- Submissions

Full Text
Surgical Medicine Open Access Journal
Protocol Based on Vital Capacity Influences the Functional Capacity in Patients Submitted to Cardiac Surgery
André Luiz Lisboa Cordeiro1*, Nassany Marilyn Amorim2, Hayssa de Cássia Mascarenhas Barbosa2, Simone Bacciotti Campodonio3, Emilly Alves Dias3, Adeilton Santos Santana Junior3, Sheila Christian Bastos de Souza3, André Raimundo Guimarães4 and Jefferson Petto5
1 Medicine and Human Health at the Bahia School of Medicine and Public Health, Bahia Faculty of Noble Faculty, Brazil
2 Faculty of Noble Faculty, Brazil
3 Personners of the Research League in Cardiopulmonary Physiotherapy, Brazil
4 Cardiac surgeon of the Noble Institute of Cardiology, Santa Casa de Misericórdia, Brazil/p>
5 Medicine and Human Health at the Bahia School of Medicine and Public Health, Brazil
*Corresponding author:André Luiz Lisboa Cordeiro, Medicine and Human Health at the Bahia School of Medicine and Public Health, Salvador, Bahia Faculty of Noble Faculty, Feira de Santana, Bahia, Brazil
Submission: June 21, 2018Published: September 17, 2018

ISSN 2578-0379 Volume2 Issue2
Abstract
Introduction: Respiratory functional assessment is of paramount importance, since it estimates and monitors the behavior of lung volumes and capacities, especially vital capacity (CV), which is frequently reduced in patients undergoing cardiac surgery.
Objective: To evaluate the impact of a physiotherapeutic protocol based on CV on the functional capacity in patients in the postoperative period (PO) of CC.
Methods: This is a randomized, controlled clinical trial. The patients were divided into two groups: control group (CG) was conducted according to the unit routines, while the intervention group (GI) underwent a pulmonary expansion protocol based on CV. In addition, a six-minute walk test (6MWT) was performed to assess functional capacity.
Result: The final sample consisted of 40 patients (20 in each group), 26 men (65%) and mean age 53±16 years. CV on the day of hospital discharge was significantly higher in GI (36.04±6.03 vs 30.83±7.5ml/kg, p=0.01), and the same CV behavior was observed in the day Of hospital discharge (25.9±9.5 vs 36.0±6.0ml/kg, p< 0.001). Regarding the 6MWT at hospital discharge, the GC ranged 413±90 meters versus 486±116 meters (p=0.03).
Conclusion: A CV-based pulmonary expansion protocol is associated with a significant increase in functional capacity in patients undergoing cardiac surgery.
Keywords: Vital Capacity; Functionality; Cardiac surgery
Introduction
Cardiac surgery (CS) is a highly complex procedure that can generate several postoperative changes. With the technological advance, the surgical procedure became the most advanced stage of the treatment of diseases of the cardiovascular system [1]. In 2008, 10,652 surgeries of myocardial revascularization and/ or valve replacement were performed during the period from January to June in Brazil [2]. Even with all technological advances that aim to increase and prolong the quality of life of patients undergoing this surgery, this procedure continues to favor the development of alterations in lung function [3].
Several factors may influence respiratory mechanics and gas exchange in CS, increasing the risk of pulmonary complications, such as obesity, chronic obstructive pulmonary disease, pulmonary congestion, smoking habit and heart failure [4]. The alveolar collapse resulting from the reduction of pulmonary volumes and capacities is the main respiratory complication observed in postoperative patients of thoracic and abdominal surgeries [5].
The physiotherapeutic resources for pulmonary expansion in this profile of patients are aimed at reducing the volume loss, with consequent reduction of functional residual capacity (FRC), which can lead to hypoxemia and increase in the risk of infections and lung injury, if not reversed [6]. The vital capacity (VC) is an important functional marker in patients submitted to CS, demonstrating the pulmonary function behavior and guiding the design of the physiotherapeutic protocols.
Respiratory physiotherapy has been widely used in postoperative CS due to the benefits of pulmonary expansion therapy (PET), including earlier restoration of VC and other indexes related to pulmonary function. Among the main techniques and resources used in PETwe highlight the ventilatory patterns, positive end-expiratory pressure (PEEP) and incentive spirometry [5].
In a study conducted by Leguisamo et al. [7] 86 individuals who performed PET observed that patients who in the preoperative pe riod applied a protocol of guidelines on respiratory physiotherapy and for 15 days exercises such as diaphragmatic, a significantly shorter hospital stay compared to individuals who were only advised one day before surgery.
