- Submissions

Full Text
Significances of Bioengineering & Biosciences
Treatment of Spondylolisthesis Using a Motion Preserving Lumbar Total Joint Replacement: A Case Report
John Alex Sielatycki1*, Marissa Koscielski2, Grant Chudik3, Tyler Metcalf4, Jason Meldau5 and Scott Dean Hodges6
1Steamboat Orthopaedic & Spine Institute, 705 Marketplace Plaza Suite 200, Steamboat Springs, USA
2The University of Notre Dame, 215 Jordan Hall of Science, Notre Dame, USA
3The Ohio State University College of Medicine, 370 W 9th Ave, Columbus, USA
4Foster G. Mcgaw Hospital, 2160 S 1st Ave, Maywood, USA
5Ohio University Heritage College of Osteopathic Medicine, 6775 Bobcat Way, Dublin, USA
63spine, 801 Broad St, Chattanooga, USA
*Corresponding author:John Alex Sielatycki, Steamboat Orthopaedic & Spine Institute, 705 Marketplace Plaza Suite 200, Steamboat Springs, USA
Submission: February 19, 2024; Published: March 01, 2024

ISSN 2637-8078Volume6 Issue5
Abstract
Spinal fusion is the primary treatment option for symptomatic spondylolisthisis. Although effective in alleviating pain and restabilizing the spine, lumbar fusion is associated with long-term sequelae due to the elimination of a motion segment. Alternatives to lumbar fusion for the treatment of grade 1 spondylolsithesis have remained limited due to the complex anatomy, need for stabilization and neural elements. To our knowledge, there are no motion-preservation options that would allow the surgeon to perform a complete laminectomy, facetectomy and segment reconstruction in the setting of isthmic spondylolisthesis. Here we present the case of a 19-year-old female that received motion-preserving lumbar Total Joint Replacement (TJR) for a grade 1 isthmic spondylisthesis at L5-S1. Patient data, including radiographs, were prospectively collected. Two years after lumbar TJR, the patient’s ODI and NRS back and leg pain scores were all 0. Our patient was symptom free at two years follow up which demonstrates that lumbar joint replacement may be a motion-preserving option for similar patients.
Introduction
Spondylolisthesis is a common cause of back and leg pain leading to the need for lumbar fusion [1]. While the two main subtypes of spondylolisthesis (isthmic and degenerative) differ in their etiology, both are commonly treated with a fusion procedure once a patient has failed to improve with nonoperative management [2-4]. For isthmic spondylolisthesis, fusion of the unstable segment is widely regarded as the treatment of choice. To our knowledge, there are no motion-preservation options that would allow the surgeon to perform a complete laminectomy, facetectomy and segment reconstruction in the setting of isthmic spondylolisthesis. Here we describe the first case report of a motion-sparing posterior lumbar total-joint replacement as a treatment alternative for grade 1 isthmic spondylolisthesis.
Case Report
Patient presentation
A 19-year-old female acrobat dancer presented with five years of atraumatic low back pain and bilateral radiculopathy in the L5 distribution. Symptoms were exacerbated with standing, walking and climbing stairs and were alleviated in the supine position. Lumbar spine mobility was restricted, most notably in flexion. The patient ambulated with a normal gate, but was unable to heel or toe walk bilaterally. The patient’s tibialis anterior motor strength was 4/5 bilaterally. Extensor hallucis longus was 3/5 bilaterally. All other motor strengths were normal.
There was decreased sensation to light touch and pinwheel testing in the L5 distribution left and right. Patellar reflexes were normal and Achilles reflex was absent bilaterally. Straight leg raising signs supine and sitting was positive on the left and right sides.
