that bilateral RLN lesions
are more frequent in neck dissection, with 5% in dissections vs 2%
in total thyroidectomies. This shows the highest complication rate
according to the complexity of the procedure [29].
Patients with a positive pathological anatomy due to
malignancy, it should be noted that this procedure prevailed in all
surgical interventions in 80.65% of the cases, 5% of the cases with
admission diagnosis of thyroid cancer and a confirmatory diagnosis
of malignancy presented bilateral paralysis. of the vocal cords, in
addition 5% of the cases presented paralysis of the left vocal
cord, with regard to thyroid nodule, the absence of post-surgical
laryngoscopy prevailed in 77.78% and 22.22% presented paralysis
of the left vocal cord, already taking the issue of multinodular goiter,
50% of the cases presented paralysis of the left vocal cord and 50%
were reported as normal.
It was evidenced that the patients under study were not
carried out with the preoperative study profile recommended
by the international literature. One of the most alarming indices
is the percentage of laryngoscopies performed, since they
were performed only in 1% of the cases evaluated. Likewise, it
was observed that the levels of parathyroid hormone, calcium,
vitamin D and thyroglobulin were not adequately evaluated in
the preoperative period. This is relevant since, as it does not
have a preoperative parameter, it will not be possible to discern
between a postoperative complication and an alteration in calcium
metabolism or in RLN dysfunction prior to the surgical procedure.
Also, having a complete preoperative profile could easily identify
patients at higher risk of postoperative complications [30]. It is
clear that the difficulty in completing the ideal preoperative studies
has a multifactorial origin, but the economic factor plays a large
role in this. Both the Hospital Escuela and the Hospital General San
Felipe are state institutions with limited financial resources and the
patients treated in these centers are, for the most part, incapable
of performing studies such as laryngoscopies, tomographies, and
special tests in private centers.
Conclusion
The profile of a patient undergoing thyroid surgery at the
Hospital Escuela y Hospital General San Felipe is an elderly female
patient from an urban area, which predisposes the presence of
associated pathologies and comorbid conditions that condition the
presentation and evolution of the disease. surgical thyroid disease.
The main comorbidities present in patients undergoing
thyroidectomy are hypertension, obesity, and diabetes mellitus. Of
the total of patients studied, 20% presented transient hypocalcemia,
7% presented permanent hypocalcemia and 15% presented a
degree of recurrent laryngeal nerve injury. The patients most at risk
of presenting postoperative complications in thyroidectomy are
those with malignant neoplastic pathology in whom radical neck
dissection is performed [31].
Gratitude
Thanks to our parents, for being the main promoters of our dreams, for trusting and believing in our expectations, for the advice, values and principles that they have instilled in us.
References
- Thyroid gland surgery josé luis pardal-refoyo sacyl. Zamora Healthcare Complex. Otolaryngology Service. Zamora, Spain.
- Sosa MG, Ernand RS (2016) Thyroidectomy at "Calixto García" general hospital. Cuban Journal of Surgery.
- Pizarro FI (2013) Thyroid and goiter: Historical evolution and its great characters default. Rev Medica Condes.
- (2017) Sociodemographic and epidemiological characterization of the most frequent neoplasms attended at Hospital Escuela Universitario, Honduras. Champion Federico Mendoza Talavera 13(1): 1.
- Vasquez SP, Mendoza RZ (2003) Fine needle aspiration biopsy of the thyroid in the teaching hospital: Evaluation of its diagnostic accuracy as a screening test. Rev Med Post Unah 8(25).
- Eduardo Núñez, Luis Munguí Surgical approach of thyroid nodules with follicular lesion of undetermined significance. Surgical approach to thyroid nodules with follicular lesion of undetermined significance.
- Flores OR (1992) Combined surgery in thyroid cancer. Honduran Medical Journal 60.
- Paguada DAO (1987) Surgical thyroid pathology, incidence, treatment modality and complications at leonardo hospital martinez valenzuela in the period from 1981-1987.
- Fernández M (2015) Pathology and surgery of the thyroid and parathyroid glands official presentation of the Spanish society of otorhinolaryngology and cervico-facial pathology 2015.
- Skandalakis J (2015) Surgery foundations of surgical anatomy 2015.
- Sanabria A, Chala A, Ramírez A, Álvarez A (2014) Cervical surgical anatomy of importance in thyroid surgery. Rev Colomb Cir 29: 50-58.
