- Submissions

Full Text
Significances of Bioengineering & Biosciences
Impact of HIV/AIDS in India (1986 to 2017)
Prakash Narayan1, Kunwer Singh Mathur2* and Rashmi Mathur3
1Department of Mathematics, G.H. Raisoni University, India
2School of Computational and Integrative Sciences, Jawaharlal Nehru University, India
3Department of Geography, Govt. Autonomous Girls PG College of Excellence, India
*Corresponding author:Kunwer Singh Mathur, School of Computational and Integrative Sciences, Jawaharlal Nehru University, India
Submission: January 19, 2024; Published: March 13, 2024

ISSN 2637-8078Volume6 Issue5
Abstract
In this article, we have endeavored to encompass nearly every facet associated with HIV/AIDS and elucidate the repercussions of HIV/AIDS in India spanning the years 1986-2017. The coverage extends across 29 States and 6 Union Territories (UTs) of India, furnishing a comprehensive overview of the HIV epidemic in the country. Key aspects addressed include prevalence, the number of people living with HIV (PLHIV), HIV incidence, new infections, disease-induced fatalities and vertical transmission. The variances in climate, environment and population distribution among the states of India pose a formidable challenge to disease control. Consequently, it is imperative for researchers, practitioners and the Indian government to intensify efforts in mitigating the impact of the disease. Additionally, following a thorough examination of the data, we have put forth a simple mathematical model pertaining to HIV/AIDS..
Keywords: HIV/AIDS; Epidemic; NACO; WHO; CDC; AVERT
Introduction
AIDS caused by Human Immunodeficiency Virus (HIV) is a very health hazardous disease having a high impact on the world [1-7]. It is originated in non-human primates in Central and West Africa while the actual origin of the Human Immunodeficiency Virus (HIV) has been a subject of scientific research and debate since the virus was identified in the 1980s. There are two types of HIV, namely HIV-1 and HIV-2, in which HIV-1 is more virulent, easily transmitted and cause the vast majority of HIV infections globally while HIV-2 is fewer dangerous, less transmittable and is largely confined to West Africa [8]. Therefore, we focus mainly on HIV-1 in this article. The virus spread through certain body fluids likes, blood, semen, pre-seminal fluid, rectal fluids, vaginal fluids and breast milk that attacks the body’s immune system of the child, specifically, the CD4+ T cells [9,10]. These specific cells help the immune system fight off infections and protect the body against infection. After entering in the body, HIV can destroy several protective cells and hence reduce the immunity to fight against infection. If the person is untreated, HIV reduces the number of CD4+ T cells in the body and finally, the person becomes an AIDS patient. After the opportunistic infections, like TB, leprosy, cancers, Pelvic Inflammatory Diseases (PIDs) or other STIs take advantage of the feeble immune system and maximize chances of the person to get co-infected [8,11-15].
According to WHO [16], the most common route of transmission of HIV infection in India is un-protected sexual intercourse with an infected person, mother to child transmission during pregnancy, childbirth and breastfeeding, sharing of contaminated needles, injecting drug use and transfusion of contaminated blood [11,17-23]. Factors affecting sexual transmission of HIV includes irregular use of condoms, frequency of sexual contact and age at sexual initiation, knowledge, attitudes and beliefs about sexual practices, low literacy and economic conditions, number of sexual partners etc. [6,14,17,24-27]. HIV/AIDS infected person can have different types of symptoms due to different immune system as no two persons infected with HIV can have the exactly same immune response. Some common symptoms are fever, headache, rapid weight loss, sore throat, swollen glands, rash, muscle soreness, rash mouth or genital ulcers, swollen lymph glands, mainly on the neck, joint pain, diarrhea, night sweats, etc. [5,13,22,28]. WHO report [29] shows that HIV/AIDS is the sixth deadliest disease in the world in which almost 36.9 million people globally were living with HIV in 2017 [30]. HIV is a type of virus called a retrovirus and therefore a combination of drugs are used to treat it which is called Antiretroviral Therapy (ART) and is recommended for all people living with HIV (PLHIV) regardless of how long they have had the virus or how healthy they are or whatever the CD4+ T-cells count is [5,13,31,32].
It is suggested that ART must be taken every day exactly as the health care provider prescribes for that. The goal of ART is to reduce a person’s viral load to an undetectable level which means that the level of HIV in the blood is too low to be detected by viral load tests viz., Nucleic Acid Test (NAT), Antigen/antibody test, Enzyme-Linked Immunosorbent Assay (ELISA) test, OraQuick (home test) [12,18,33,34]. There is no available vaccine to cure of the disease [9,23,24,31,32,35]. Combined ARV Therapy (cART) is referred to as Highly Active Art (HAART) and given to the people so that they remain healthy for many years [1,2,7,15,36, 37]. Before starting ART, people with HIV should talk to their health care provider about possible side effects of HIV medicines and potential drug interactions between HIV medicines and other medicines, a person is taking for another disease. Newer HIV regimens cause fewer side effects than regimens used in the past. There are currently five classes of ART drugs each of which inhibits a specific stage in the HIV life cycle, viz., Entry inhibitors, Nucleoside reverse transcriptase inhibitors, non-nucleoside reverse transcriptase inhibitors, Integrase inhibitors, Protease inhibitors. People who get tested and know they are HIV-negative can also make decisions about sex, drug use and health care that can protect them from HIV. For people at very high risk of HIV, taking daily HIV medicine called Pre-Exposure Prophylaxis (PrEP) can prevent them from HIV infection effectively [23,24]. Post-Exposure Prophylaxis (PEP) is also an effective control strategy to minimize the risk of getting an infection if it is immediately taken by the person after accidental exposure to HIV [38].
