- Submissions

Full Text
Surgical Medicine Open Access Journal
Pelvi-Acetabular Fixations_ My Worst-Case Scenarios and Lessons Learnt
Rakesh Bhargava*
Department of Tuberculosis and chest diseases, India
*Corresponding author: Rakesh Bhargava, Department of Tuberculosis and chest diseases, Aligarh, India
Submission: September 18, 2019;Published: October 04, 2019

ISSN 2578-0379 Volume3 Issue1
Abstract
Pelvi-aetabular fixation is often complex and perilous. Some iatrogenic decisions or lack of them compounds the situation, posing great difficulties for the surgeon and poor outcomes for the patient.
Learning by hindsight is what constitutes experience. Acknowledging your mistakes, though often tough, should not involve reluctance, and lessons learnt need to be passed on.
Figure 1:X-ray showing # both rami, # floor acetabulum, large fragment post. Lip and post dislocation.

Introduction
The first Pelvi-acetabular fixation workshop in India was organized by Synthes at the Taj, Mumbai quite a few years ago, and I happened to attend. It was a fascinating subject and petty absorbing. Coming back after the workshop, I realized two hurdles at my Government Medical college institution. There would be no funds to purchase the set of instruments, and Synthes at that time was not into lending out the instrument sets even if you were buying their implants. The alternative was to make do with Indian implants and local instrument sets. These included the bare essential forceps. There was no bending press for the implants, so essential as there were no pre-bent plates. Screw sets were grossly inadequate and deficient, all of which I was to realize to my chagrin.
Case I
The case I had taken up was a 17-year-old boy with # dislocation hip in road accident He had a Type IV (Thompson-Epstein) injury and was hemodynamically unstable. My first mistake was to wait for the reduction to stabilize, resulting in a fixation delay of 12 days. First principle of pelvi-acetbular fixation is to operate as early as possible preferably within seven days. Any delay beyond ten days may spell havoc for the surgeon and the patient (Figure 1). It is well-nigh impossible to achieve a good reduction, more so without proper instrumentation or with an incomplete set. The local suppliers of instrument sets and implants make do with locally made copies of the instruments and the least number in the set they can get away with Consequently, all you may get in the set is two reduction clamps and a Kings clamp and a set of plate benders (Figure 2).
Figure 1:X-ray showing # both rami, # floor acetabulum, large fragment post. Lip and post dislocation.

Figure 2:Consequently, all you may get in the set is two reduction clamps and a Kings clamp and a set of plate benders.

Second lesson I learned on the table was not to operate without a full set of instruments and implants. I tried to do the best I could. Post operation x-rays showing the fixation and grafted area (Figure 3). The defect between the fractured ends was bone grafted, and after 17 months it was fully integrated, and defect bridged (Figure 4). The patient could squat and sit crosslegged, so important to the Indian patient but not fully (Figure 5). Remember a compromised reduction and fixation cannot give a perfect result, may possibly just yields a satisfactory result, to the patient that is Lessons I learnt were to work with complete set of instruments and implants and not compromise with the ‘just adequate’. Operate to fix early, do not procastinate, especially for reasons of apprehension about self capability.Refer the paient timely. In fracture-dislocations, fix in situ even with slightly displaced fragments. Functional end results may be pretty good except for some shortening. Complication to watch for is AVN.
Figure 3:Post operation x-rays showing the fixation and grafted area.
Figure 4:The defect between the fractured ends was bone grafted, and after 17 months it was fully integrated, and defect bridged.
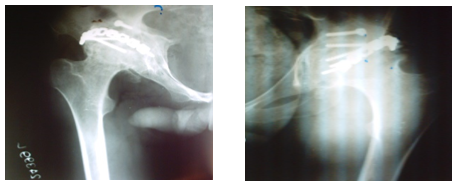
Figure 5:The patient could squat and sit cross legged, so important to the Indian patient but not fully.