- Henry BM, Sanna B, Vikse J, Graves MJ, Spulber A, et al. (2017) Zuckerkandl's tubercle and its relationship to the recurrent laryngeal nerve: A cadaveric dissection and meta-analysis. Auris Nasus Larynx 44(6): 639-647.
- Rojas M, Quijano Y, Miguel R, Bernal L (2016) Anatomical variations of the recurrent laryngeal nerve in a Colombian population sample recurrent laryngeal nerve in a sample of the Colombian population. Rev Fac Med 64(2): 207-213.
- Toda FILL, Salas MMV (2017) Thyroid pathology update. In: Aepap (Edr.), Pediatrics Update Course pp. 161-174.
- Fernandez M (2015) Official presentation of the Spanish society of otorhinolaryngology and cervico-facial pathology 2015. Pathology and Surgery of the Thyroid and Parathyroid Glands.
- Garcia G (2016) Thyroid physiology. Med Int Mex 32(5): 569-575.
- Ortega PR, Urra AB, Compan AJ (2011) Clinical experience in total thyroidectomy. Rev Otorrinolaringol Cir Head Neck 71: 53-56.
- Joliat GR, Guarnero V, Demartines AN, Schweizer V, Matter M (2017) Recurrent laryngeal nerve injury after thyroid and parathyroid surgery incidence and postoperative evolution assessment. Medicine 96(17): e6674.
- Jiang Y, Gao B, Zhang X, Zhao J, Chen J, et al. (2014) Prevention and treatment of recurrent laryngeal nerve injury in thyroid surgery. Int J Clin Exp Med 7(1): 101-107.
- García JA, Calderón J, Zarza VV, Velarde MC, Rodríguez MD. The neuromonitoring in cervical endocrine surgery. Detection and Intraoperative Prevention of Laryngeal Paralysis.
- Jeannon JP, Orabi JP, Bruch GA, Abdalsalam HA, Simo R (2009) Diagnosis of recurrent laryngeal nerve palsy after thyroidectomy: A systematic review. Int J Clin Pract 63(4): 624-629.
- Bello AM, Real PR, García MAR (2014) Postoperative morbidity in patients undergoing thyroidectomy at the general hospital of Acapulco. Three years of experience. Elsevier Cir Gen 3(2): 91-95.
- Paek SH, Kang KH, Park SJ (2018) A comparison of robotic versus open thyroidectomy for papillary thyroid cancer. Surg Laparosc Endosc Percutan.
- Thyroidectomy without cervical incision by endoscopic approach biaxyl-biareolar. First impressions after its introduction in a specialized unit. Literature Review. Mount Sinai Hospital, New York, Ny, USA.
- Gordillo VR, Vásquez WI, Andrade CA (2017) Thyroidectomy transoral endoscopic by vestibular approach (Toetva): Report of the first human case in Latin America. Hospital del Instituto Ecuatoriano de Seguridad Social (Iess), Ibarra, Ecuador. Rev Chil Cir 69(1): 60-64.
- Tae K, Ji YB, Cho SH, Lee SH, Kim DS, et al. (2012) Early surgical outcomes of robotic thyroidectomy by a gasless unilateral axillo-breast or axillary approach for papillary thyroid carcinoma: 2 years' experience. Head Neck 34(5): 617-625.
- Benhidjeb T, Wilhelm T, Harlaar J, Kleinrensink GJ, Schneider TAJ, et al. (2009) Natural orifice surgery on thyroid gland: Totally transoral video-assisted thyroidectomy (Tovat): Report of first experimental results of a new surgical method. Surg Endosc 23(5): 1119-1120.
- Refoyo JLP (2012) Utility of neuromonitoring in thyroid surgery. Acta Otorrinolaringol Esp 63(5): 355-363.
- Nuño P, Montañez JB, Carrasco CR, Negrín AP (2002) Immediate postoperative period in patients undergoing total thyroidectomy in ICU. Enferm Intensiva 13(2): 78-84.
- Edafe O, Antakia R, Laskar N, Uttley L, Balasubramanian SP (2014) Systematic review and meta-analysis of predictors of post-thyroidectomy hypocalcemia. Br J Surg 101(4): 307-320.
- Espino CP, Já RB, Caselles AM, González SJ, Pavía GA, et al. (2018) Use of the value of intact parathyroid hormone on the first postoperative day after total thyroidectomy as a predictor of permanent hypoparathyroidism. Endocrinol Diabetes Nutr.
© 2021 Allan Fernando DM. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