The burden and transmission of the infection can be controlled by using the mathematical models [39-45]. Several researchers developed different types of mathematical models with various control strategies viz., condom use, PrEP, ART, time delay in infection stages, etc. [24,26]. Two types of mathematical approaches to tackle the disease are found in the literature. The first one is interactions between cells of the human body i.e., mathematical modeling in vivo while the second one is the interaction between the human population. In 1995, a model for HIV/AIDS in Asia is proposed and analyzed by Busenberg et al. [39] and obtained the global stability and existence of multiple equilibria [39]. A mathematical model of HIV/AIDS to predict the impact of national response is developed by Rao et al. [40] and gives the methods for obtaining disease progression parameters using convolution approaches [40]. Grassly et al. [44] modeled the role of injecting drug use and sexual transmission in HIV/AIDS in Russia, China and India mathematically and to control the burden of the infection it is suggested that more research is needed in this regard [44]. A mathematical model for the people who are eligible for ART-1 and ART-2 and who will be on these therapies since the beginning of 2011 is developed and sensitivity analysis is performed by Rao et al. [42]. Mitchell et al. [45] proposed and analyzed a mathematical model for MSM which highlights the importance of collecting MSM sexual mixing data to improve understanding of the impact of targeted interventions and to better guide resource allocation and identifying the most suitable matrix for future modelling of the population [45-52]. The present article is more useful for practitioners as well as researchers in India in the sense that it describes all the aspects, distribution of HIV/AIDS, and the impact of disease in the population across the country. Data and suggestions given in this article may be useful for researchers and practitioners to control the disease by taking serious steps.
Study Area
The study is conducted in the region of India which includes various States and Union Territories. HIV/AIDS is not only a simple medical issue but also a complex societal problem which needs to understand from a biopsychosocial point of view rather than only a biomedical perspective because the families in the societies are fundamentally characterized by strong emotional ties that connect people together and promote sharing and mutual dependence [1,35]. In India, the first known case of HIV was diagnosed by Dr. Suniti Solomon [53] and her student Dr. Sellappan Nirmala amongst female sex workers in Chennai, Tamil Nadu, in 1986 [8,9,15,18,20,23,25]. After the first case of HIV was reported, sex workers began showing signs and symptoms of this baneful disease. At that time, foreigners in India were traveling in and out of the country and it is thought that foreigners were the ones responsible for the first infection [46,47]. In 1987, about 135 more cases came to light among these 14 had already progressed to AIDS. Most of these initial cases had occurred through heterosexuals, but at the end of the 1980s, a rapid spread of HIV was observed among injecting drug users in Manipur, Mizoram and Nagaland. At the beginning of the 1990s, infection rates continued to rise. Prevalence in high-risk groups reached above 5% by 1990. In 1992, the National AIDS Control Organization (NACO) reported that there were between 3.97 and 4.58 million HIV cases [22]. In India, an estimate of cumulative HIV positive people by the end of the year 1994 ranges from 900,000 to 1.9 million and by 2000 it ranges from 500,000 to 1.2 million [25]. In 2005, an estimated HIV patients were 5.206 million [48]. As per UNDP’s 2010 report, India had 2.395 million people living with HIV at the end of 2009, up from 2.27 million in 2008. Adult prevalence also rose from 0.29% in 2008 to 0.31% in 2009. According to the United States National Intelligence Council (NIC), HIV could infect up to 25 million Indians or about 5% of the adult population by 2010 [49].
The Prevention of Mother-To-Child Transmission Programme (PMTCT) and the provision of anti-retroviral treatment were materialized. It also decentralized the effort to local levels and Non Governmental Organizations (NGOs) to provide welfare services to the affected. HIV infection is now common in India. The world has committed to ending the AIDS epidemic by 2030. In various parts of the country where poverty, illiteracy and inadequate health remains, the spread of HIV infection is a challenging issue [32,33,46,47]. According to a National AIDS Control Organization (NACO) report, [50], Among the States/UTs, in 2017, Mizoram has shown the highest estimated adult HIV prevalence of 2.04%, followed by Manipur 1.43%, Nagaland 1.15%, Telangana 0.70% and Andhra Pradesh 0.63%. Besides these States, Karnataka 0.47%, Goa 0.42%, Maharashtra 0.33% and Delhi 0.30% have shown estimated adult HIV prevalence greater than the national prevalence 0.22%, while Tamil Nadu 0.22% had a point prevalence like the national average. All other States/UTs have levels of adult HIV prevalence below 0.22% and around 87.58 thousand new HIV infections and 69.11 thousand AIDS-related deaths occurred in 2017. India is the third-largest affected country with HIV/AIDS in the world.
Tools and Methodology
Various organizations use different types of software to represent the data of HIV/AIDS graphically as the graphical representation of data is more interpretable than numerical data. In particular, the NACO used Spectrum version 5.63 by the recommendations of the UNAIDS secretariat to represent the data of HIV/AIDS of various States/UTs of the country [50]. The numerical data of the country varies from state to state (inter-states also) and UTs and hence ups and downs occurred in the graph. For instance, in the Northeast, the states of Manipur, Mizoram and Nagaland have a prevalence of over 1% but the epidemic trend in them varies considerably. In Manipur, the prevalence declined after reaching a peak of around 3% in 1999 whereas in Nagaland it is stable at around 1% and in Mizoram, it continues to rise after a period of a stable trend. In the region of remaining states, the prevalence levels are low (between 0.05 to 0.11) but rising [50]. The data collected from the various research articles and reports published by NACO, UNAIDS, WHO, UNICEF, etc., are shown graphically by the Mathematica 11.2 version in this article. The validation of these graphs is done by the use of MATLAB software. MS-Excel is also used to demonstrate some data so that the data can be interpretable.
State/UTS-Wise Distribution of AID
The data on HIV/AIDS varies due to the diversity between the States/UTs of the country. Therefore, to find out the burden of the disease within the country it is necessary that first collect complete data of each state and UTs and then study the data carefully and finally make the conclusions which are fruitful for the countrymen as well as to the world. Hence, in this section, we present the collected data in the various facet.
Number of HIV infections (PLHIV)
There is an inter-state variation in the distribution of new HIV infections in India. After the disease came to know, the rate of new infections increased rapidly and have peaked in 1995 and then started to decline. Until April 2004, Maharashtra had more than 16,000 people living with HIV/AIDS [22]. An estimated number of People (adults and children) Living with HIV (PLHIV) in 2011 was 2.09 million compared to the estimated 2.25 million in 2007 and hence 8% declined in the total number of PLHIV [36]. On the other hand, the estimated number of children living with HIV increased from 2007 to 2009 and then declined from 2009 to 2011 and was estimated at 145,000 in 2011 [36]. An estimated 87.58 thousand new HIV infections occurred in 2017, meaning there has been an 85% decline in annual new HIV infections since the peak of the epidemic. However, the trend of decline in new HIV infections has levelled off in recent years and declined only by 27% between the years 2010-2017. The government has made the target to decline the new infections 75% by 2020 from the baseline value of 2010 [50]. We represent the collected data of PLHIV in graphical form as shown in Figure 1.