Therefore, the objective of the present study was to evaluate the impact on the vital capacity and functional capacity of a protocol of Pulmonary Expansion Therapy in patients undergoing cardiac surgery.
Materials and Methods
This is a randomized, controlled clinical study in patients undergoing cardiac surgery at the Instituto Nobre de Cardiologia. It was submitted and approved by the Research Ethics Committee of the Faculdade Nobre in Feira de Santana-Bahia. Patients who underwent elective cardiac surgery (myocardial revascularization, aortic or mitral valve replacement, and correction of inter-atrial communication) were included via sternotomy and extracorporeal circulation, over 18 years of age and of both sexs.
Patients with hemodynamic instability at the time of the measurements, history of previous CS, difficulty in understanding or performing physical therapy measures and/or behaviors, those who underwent noninvasive ventilation for more than 24hours after admission to the ICU, were excluded. Were hospitalized in the ICU for more than 4 days, with functional limitation to perform the walk test, with ventilatory disturbance to spirometry performed in the preoperative period and who did not agree to sign the Free and Informed Consent Term.
In the preoperative period all the patients performed an evaluation of the functional capacity through the Six-Minute Walk Test (6MWT). According to the American Thoracic Society (ATS) the test must be performed in a corridor with 30 meters, flat and totally free of obstacles. Before the test, blood pressure, pulse oximetry, level of dyspnea (Borg scale), heart rate and respiratory rate were analyzed. The patient was advised to walk as fast as possible, without running, walking in this corridor for a time of six minutes. After the test, the patient sat down and the vital signs were again evaluated.
All patients received general anesthesia and the surgical procedure was performed with extracorporeal circulation via median sternotomy. On admission to the ICU, patients were submitted to mechanical ventilation with a tidal volume of 6 to 8ml/kg of predicted weight, Positive End-expiratory Pressure (PEEP) of 5cm H2O, respiratory rate programmed to maintain the partial pressure of carbon dioxide in arterial blood between 35 to 45mmHg and Inspired Oxygen Fraction required to maintain Peripheral Oxygen Saturation above 92%. After extubation, the patients were followed up and submitted to standard procedures, according to the norms and routines of the unit, without the intervention of the researchers.
After discharge from the ICU, the patients were randomly divided into two groups: control group (CG) or intervention group (IG). The CG received conventional treatment of the unit, which consists of reexpansive ventilatory patterns (maximal and sustained inspiratory and fractional inspiration), diaphragmatic stimulation, active kinesiotherapy, ambulation and cycloergometer for lower limbs. These individuals had the VC evaluated on the first day after discharge from the ICU and on the day of hospital discharge. For VC measurement, patients were seated in the armchair, the patient was asked to take a deep breath, close to the total lung capacity, followed by a maximal and slow expiration until near the residual volume, through a facial mask Connected to the Wright Mark 8 analogue ventilator (Ferraris), with a 35mm display, two 0-1l/min and 0-100l/min dials. Three measurements were taken, with a one minute interval between them, adopting as reference, the highest value obtained.
The IG was submitted to Pulmonary Expansion Therapy based on the daily VC value using the following criteria: when a CV< 15ml/ kg was obtained continuous positive airway pressure (CPAP 15cm H20); When the VC was between 15 and 20ml/kg, positive pressure was used at the end of expiration (EPAP 15 cm H20); For a VC between 20 and 30ml/kg flow stimulation spirometry was used; And when a VC >30ml/kg was observed, deep breathing exercises were performed. The VC was evaluated daily until the day of hospital discharge, and the physiotherapeutic intervention was maintained or modified according to the value of this variable. In addition to these conducts, kinesiotherapy, ambulation and cycle ergometry were performed for MMII.
On the day of hospital discharge, all patients underwent VC and 6MWT evaluation.
Chi-square test was used to evaluate the categorical variables. The Wilcoxon test was used to evaluate the intragroup data, and the Mann Whitney test compared the groups to each other. For all statistical tests, the significance level adopted was alpha 5%.
Result
The final sample consisted of 40 patients, divided between GC (n=20) and GI (n=20). The sample was mostly composed of men 26 (65%) and the mean age was 53.5±16 years. Table 1 presents the general characteristics of the sample studied.
Table 1:Characteristics of the patients.