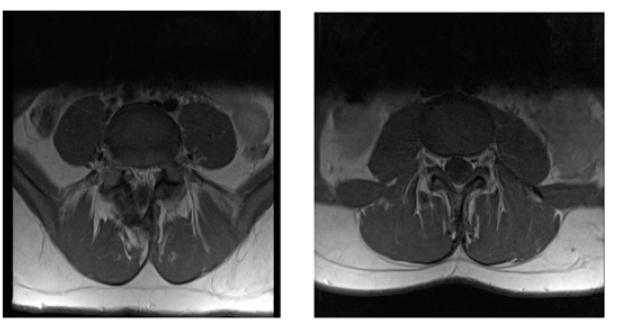
Preoperative radiographs
Preoperative standing radiographs demonstrated a grade 1 isthmic spondylolisthesis at L5-S1 without coronal plane deformity (Figure 1 A&B). Flexion/extension stress radiographs did not show dynamic instability at L5-S1. Preoperative CT scan confirmed L5 pars interarticularis defect with 7mm spondylolisthesis of L5 on S1 (Figure 2 A&B). MRI revealed a foraminal disc herniation with impingement of the exiting L5 and S1 nerve roots (Figure 3 A&B). Patient Reported Outcomes (PRO’s) included an Oswestry Disability Index (ODI) score of 56 with Numeric Rating Scale (NRS) back and leg pain scores of 60 and 40, respectively.
Figure 1:
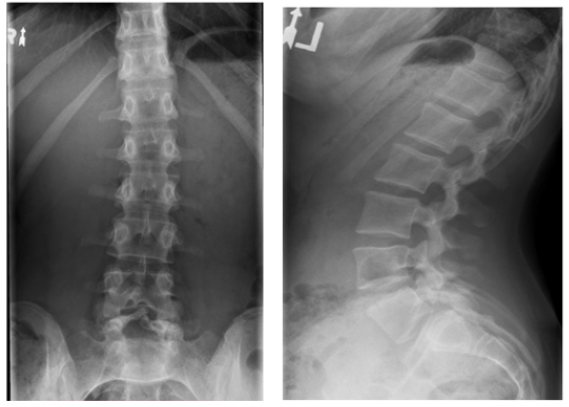
Figure 2:
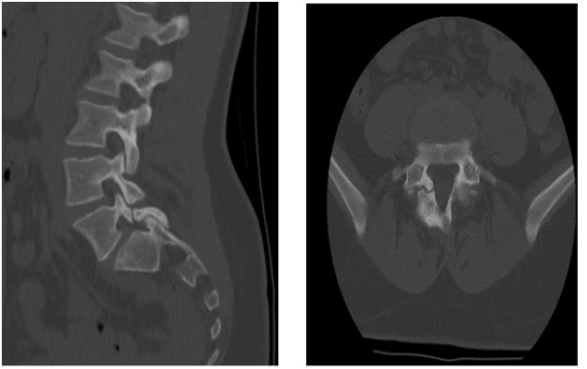
Figure 3:
Procedure decision
Patients with L5-S1 isthmic spondylolisthesis are not usually candidates for approved motion preservation techniques, such as anterior disc replacement. However, lumbar TJR is indicated for grade 1 spondylolisthesis due to its posterior approach and reconstruction and stabilization of the motion segment. Given the patient’s clinical and radiographic presentation and satisfaction of all of the inclusion criteria of the indicated lumbar TJR, the lumbar TJR was chosen as the appropriate procedure for her condition. The biomechanical attributes of the lumbar TJR are among the reasons why the TJR was utilized for this patient. First, the surgical technique and bilateral joints of the prostheses enable the adjacent segment to re-balance the segmental lordosis, compared to the adjacent segment hyper lordosis often observed in fusion cases. Additionally, many of isthmic spondylolisthesis’s cases present with a high Pelvic Incidence (PI) with associated high Sacral Slope (SS). The supra-pedicular three-column osteotomy, associated with the lumbar TJR procedure, allows a 1:1 reduction in PI and SS. The reduction in SS allows the mechanical shear forces acting across the joint to be reduced and the compression forces to be increased. This change in force distribution allows for greater stability of the reconstructed joint. Further benefits of motion at the lumbosacral junction are reduced stress in the pelvis including the Sacroiliac Joints (SI) and the hip joints. Patients with a grade II spondylolisthesis are not a candidate for the lumbar TJR procedure due to multiple factors. Firstly, the center of rotation of the implant utilized in this patient does not allow for the major offset of the two vertebral bodies that are greater than 25%. In order to have a matching fulcrum, the two vertebral bodies must have an offset of 25% or less. Secondly, there needs to be adequate bone-implant contact surface area to ensure a stable bony ingrowth to provide long term stability.