Figure 1:Graphical representation of number of people living with HIV (PLHIV).
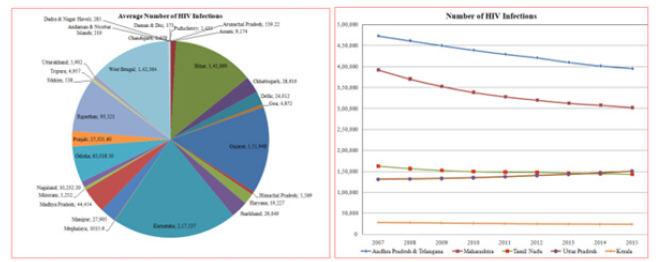
The average number of PLHIV in some states viz., Bihar, Karnataka, Gujrat, West Bengal, etc. is shown in pie-chart while the linear graph is given for the states where the number of people living with HIV is high such states are, Andhra Pradesh & Telangana, Maharashtra, Tamil Nadu, Uttar Pradesh and Kerala. It is clear from the above Figure 1 that the average number of HIV infection in Karnataka-2,17,537 is very high followed by Gujarat-1,51,948; West Bengal-1,42,364; Bihar-1,41,899; Rajasthan-93,321 etc. The number of PLHIV in the states Andra Pradesh & Telangana, Maharashtra and Tamil Nadu is decreased continuously from the year 2007 to 2015 while in Uttar Pradesh this number is increasing in the same time duration. In the state of Kerala, the number of PLHIV remains constant from the year 2007 to 2015.
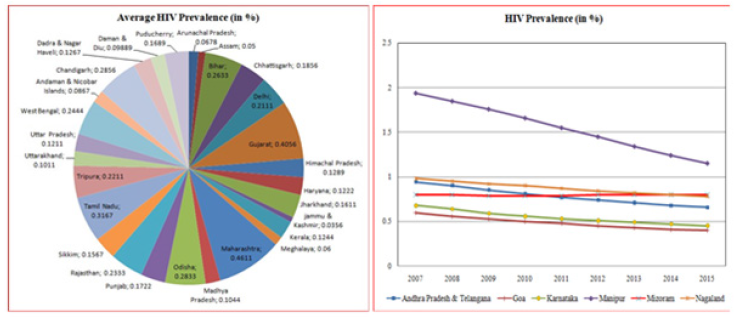
Prevalence
HIV prevalence rate in India can be increased by sex workers, long-distance truck drivers, men having sex with men, injecting drug users and married women etc. [3,6,21,22,35]. Depression also affects the prevalence rate and among HIV sero-positive individuals it is as high as 47% [28]. Prevalence may vary according to geographical areas and different risk groups across the country [9,35]. In 2002, the HIV prevalence at antenatal clinics was as follows; Goa-1%, Tamil Nadu-0.88% while in Maharashtra and Karnataka it increases 1% in all recent years [48]. In 2005, Andhra Pradesh had the HIV prevalence at antenatal clinics was 2% while in other states viz., Goa-0%, Tamil Nadu-0.5%, Mizoram-0.88% and Nagaland-1.63% [48]. It also varies from group to group like MSM, FSWs, IDUs, etc. An estimated HIV prevalence among children during 2007-2011 remained almost constant at 0.04% while in the young male it declined 0.15% in 2007 to 0.11% in 2010 and a similar trend was observed for young female, 0.15% in 2007 and 0.11% in 2011 [36]. In 2009, an estimated 2,390,000 people were living with HIV with an estimated adult HIV prevalence was 0.31% [14]. Adult HIV prevalence among 15-49 years old people have been declined in India and it was estimated at 0.22% in 2017. Mizoram had the highest adult HIV prevalence of 2.04%, followed by Manipur (1.43%) and Nagaland (1.15%). Telangana (0.70%), Andhra Pradesh (0.63%), Karnataka (0.47%), Goa (0.42%), Maharashtra (0.33%) and Delhi (0.30%), were other States with an adult HIV prevalence higher than the national average. The lowest prevalence was found in Jammu & Kashmir (0.03%). Tamil Nadu (0.22%) had a point prevalence similar to the national prevalence. All other States had an adult HIV prevalence like the national average or lower. The pie-chart shown in Figure 2 reveal that the average HIV prevalence in the state of Maharashtra-0.4611% is high followed by the states viz, Gujarat-0.4056%; Tamil Nadu-0.3167%; Odisha-0.2833%; Bihar-0.2633% while Jammu & Kashmir has the lowest HIV prevalence which is 0.0356%. For those states/UTs where the HIV prevalence is very high, the linear graph is presented in the Figure 2 which shows that in Manipur, Nagaland, Andhra Pradesh & Telangana, Karnataka and Goa the prevalence rate is decreased and Manipur has the highest decreasing rate of HIV prevalence. On the other hand, in Mizoram, the prevalence rate is slightly increasing.
Figure 2:Graphical representation of HIV prevalence.
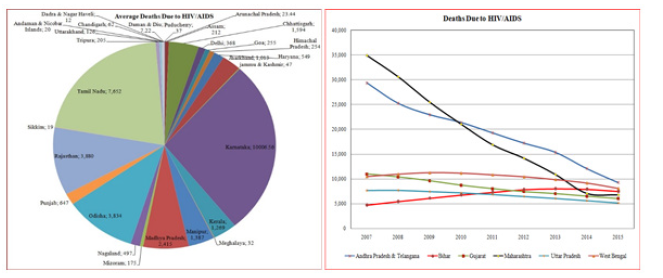
Deaths related to AIDS
Poverty and illiteracy in the country leads to increasing susceptibility to infection and there after death [10,28,33]. According to a NACO report, around 69.11 thousand PLHIV died of AIDS-related causes in 2017 and annual AIDS-related deaths among them kept on increasing until 2005 and then started to decline. AIDS-related deaths have dropped in all India’s States/UTs after attaining a peak in the period from 2005 to 2010, with the exception of some places viz., Assam, Bihar, Jharkhand, Haryana, Delhi and Uttarakhand. In Figure 3 the linear graph and pie-chart are given which represent the deaths that occurred due to HIV/ AIDS between the duration 2007 to 2015. The maximum average death due to HIV/AIDS in India is in Karnataka-10,006.56 followed by Tamil Nadu-7,652; Rajasthan-3,880; Odisha-3,834; Madhya Pradesh-2,415 which are shown in Figure 3. The minimum average number of deaths occurred in Daman & Diu which is 7.22. In some states such as Andhra Pradesh & Telangana, Gujarat and Uttar Pradesh becomes smaller and smaller between 5,000-1,000 when we go through the years 2007 to 2015. In 2007, Maharashtra has the highest deaths around 35,000 which decrease significantly up to the year 2014 while after mid-2014 the death of people then increases. Initially, in the states of West Bengal and Bihar, the total number of deaths increases and some peak points have occurred after that the number of people died due to the HIV/AIDS is decreasing. The peak for West Bengal occurred in the year 2009 while for Bihar it occurs in 2013.