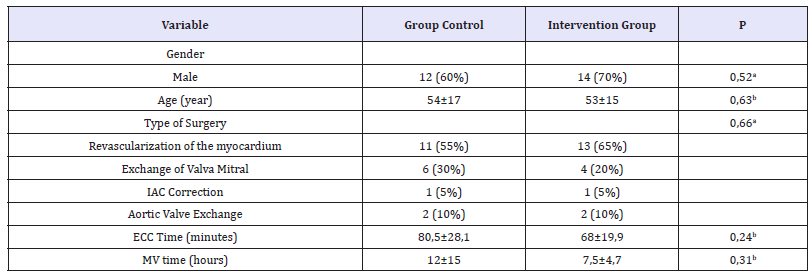
a: Teste de Quiquadrado; b: Teste de Mann-Whitney; IAC: Interatrial communication; ECC: Extracorporeal circulation; MV: Mechanical Ventilation.
The VC behavior, assessed at the beginning and at the end of the study protocol, is shown in Table 2. No significant difference was observed in VC behavior in the CG (26.5±8.9 vs 30.8±7 , 5ml/kg, p=0.08), while in IG a significant increase was observed at the end of the study protocol (25.9±9.5 vs 36.0±6.0ml /kg, p < 0 , 01). No significant difference was observed between the groups in the analysis of VC obtained at the beginning of the study protocol (26.5±8.9 vs 25.9±9.5ml/kg, p=0.83). At the end of the study, VC was significantly higher in IG than in CG (36.0±6.0 vs 30.8±7.5ml/kg, p=0.01).
Regarding performance in the walking test (Table 3), a significant difference was observed between groups (413±90 vs 486±116, p = 0.03).
Table 2:Variation of intergroup vital capacity.
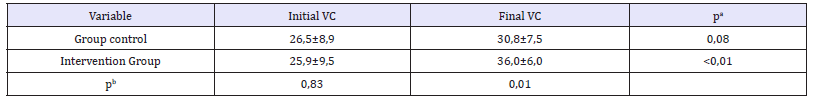
a: Teste de Wilcoxon; b: Teste de Mann-Whitney; VC: Vital capacity Amounts in ml/kg.
Table 3:Variation of intergroup vital capacity.
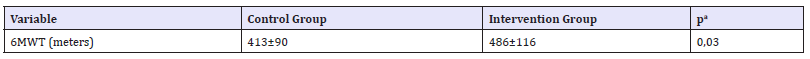
Teste de wilcoxon; 6MWT-six minutes walk test
Discussion
In the present study, a significant increase in VC was observed in patients submitted to a pulmonary expansion therapy protocol based on the daily evaluation of this variable, with an impact on the improvement of the functional capacity of patients in the postoperative period of cardiac surgery.
The worsening of pulmonary function after cardiac surgery is already well documented in the literature [1-7] and several authors propose alternatives to optimize this function as early as possible. Inspiratory muscle training (IMT), for example, is an alternative for improving respiratory function and functional capacity [8]. Matheus et al. [9] adopted an IMT protocol and observed that there was an improvement in tidal volume and vital capacity on the third postoperative day. Cordeiro et al. [10] using the same training protocol verified an improvement in the functional capacity evaluated through the 6MWT.
Another feature used to improve vital capacity is Non-Invasive Ventilation (NIV), which consists of applying positive pressure via an interface that does not enter the airway. Mazullo Filho and colleagues [11] applied this feature immediately after extubation of patients undergoing cardiac surgery and observed an increase in CV (300 to 550 after NIV) that was maintained until the sixth postoperative day. However, it has also been shown that preoperative guidelines have a positive impact on forced vital capacity after the surgical procedure [7,12].
In a literature review, resources such as incentive spirometry, deep breathing exercises, positive expiratory pressure and continuous positive airway pressure (CPAP) have been widely used in the postoperative period of cardiac surgery in order to reestablish pulmonary function [13]. It is noteworthy that in these studies the patients maintained the technique during all hospitalization time, different from the present study that altered the technique according to the evolution of vital capacity.
Dias et al. [14] in their study affirm that there is a reduction of vital capacity after surgery and regardless of the protocol used there will be an improvement of this capacity. Despite the logic of this statement, the goal in this patient profile is to restore pulmonary function as quickly as possible, reducing the rate of complications and length of hospital stay [15-17].
Shakouri et al. [18] concluded that the application of techniques such as breathing exercises and flow enhancers increase lung function in patients undergoing CS. It is worth mentioning that in this study, the intervention was performed in the preoperative period, where the patients performed physiotherapy sessions 15days before the surgery, which consisted of orientation and instructions for breathing patterns, incentive spirometry, improvement of the efficacy of Cough, exercises aimed at strengthening inspiratory musculature and optimizing thoracic expandability.
Conclusion
Based on these findings, it was verified that a Pulmonary Expansion Therapy protocol based on vital capacity improves pulmonary function and increases functional capacity in patients undergoing cardiac surgery.