Surgical technique
The surgical technique and implant details are described in a 2021 publication [5]. The lumbar TJR is indicated for the reconstruction and stabilization of the lumbar motion segment to treat symptomatic lumbar degeneration with or without spinal stenosis and up to a grade 1 spondylolisthesis, after failing conservative care. The procedure utilized a bilateral Transforaminal Lumbar Interbody Fusion (TLIF) approach subsequent to laminectomy, bilateral facetectomy and comprehensive discectomy at L5-S1 while preserving the anterior longitudinal ligament, lateral annulus and the cortical endplate. Far lateral tethering ligaments to the exiting L5 nerve roots were released and the L5 nerve root gently mobilized. Fluoroscopy was used to assist with length and height trialing. Powered osteotomies were used to create parallel endplates between inferior L5 and superior S1 vertebral bodies, followed by parallel and co-planar keel slots in the L5 inferior endplate along the axis of the pedicle. The right sided implant was inserted in neutral alignment. The S1 osteotomy, keel cuts and implantation were repeated for the left side. Final radiographs demonstrated appropriate implant positioning and alignment. The wound was closed in a layered fashion. Minimal adaptive changes are needed in the TJR surgical technique for isthmic L5- S1 spondylolisthesis cases. The supra-pedicular osteotomy used to decrease the sacral slope will be larger L5-S1, compared to other lumbar levels. Also, because the vertebral body of L5 and the superior portion of S1 is larger than the remaining levels, it is advantageous to have a higher convergence angle of the keel cuts and implants in the axial plane to provide greater resistance to anterior translation at the bone-implant interface.
Postoperative course
Standardized Enhanced Recovery after Surgery protocol allowed mobilization within 4 hours of surgery completion. The patient was walking independently with standby assist and cleared for discharged home 8 hours post operatively. Multimodal pain regimen consisting of an NSAID, a muscle relaxer and a short course of oral narcotic as instructed for 2 weeks. Daily rehabilitation program included independent walking, stair climbing and truncal isometric muscle strengthening. Unrestricted standing, sitting and walking were allowed immediately following surgery. At 3-months, her radicular symptoms had largely resolved (ODI: 28, NRS-back: 9, NRS-leg: 9) and continued to improve at both 6-months (ODI: 10, NRS-back: 9, NRS-leg:9) and 24-months (ODI: 0, NRS-back: 0, NRS-leg:0). She returned to all desired physical activity. All prior recorded weakness has resolved with normal motor strength in all muscle groups of both lower extremities (5/5). There are no sensory deficits in the lower extremities.
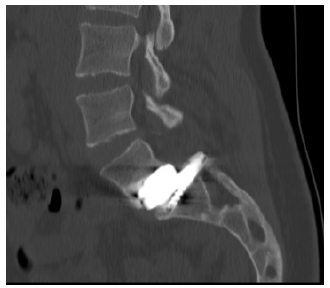
Postoperative radiographs
24-month postoperative standing and sitting dynamic views reveal no evidence of instability with dynamic motion of 12 degrees at the index level as well as normal motion in the remaining lumbar spine and in the pelvis (Figure 4 A&B). CT scan of the lumbar spine shows stability of implants with no osteolysis or heterotopic ossification (Figure 5).
Figure 4:

Figure 5:
Discussion
Here we present the first case report of a patient treated with a lumbar total joint replacement for grade 1 isthmic spondylolisthesis at L5-S1. The patient had progressive improvement in pain and at two years postoperatively, was engaged in numerous athletic activities with no reported back or leg pain and an ODI score of 0. The treatment of high-grade isthmic spondylolisthesis in symptomatic patients will likely continue to require arthrodesis; however, these results suggest that grade-1 isthmic slips may be amenable to a motion-preserving alternative. The clinical outcomes for fusion for L5-S1 spondylolisthesis appear similar regardless of surgical approach or technique used [6]. While a fusion allows for stabilization of the motion segment, altered lumbopelvic kinematics may lead to Adjacent Segment Disease (ASD) [7-9]. Re-operation rates two and five years after lumbar fusion average approximately 10% and 20%, respectively, with most of the need for revision surgery being attributed to proximal ASD [10-12]. However, alternatives to fusion remain limited due to the complex anatomy, neural anatomy and need for re-stabilization. This case illustrates the potential benefits including complete decompression of the neural elements and re-stabilization of the mobile segment using a motion preserving implant. Large scale and longer-term Food and Drug Administration studies are underway to determine the efficacy and durability of this lumbar total joint replacement procedure [13-25].