Figure 3:Graphical representation of deaths due to HIV/AIDS.
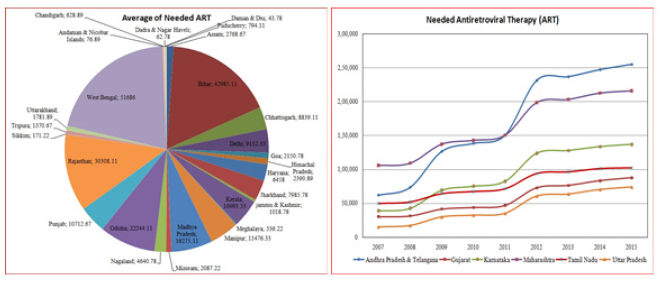
Needed ART
After the introduction of ART, there has been dramatic decreases in AIDS related morbus and deaths [32]. Once patients are initiated on ART, it is necessary that they continue on ART and regularly take precautions given by his or her health care provider. Treatment reduced the annual death rate up to 29% between 2007 to 2009 [34]. There is high requirement of antiretroviral therapy to the person having HIV/AIDS. The need of ART across the country increases with the time (Figure 4). It is obtained that the average number of needed ART in West Bengal was very high in between the duration 2007 to 2015 which was 51, 686. Bihar is the second state where the average requirement of ART was 42,985.11, while Rajasthan was the third state where the needed ART was 30,308.11. The minimum average requirement of ART was in the union territory viz, Daman & Diu in 2007 to 2015 which was 43.78. On the other hand, in 2007, the requirement of ART of Maharashtra was 1,05,664 and in 2015 it was 2,15,971. Similarly, for Andhra Pradesh needed ART was very high. In 2007 it was 62,018 while in 2015 it was increases to 2,54,902. The minimum requirement of ART was in Uttar Pradesh which was 15,049 in 2007 and then it increases to 73,991 for the year 2015.
Figure 4:Graphical representation of people needed antiretroviral therapy.
Prevention of mother to child transmission
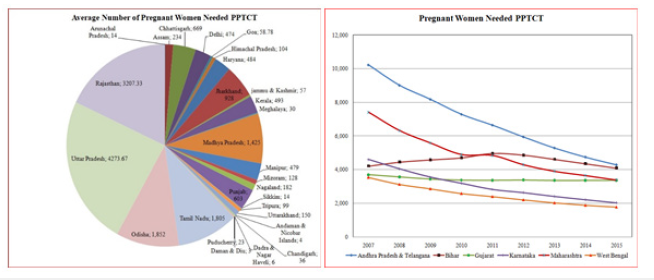
The vertical transmission of HIV/AIDS, in which the disease is transmitted during pregnancy and breastfeeding is also dangerous in India since the beginning of the disease. Around 22,677 HIV positive women who gave birth in 2017 and needed prophylaxis for Prevention of Mother-To-Child Transmission (PMTCT) of HIV in the country. In particular, the PMTCT or Prevention of Parent to Child Transmission (PPTCT) need was highest in Maharashtra followed by Uttar Pradesh, Bihar, Andhra Pradesh, Karnataka, Telangana, West Bengal, Gujarat, Tamil Nadu and Rajasthan. Together, these 10 States contribute almost three fourth of the total PMTCT need in the country. The graphical representation of data of PMTCT or PPTCT from the year 2007 to 2015 are shown in the Figure 5. Here, pie-chart reveal that Uttar Pradesh has the largest average number of pregnant women which required PPTCT and from 2007 to 2015 it was 4,273.67. Rajasthan was at the second number in this regard and the average number of pregnant women needed PPTCT was 3,207.33 followed by Odisha-1,852; Tamil Nadu-1,805; Madhya Pradesh-1,425. In the union territory Daman & Diu, the average number of pregnant women needed PPTCT was smallest which was 3 in the same time period 2007 to 2015. The number of Pregnant women needed PPTCT for the states viz, Andhra Pradesh & Telangana, Maharashtra, Karnataka, Gujarat and West Bengal was decreases from the year 2007 to 2015. In Bihar, the number of pregnant women needed PPTCT increases initially and after the year 2011 it was decreases continuously until the year 2015. Therefore, Bihar had the peak point in 2011.
Figure 5:Graphical representation of pregnant women needed PPTCT.
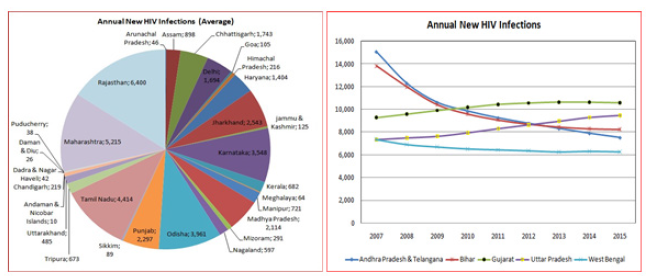
Annual new HIV infections
The annual new HIV cases obtained in several States/UTs of the India are shown in the Figure 6. As shown in the pie-chart, Rajasthan had the largest average number of newly recruited individuals of HIV infection in the country which was 6,400 followed by Maharashtra-5,215; Tamil Nadu-4,414; Odisha-3,961; Karnataka-3,548 and Jharkhand-2,543. The union territory Andaman & Nicobar Is-lands had the minimum number of average new HIV infections annually which was in number 10. The linear graph given in Figure 6 reveal that in the states Andhra Pradesh & Telangana and Bihar the number of annual new HIV cases decreases continuously since the year 2007 to 2015 but in West Bengal this is not the case. From 2007 to 2013 the total number of HIV cases reported annually decreases but after the year 2013 this number almost remains constant till 2015. In Uttar Pradesh the cases of new infection increase continuously since 2007 to 2015. In Gujarat, initially the cases increase up to the year 2011 and then it remains constant till the year 2015.