References
- Weissman C (2004) Pulmonary complications after cardiac surgery. Semin Cardiothorac Vasc Anesth 8(3): 185-211.
- (2014) Ministério da saúde. DATASUS. Informações de saúde. Morbidade e informações epidemiológicas. Disponível em.
- Herdy AH, Marcchi PLB, Vila A, Tavares C, Collaço J, et al. (2008) Pre and postoperative cardiopulmonary rehabilitation in hospitalized patients undergoing coronary artery bypass surgery: a randomized controlled trial. Am J Phys Med Rehabil 87(9): 714-719.
- Higgins TL, Estafanous FG, Loop FD, Beck GJ, Blum JM, et al. (1992) Stratification of morbidity and mortality outcome by preoperative risk factors coronary artery bypass patients. JAMA 267(17): 2344-2348.
- França EET, Ferrari F, Fernandes P, Cavalcanti R, Duarte A, et al. (2012) Fisioterapia em pacientes críticos adultos: recomendações do Departamento de Fisioterapia da Associação de Medicina Intensiva Brasileira. Rev Bras Ter Intensiva 24(1): 6-22.
- Marini JJ, Pierson DJ, Hudson LD (1979) Acute lobar atelectasis: a prospective comparison of fiberoptic bronchoscopy and respiratory therapy. Am Rev Respir Dis 119(6): 971-978.
- Leguisamo CP, Kalil RA, Furlani AP (2005) A efetividade de uma proposta fisioterapêutica pré-operatória para cirurgia de revascularização do miocárdio. Rev Bras Cir Cardiovasc 20(2): 134-141.
- Neto MG, Martinez BP, Reis HFC, Carvalho VO (2017) Pre- and postoperative inspiratory muscle training in patients undergoing cardiac surgery: Systematic review and meta-analysis. Clinical Rehabilitation 31(4): 454-464.
- Matheus GB, Dragosavac D, Trevisan P, Costa CE, Lopes MM, et al. (2012) Treinamento muscular melhora o volume correntee a capacidade vital no pós-operatório derevascularização do miocárdio. Rev Bras Cir Cardiovasc 27(3): 362-369.
- Cordeiro ALL, Melo TA, Neves D, Luna J, Esquivel MS, et al. (2016) Inspiratory muscle training and functionalcapacity in patients undergoing cardiac surgery. Braz J Cardiovasc Surg 31(2): 140-144.
- Mazullo FJBR, Bonfim VJG, Aquim EE (2010) Ventilação mecânica não invasiva no pós-operatório imediato de cirurgia cardíaca. Rev Bras Ter Intensiva 22(4): 363-368
- Miranda RCV, Padulla SAT, Bortolatto CR (2011) Fisioterapia respiratória e sua aplicabilidade noperíodo pré-operatório de cirurgia cardíaca. Rev Bras Cir Cardiovasc 26(4): 647-652.
- Renault JA, Costa VR, Rossetti MB (2008) Fisioterapia respiratória na disfunção pulmonarpós-cirurgia cardíaca. Rev Bras Cir Cardiovasc 23(4): 562-569.
- Dias CM, Vieira RO, Oliveira JF, Lopes AJ, Menezes SLS, et al. (2011) Três protocolos fisioterapêuticos: Efeitos sobre os volumes pulmonares após cirurgia cardíaca. J Bras Pneumol 37(1): 54-60.
- Hulzebos EH, Helders PJ, Favié NJ, De Bie RA, Brutel de la RA, et al. (2006) Preoperative intensive inspiratory muscle training to prevent postoperative pulmonary complications in high-risk patients undergoing CABG surgery: a randomized clinical trial. JAMA 296(15): 1851-1857.
- Yánez BI, Pita FS, Juffé SA, Martinez GU, Pértega DS, et al. (2009) Respiratory physiotherapy and incidence of pulmonary complications in off-pump coronary artery bypass graft surgery: an observational followup study. BMC Pulm Med 9(36).
- Guizilini S, Galacho GC (2012) Complicações pulmonares no pósoperatório de cirurgia cardíaca. In: fisioterapia em cardiologia: da unidade de terapia intensiva à reabilitação (2nd edn) São Paulo: Roca, Brazil.
- Shakouri SK, Salekzamani Y, Taghizadieh A, Sabbagh JH, Soleymani J, et al. (2015) Effect of respiratory rehabilitation before open cardiac surgery on respiratory function: a randomized clinical trial. J Cardiovasc Thorac Res 7(1): 13-17.
© 2018 André Luiz Lisboa Cordeiro. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