Case II
The case II is an 18-year-old girl with poly-trauma in a roadside accident Her multiple injuries included fracture mandible, injury to pelvis and left hip, transcervical fracture neck femur and both column fracture acetabulum (Figure 6) showing the CT scan and #D reconstruct images the mandible was wired by plastic surgeon. I fixed the fracture neck femur with two cancellous screws after reduction under vision. Subsequently I fixed the anterior column with a long cancellous screw obliquely from roof of acetabulum to pubic ramus and fixed the anterior superior iliac spine and adjacent ilium with a cortical screw. Lastly, I fixed the posterior column with a plate and screws (Figure 7) show the post-op radiological images with the affected limb in external and internal rotation to assess the fixation of the transcervical fracture neck of femur and the size of the cannulated screws (Figure 8) focus on the radiological images of the fractures of the acetabulum One year after the surgery, the neck fixation implants were partially removed (Figure 9) All implants were removed two and a half years after surgery (Figure 10).
Figure 6:Showing the CT scan and #D reconstruct images.
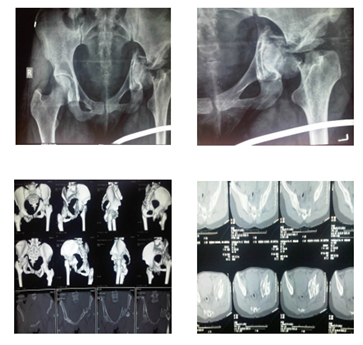
Figure 7:Show the post-op radiological images with the affected limb in external and internal rotation to assess the fixation of the transcervical fracture neck of femur and the size of the cannulated screws.

Figure 8:Focus on the radiological images of the fractures of the acetabulum.
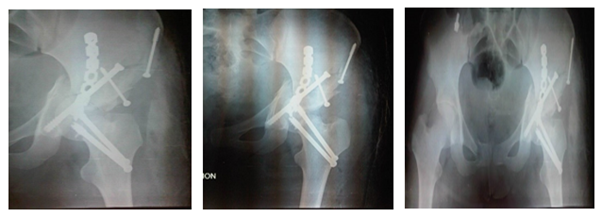
Figure 9:One year after the surgery, the neck fixation implants were partially removed.
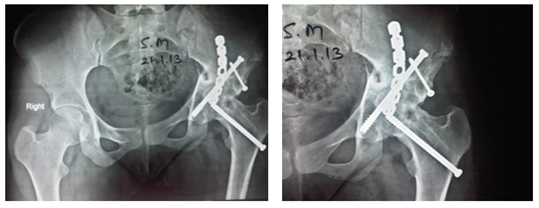
Figure 10:All implants were removed two and a half years after surgery.
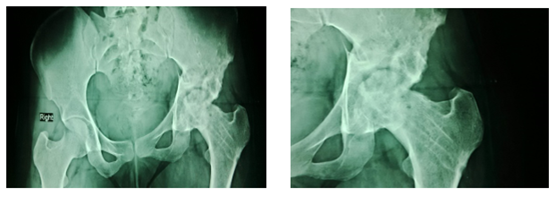
The girl belonged to a community where marriages take place early and she was married shortly after. She has now been married for five years and though she has no issue as yet, she has no complaints, can do her housework and perform her daily duties. She can squat and sit cross-legged and as yet has no symptoms of avascular necrosis of femur. Although AVN of femoral head develops within two years of injury if it has to, but I am keeping my fingers crossed as time is not a deterrent to AVN. Moral of this story is in polytrauma, ideal may not be possible. In an effort to achieve the best, one may lose the chance to do the achievable. The difference in cost may sometimes be the life of the patient. More implant doesn’t necessarily mean better fixation. Leave somethings to nature and it will oblige [1-3].
References
- Soloman L, David W, Selvadurai N (2014) Apley's System of Orthopedics and Fractures (9th edn), London, pp. 844.
- (2006) SPS Matta Pelvic System: Stryker Trauma Ag Bohnackerweg. Altreu, Switzerland.
- Pelvic ring and acetabulum. In: Chris C, Steve K, Joseph S, Peter T, Michael B, et al. (Eds.), AO surgery Reference, AO Foundation, Switzerland.
© 2019 Jameel Ali. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