Figure 6:Graphical representation of newly recruited people of HIV infection annually.
High Risk Groups
There are various high-risk groups which are most vulnerable and make the large impact on the spread of HIV/AIDS [2-4,8,19,31]. HIV epidemic in southern India is highly centered among highrisk groups viz, Female Sex Workers (FSWs) and their clients, Men Having Sex with Men (MSM) [20,22,26,36,49,52,53]. Until march 1998, 5204 AIDS cases were reported in which heterosexual transmission constituted 74.5%, homosexual transmission constituted 0.58%, recipients of blood constituted 7.05%, Injecting Drug Users (IDUs) constituted 7.3% and other 10.92% [19]. In a study it is obtained that MSM had the highest HIV prevalence at 4.4% while IDUs at 7.14% [23]. The high-risk group are as follows:
Men who have sex with men (MSM)
Men having sex with men or ‘gay’ people are highly vulnerable to HIV because of doing unprotected anal sex other than vaginal sex [21]. Financial and professional reward can lead young men into film industry to sell sex on commercial basis [7,54]. In a study it is obtained that MSM are 8 times more likely to be seropositive for HIV and over twice more likely to have STD than non MSM [8]. According to AVERT, gay men and other men who have sex with men are 27 times more at risk of HIV than general population. In India, Madurai, Coimbatore, Chennai, Hyderabad, Delhi etc. have largest numbers of HIV patients by MSM [18,55]. In 1994, about 16% of MSM attending STD clinics of Mumbai were HIV positive [19]. In 2001, the study on Chennai had obtained that 51 MSM attended a community-based clinic over a period of three months out of them 26% MSM were clinically diagnosed to have one or more STDs [19].
Female Sex Workers (FSWS)
Female sex workers play key role to spread HIV infection across the country [3,11,21,25,27,56]. Therefore, the epidemic has spread from urban to rural areas [8,10,22,46]. Enough proportion of female sex workers are rural and traditional which are doing sex for money [7,46]. One of the main reasons of female sex workers to do so is abandoned by their husbands are forced to become FSWs due to illiteracy, non-availability of other opportunity, poor socioeconomic status or to continue their livelihood [11,22,57]. FSWs can be classified into different conceptual groups according to their practices in which common girl prostitutes functioning as fulltime Commercial Sex Workers (CSWs) through brothels, road side hotels, restaurants and part time working girl known as “call girl” do so for resolving their financial problems and survival [25,48,57]. Other countries viz., Bangladesh, Nepal etc. are also the source of illegal immigration of CSWs in India. According to Central Social Welfare Board of India approximately 40% of CSWs population entered the sex trade below 18 years of age [57]. There are sexual trades running inside the country in different metropolitan cities like Delhi, Mumbai, Chennai, Bangalore, Hyderabad etc. [23].
Injecting Drug Users (IDUs)
The burden of HIV infection in India is high among people who inject drugs [8,49]. Kanpur and eastern India have the highest percentage of the person acquiring HIV through injecting drug use [18]. Women are more likely to get infected with HIV than men if they take drugs. At the end of 1980s, rapid spread of HIV was occurred among IDUs in Manipur, Mizoram and Nagaland [48]. A study among women in Manipur in 1997 revealed that HIV prevalence is 57% in the individuals who inject drugs while 27% in those who are not inject drugs [8].
Transgenders/Hijra
Hijra is an Urdu term and the person belongs to this group depends at least partly for their livelihood on working as male prostitutes in India [25]. Therefore, they can also spread the HIV infection mostly in their community. Hijras generally earn money through musical performance at door to door on special occasions viz., male childbirth, weddings etc. Like FSWs, hijra are also working full or part time male prostitutes in the country and lived-in redlight areas of metropolitan cities. Hijras is often stigmatized due to their HIV status and the groups belonging to [5,7,48].
Government Policies
The vast size of India makes very hard to evaluate the effects of HIV on the whole country [48]. Undoubtedly, HIV/AIDS has a powerful negative impact on economy of the country [7]. It is estimated that productive loss from HIV/AIDS in only single year in 1991 is Rs. 1014 billion and an average estimate in the year 1995 is 2.5 million [37]. The Indian government implements various policies to reduce the burden of HIV/AIDS. Screening centers for HIV is the first step taken by the government to screen Indians and blood banks. In 1956 and 1986 legislation passed in India regarding prostitutes didn’t have the objective of abolishing prostitutes and prostitution but the stated objectives of the legislation were suppression and prevention of prostitution [25]. The 1986 act provides some benefits to prostitutes by prohibiting male police officers from searching and draw away them from prostitution unless accompanied by two female police officers [25]. When the cases of HIV/AIDS increase rapidly, it demands introduction of adequate programs to minimize the new cases by using condoms as soon as possible [4]. Indian Council of Medical Research (ICMR) initiated surveillance for the HIV infection in 1985-1986 to react the global reports of HIV/AIDS [8]. In 1987, Indian government set up the National AIDS Control Programme for the co-ordination of national responses such as blood screening and health education [48,58]. In between 1992 to 1999, the rate of condom uses among sex workers in Kolkata increased from 3% to 90% [4]. The information about importance and availability of condoms are given by various advertisement through radio, television so that a maximum number of people can use while having sex.
In 1992, National AIDS Control Organization (NACO) was set up to oversee policies, prevention and control Programme relating to HIV/AIDS and the National AIDS Control Programme (NACP- I) for HIV prevention [47,48,59]. This plan established the administrative and technical basis for Programme management and also set up state AIDS bodies in 25 states and 7 union territories. It was able to make several important improvements in HIV prevention such as improving blood safety. After that, the second phase of the National AIDS Control Programme (NACP-II) was introduced in 1999 which focused mainly on research and development [47,58]. In this regard, NACO identified some academic institutions to conduct operational and demographical research for the treatment of the infection. In 2001, the government adopted the National AIDS Prevention and Control Policy, and Indian pharmaceutical companies marketed Antiretroviral (ARV) drugs with considerable price reduction [8,48]. In 2003, the central government announced the policy to provide HAART to that person who suffers from AIDS [8]. The annual per capita cost of ART was Rs. 48,975 in the center of excellence and Rs. 24,954 in ART centers [34]. In 2005, the total number of AIDS cases reported by NACO was 1,11,608 of which 32,567 were women, and 37% were under the age of 30. In 2006, UNAIDS estimated that 5.6 million people were living with HIV in India, which indicated that there were more people with HIV in India than any other country in the world. In this year, the government of India under NACP introduced various ART centers to provide free treatment in prevention strategies [34].
In 2007, the third phase of the National AIDS Control Programme (NACP-III) targeted the high-risk groups, conducted outreach Programme, amongst others [48]. The national response to HIV/AIDS during the first three years of NACP-III had been commendable in terms of infrastructure and system development, monitoring, and targeted population coverage [14]. Since the beginning of NACP-III, NACO has positioned itself as the promoter and organizer of research on the infection through various routes like networking, partnership and capacity building of institutions across the country [47]. In 2007, using a more effective surveillance system, UNAIDS and NACO agreed on a new estimate between 2 million and 3.6 million people living with HIV which leads India behind South Africa and Nigeria in PLHIV. Over the last decade, the Indian government increases budget allocation from 17% to 29.5% of the total budget for NACP-III to NACP-IV [34]. To create and increase awareness about HIV/AIDS in India the government was launched the seven coach Red Ribbon Express which was flagged off by United Progressive Alliance On world AIDS day, 2009 [60]. Non-governmental and community-based organizations are also working to prevent HIV [8]. Indian government allowed free ART treatment under the national Programme since 2004 to those people which are infected with HIV/AIDS [24]. The Indian government set up a human right viz., Human Immunodeficiency Virus and Acquired Immune Deficiency Syndrome (Prevention and Control) Act, 2017.
The first voluntary counseling and testing center was set up at the Institute of Microbiology in Chennai, India afterward the confirmation of the first case [9,18]. Efforts to improve information, education and communication (IEC) are taken by the government. The State AIDS Control Societies (SACS) was established in 25 societies and 7 union territories to improving blood safety. The Indian government has made a national strategic plan for HIV/ AIDS and STI, for the duration 2017-2024, viz. “Paving Way for an AIDS-Free India”. Expenditure on HIV/AIDS in India increased from 2003 to 2007 and drop by 15% from 2008 to 2009. Currently, India spends about 5% of its health budget on HIV/AIDS. Despite government funding, various international foundations like UNDP, World Bank, Elton John AIDS Foundation, USAID, Global Fund, DFID, CIDS, etc., provides fund to reduce the burden of HIV/AIDS in India [61].
Conclusion
After analyzing the collected data, we have observed that to reduce the number of HIV cases in the states viz., West Bengal, Karnataka, Gujarat, Bihar, Odisha and Uttar Pradesh the strict preventive measures should be taken by the government of India. As the HIV prevalence in some States/UTs such as Andhra Pradesh & Telangana, Goa, Karnataka, Manipur, Mizoram, Nagaland, Maharashtra, Gujarat, Tamil Nadu and Odisha was very large infect Mizoram is the state in the country where the prevalence rate continuously increases and therefore to control it some control strategies like ART, PrEP, PEP, condom, etc. should be necessarily taken. The death rate due to the infection is very high in states Andhra Pradesh & Telangana, Bihar, Gujarat, West Bengal, Karnataka, Tamil Nadu, Odisha and Rajasthan. Bihar is the state in which the deaths of people due to HIV infection is continuously increased since the year 2007 to 2015 and hence some alternative prevention of the infection is required in this state. Some states are needed much supply of ART such states are, Andhra Pradesh & Telangana, Maharashtra, Karnataka, Tamil Nadu, West Bengal, Bihar, Rajasthan, Odisha, Madhya Pradesh, etc. It is also required to control the vertical transmission of HIV infection in the states like Andhra Pradesh & Telangana, Bihar, Uttar Pradesh, Rajasthan, Odisha, Tamil Nadu, and Madhya Pradesh more effectively. It is necessary to control new HIV cases to reduce mortality especially in the states viz., Gujarat, Andhra Pradesh & Telangana, Bihar, Uttar Pradesh, West Bengal, Rajasthan, Maharashtra, Tamil Nadu, Odisha and Jharkhand.
Main problem to effective control of HIV/AIDS are insufficient resources, illiteracy about the infection, social stigma and discrimination, domestic violence. To control the HIV infection in the country, effective and appropriate interventions are required to be developed, more attention should be made to the specific cultural context of sexuality and to how cultural diversity relates to sexual risk behavior. Illiteracy and poverty are the major reasons for women entering commercial sex work at minimum expenses and maximum saving. It increases the risk of getting HIV or other STDs. Since most of the HIV patients are illiterate, poor and belongs to rural areas and hence to reduce the HIV outbreak greater awareness and sex education must begin at the grassroots level [8,46]. However, the government of India now provides condoms freely to the people available in government hospitals or medical colleges. In India, some social factors like stigma and discrimination associated with HIV/AIDS are the major obstacles to control the disease [17,18,48,53]. When the people are facing HIV infection or other opportunistic infections, at that stage medical treatment and psychological support are needed to improve the survival and quality of life to the patients [52]. The government needs to enforce the developed program to customize its strategies to effectively address the emerging vulnerabilities and adapt them to fulfill the requirements of different geographical regions of the country. The study had been shown that in married Indian women, physical and sexual violence from the husband side increased the prevalence of HIV infection [27]. In India, more research is required to control the transmission of HIV with the effect of male circumcision, ART, etc. [4]. It is necessary to advertise the HIV related counseling services and about the testing centers available in the district on the ground level.
More study on voluntary counseling and testing and its impact on HIV is required. Treatment and care programs launched or to be launched by the government should take a broad, and holistic approach [32]. Depression is a most common psychiatric syndrome in HIV patients which leads to non-adherence to ART and consequently poorer health [28]. Therefore, early diagnosis and management of depression are required. There are several mathematical models of HIV/AIDS and its impact around the globe that are developed and analyzed by several researchers. But in the point of view of India, there are more mathematical modeling required which includes some control strategies such as condom use, ART and its side effects on people, male circumcision, premarriage test, etc. through which we can reduce the burden of HIV infection from the population as much as possible. The immune regulation is significantly influenced by the crucial function of antiaging Sirtuin 1 [62-64]. It is essential to evaluate the levels of Sirtuin 1 in infected individuals in India to gauge the severity of both the AIDS virus and associated illnesses. This research is preserved for potential future exploration [65-67].
Conflict of Interest
Authors have declared that no competing interests exist.
Author Contributions
All authors contributed equally in the preparation and development of the manuscript.
Acknowledgement
First author extends a sincere thanks to UGC New Delhi for Non-NET fellowship.
References
- Krishna VA, Bhatti RS, Chandra PS, Juvva S (2005) Unheard voices: Experiences of families living with HIV/AIDS in India. Contemporary Family Therapy 27(4): 483-506.
- Pendse R, Gupta S, Yu D, Sarkar S (2016) HIV/AIDS in the South-East Asia region: Progress and challenges. Journal of Virus Eradication 2(4): 1-6.
- Karnik N (2001) Locating HIV/AIDS and India: Cautionary notes on the globalization of categories. Science, Technology & Human Values 26(3): 322-348.
- Arora P, Cyriac A, Jha P (2004) India’s HIV-1 epidemic. Cmaj 171(11): 1337-1338.
- Thomas B, Nyamathi A, Swaminathan S (2009) Impact of HIV/AIDS on mothers in southern India: A qualitative study. AIDS and Behavior 13(5): 989-996.
- Mothi SN, Lala MM, Tappuni AR (2016) HIV/AIDS in women and children in India. Oral Diseases 22: 19-24.
- Mahal A, Rao B (2005) HIV/AIDS epidemic in India: An economic perspective. Indian J Med Res 121(4): 582-600.
- Godbole S, Mehendale S (2005) HIV/AIDS epidemic in India: Risk factors, risk behaviour & strategies for prevention & control. Indian J Med Res 121(4): 356-368.
- Shrotri A, Shankar AV, Sutar S, Joshi A, Suryawanshi N, et al. (2003) Awareness of HIV/AIDS and household environment of pregnant women in Pune, India. International Journal of STD & AIDS 14(12): 835-839.
- Ghosh J (2002) A geographical perspective on HIV/AIDS in India. Geographical Review 92(1): 114-126.
- Halli SS, Ramesh BM, O’Neil J, Moses S, Blanchard JF (2006) The role of collectives in STI and HIV/AIDS prevention among female sex workers in Karnataka, India. AIDS Care 18(7): 739-749.
- Dhir AA, Sawant S, Dikshit RP, Parikh P, Srivastava S, et al. (2008) Spectrum of HIV/AIDS-related cancers in India. Cancer Causes & Control 19(2): 147-153.
- Nyamathi AM, Ekstrand M, Yadav K, Ramakrishna P, Heylen E, et al. (2017) Quality of life among women living with HIV in rural India. Journal of the Association of Nurses in AIDS Care 28(4): 575-586.
- Bachani D, Sogarwal R (2010) National response to HIV/AIDS in India. Indian journal of Community Medicine 35(4): 469.
- Solomon S, Solomon SS, Ganesh AK (2006) AIDS in India. Postgrad Med J 82(971): 545-547.
- http://www.searo.who.int/india/topics/hiv/en/
- Mawar N, Sahay S, Pandit A, Mahajan U (2005) The third phase of HIV pandemic: Social consequences of HIV/AIDS stigma & discrimination & future needs. Indian Journal of Medical Research 122(6): 471-484.
- Solomon S, Kumarasamy N, Challacombe SJ (2016) The social impact of HIV/AIDS in India. Oral Diseases 22: 15-18.
- Khan S (2004) MSM and HIV/AIDS in India. Naz Foundation International.
- Newmann S, Sarin P, Kumarasamy N, Amalraj E, Rogers M, et al. (2000) Marriage, monogamy and HIV: A profile of HIV-infected women in south India. International Journal of STD & AIDS 11(4): 250-253.
- Singh YN, Malaviya AN (1994) Long distance truck drivers in India: HIV infection and their possible role in disseminating HIV into rural areas. International Journal of STD & AIDS 5(2): 137-138.
- Pallikadavath S, Garda L, Apte H, Freedman J, Stones RW (2005) HIV/AIDS in rural India: Context and health care needs. Journal of Biosocial Science 37(5): 641-655.
- Paranjape RS, Challacombe SJ (2016) HIV/AIDS in India: An overview of the Indian epidemic. Oral Diseases 22: 10-14.
- Vissers DC, Voeten HA, Nagelkerke NJ, Habbema JD, Vlas SJ (2008) The impact of Pre-Exposure Prophylaxis (PrEP) on HIV epidemics in Africa and India: A simulation study. PloS One 3(5): e2077.
- Nag M (1995) Sexual behaviour in India with risk of HIV/AIDS transmission. Health Transition Review 5: 293-305.
- Boily MC, Pickles M, Lowndes CM, Ramesh BM, Washington R, et al. (2013) Positive impact of a large-scale HIV prevention programme among female sex workers and clients in South India. AIDS 27(9): 1449-1460.
- Silverman JG, Decker MR, Saggurti N, Balaiah D, Raj A (2008) Intimate partner violence and HIV infection among married Indian women. Jama 300(6): 703-710.
- Salma K (2016) Depression and coping mechanism among HIV/AIDS patients under anti-retroviral therapy. Indian Journal of Social Psychiatry 32(2): 149-153.
- https://www.who.int/news-room/questions-and-answers/item/what-is-the-deadliest-disease-in-the-world
- (2018) Global HIV & AIDS statistics-fact sheet.
- Bharat S, Aggleton P (1999) Facing the challenge: Household responses to HIV/AIDS in Mumbai, India. AIDS Care 11(1): 31-44.
- Kumarasamy N, Venkatesh KK, Mayer KH, Freedberg K (2007) Financial burden of health services for people with HIV/AIDS in India. The Indian Journal of Medical Research 126(6): 509-517.
- Barnett T, Whiteside A (1999) HIV/AIDS and development: Case studies and a conceptual framework. The European Journal of Development Research 11(2): 200-234.
- Sharma A, Prinja S, Sharma A, Gupta A, Arora SK (2019) Cost of antiretroviral treatment for HIV patients in two centres of North India. International Journal of STD & AIDS 30(8): 769-778.
- Bryan AD, Fisher JD, Benziger TJ (2001) Determinants of HIV risk among Indian truck drivers. Social Science & Medicine 53(11): 1413-1426.
- Raj Y, Sahu D, Pandey A, Venkatesh S, Reddy DC, et al. (2016) Modelling and estimation of HIV prevalence and number of people living with HIV in India, 2010-2011. International Journal of STD & AIDS 27(14): 1257-1266.
- Anand K, Pandav CS, Nath LM (1999) Impact of HIV/AIDS on the national economy of India. Health Policy 47(3): 195-205.
- Cardo DM, Culver DH, Ciesielski CA, Srivastava PU, Marcus R, et al. (1997) A case-control study of HIV seroconversion in health care workers after percutaneous exposure. New England Journal of Medicine 337(21): 1485-1490.
- Busenberg S, Cooke K, Hsieh YH (1995) A model for HIV in Asia. Mathematical Biosciences 128(1-2): 185-210.
- Rao AS, Thomas K, Sudhakar K, Maini PK (2009) HIV/AIDS epidemic in India and predicting the impact of the national response: Mathematical modeling and analysis. Math Biosci Eng 6(4): 779-813.
- Vaidya NK, Wu J (2011) HIV epidemic in far-western Nepal: Effect of seasonal labor migration to India. BMC Public Health 11: 310.
- Rao AS, Thomas K, Kurapati S, Bhat R (2012) Improvement in survival of people living with HIV/AIDS and requirement for 1st-and 2nd-line art in India: A mathematical model. Notices of The AMS 59(4): 560-562.
- Rao AS, Kakehashi M (2005) Incubation-time distribution in back-calculation applied to HIV/AIDS data in India. Mathematical Biosciences & Engineering 2(2): 263-277.
- Grassly NC, Lowndes CM, Rhodes T, Judd A, Renton A, et al. (2003) Modelling emerging HIV epidemics: the role of injecting drug use and sexual transmission in the Russian fed-eration, China, and India. International Journal of Drug Policy 14(1): 25-43.
- Mitchell KM, Foss AM, Prudden HJ, Mukandavire Z, Pickles M, et al. (2014) Who mixes with whom among men who have sex with men? Implications for modeling the HIV epidemic in southern India. Journal of Theoretical Biology 355(100): 140-150.
- ONeil J, Orchard T, Swarankar RC, Blanchard JF, Gurav K, et al. (2004) Dhandha, dharma, and disease: Traditional sex work and HIV/AIDS in rural India. Social Science & Medicine 59(4): 851-860.
- Chandrasekaran P, Dallabetta G, Loo V, Rao S, Gayle H, et al. (2006) Containing HIV/AIDS in India: The unfinished agenda. The Lancet Infectious Diseases 6(8): 508-521.
- Marfatia YS, Sharma A, Modi M (2007) Overview of HIV/AIDS in India. Indian Journal of Sexually Transmitted Diseases and AIDS 28(1): 1.
- Cohen J (2004) HIV/AIDS in India. HIV/AIDS: India’s many epidemics. Science 304(5670): 504-509.
- (2017) India HIV Estimations. Technical Report.
- Bharat S, Aggleton P, Tyrer P (2001) India: HIV and AIDS-related discrimination, stigmatization and denial. UNAIDS 3: 5-66.
- Foss AM, Vickerman PT, Mayaud P, Weiss HA, Ramesh BM, et al. (2011) Modelling the interactions between herpes simplex virus type 2 and HIV: Implications for the HIV epidemic in southern India. Sexually Transmitted Infections 87(1): 22-27.
- Zelaya CE, Sivaram S, Johnson SC, Srikrishnan AK, Suniti S, et al. (2012) Measurement of self, experienced, and perceived HIV/AIDS stigma using parallel scales in Chennai, India. AIDS Care 24(7): 846-855.
- Asthana S, Oostvogels R (2001) The social construction of male homosexuality in India: Implications for HIV transmission and prevention. Social Science & Medicine 52(5): 707-721.
- Go VF, Srikrishnan AK, Sivaram S, Murugavel GK, Galai N, et al. (2004) High HIV prevalence and risk behaviors in men who have sex with men in Chennai, India. JAIDS Journal of Acquired Immune Deficiency Syndromes 35(3): 314-319.
- Zelaya CE, Sivaram S, Johnson SC, Srikrishnan AK, Solomon S, et al. HIV/AIDS stigma: Reliability and validity of a new measurement instrument in Chennai, India. AIDS and Behavior 12(5): 781-788.
- Chattopadhyay A, McKaig RG (2004) Social development of commercial sex workers in India: An essential step in HIV/AIDS prevention. AIDS Patient Care and STDs 18(3): 159-168.
- Patra SK, Chand P (2007) HIV/AIDS research in India: A bibliometric study. Library & Information Science Research 29(1): 124-134.
- (1993) The next battleground AIDS in India. Radio Netherlands Archives.
- https://unicef.in/Story/223/The-Red-Ribbon-Express
- Funds and Expenditures; National AIDS Control Organization (NACO); MoHFW, GoI.
- Martins IJ (2016) Anti-aging genes improve appetite regulation and reverse cell senescence and apoptosis in global populations. Advances in Aging Research 5(1): 9-26.
- Martins IJ (2017) Single gene inactivation with implications for diabetes and multiple organ dysfunction syndrome. J Clin Epigenet 3(3): 24.
- Martins IJ (2018) Biotherapy and the immune system in ageing science. Acta Scientific Nutritional Health 2(4): 29-31.
- https://www.who.int/mediacentre/factsheets/fs360/en/
- https://www.unaids.org/sites/default/files/media asset/UNAIDS FactSheet_en.pdf
- https://naco.gov.in/national-strategic-plan-hivaids-and-sti-2017-24
© 2024 Kunwer Singh Mathur, This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