Funding
This study did not receive funding from any institution or grant.
Acknowledgement
Authors 1, 2 and 6 disclose that they have equity in the company 3spine, which is involved in the manufacture of a device used in this study. Author 1 discloses that they receive consulting fees from Medtronic and Stryker. Authors 3, 4 and 5 have nothing to disclose.
References
- Glassman SD, Carreon LY, Djurasovic M, Dimar JR, Johnson JR, et al. (2009) Lumbar fusion outcomes stratified by specific diagnostic indication. The Spine Journal 9(1): 13-21.
- Hu SS, Tribus CB, Diab M, Ghanayem AJ (2008) Spondylolisthesis and spondylolysis. The Journal of Bone & Joint Surgery 90(3): 656-671.
- Fitzgerald JA, Newman PH (1976) Degenerative spondylolisthesis. The Journal of Bone and Joint Surgery British 58(2): 184-192.
- Hammerberg KW (2005) New concepts on the pathogenesis and classification of spondylolisthesis. Spine (Phila Pa 1976) 30(6 Suppl): S4-S11.
- Sielatycki JA, Devinc CJ, Pennings J, Koscielski M, Metcalf T, et al. (2021) A novel total joint replacement may be an improvement over fusion for degenerative lumbar conditions: A comparative analysis of patient-reported outcomes at one year. The Spine Journal 21(5): 829-840.
- Divi SN, Schroeder GD, Goyal DK, Radcliff KE, Galetta MS, et al. (2019) Fusion technique does not affect short-term patient-reported outcomes for lumbar degenerative disease. The Spine Journal 19(12): 1960-1968.
- Ren C, Song Y, Liu L, Xue Y (2014) Adjacent segment degeneration and disease after lumbar fusion compared with motion-preserving procedures: A meta-analysis. European Journal of Orthopaedic Surgery & Traumatology 24(S1): 245-253.
- Zhong ZM, Deviren V, Tay B, Burch S, Berven SH (2017) Adjacent segment disease after instrumented fusion for adult lumbar spondylolisthesis: Incidence and risk factors. Clinical Neurology and Neurosurgery. 156: 29-34.
- Diebo BG, Beyer GA, Grieco PW, Liu S, Day LM, et al. (2018) Complications in patients undergoing spinal fusion after THA. Clinical Orthopaedics & Related Research 476(2): 412-417.
- Liu J, Deng H, Long X, Chen X, Xu R, et al. (2016) A comparative study of perioperative complications between transforaminal versus posterior lumbar interbody fusion in degenerative lumbar spondylolisthesis. European Spine Journal 25(5): 1575-1580.
- Epstein NE (2018) Lower complication and reoperation rates for laminectomy rather than MI TLIF/other fusions for degenerative lumbar disease/spondylolisthesis: A review. Surg Neurol Int 9: 55.
- Irmola TM, Häkkinen A, Järvenpää S, Marttinen I, Vihtonen K, et al. (2018) Reoperation rates following instrumented lumbar spine fusion. Spine (Phila Pa 1976). 43(4): 295-301.
- Deckey DG, Kalish LA, Hedequist D, Emans J, Proctor M, et al. (2019) Surgical treatment of developmental spondylolisthesis: Contemporary series with a two-surgeon team. Spine Deformity 7(2): 275-285.
- Min JH, Jang JS, Lee SH (2007) Comparison of anterior- and posterior-approach instrumented lumbar interbody fusion for spondylolisthesis. Journal of Neurosurgery: Spine 7(1): 21-26.
- Lee CW, Yoon KJ, Ha SS (2017) Which approach is advantageous to preventing development of adjacent segment disease? comparative analysis of 3 different lumbar interbody fusion techniques (ALIF, LLIF, and PLIF) in L4-5 Spondylolisthesis. World Neurosurgery 105: 612-622.
- Goz V, Weinreb JH, Schwab F, Lafage V, Errico TJ (2014) Comparison of complications, costs and length of stay of three different lumbar interbody fusion techniques: An analysis of the Nationwide Inpatient Sample database. The Spine Journal 14(9): 2019-2027.
- Gornet MF, Lanman TH, Burkus JK, Dryer RF, McConnell JR, et al. (2019) Two-level cervical disc arthroplasty versus anterior cervical discectomy and fusion: 10-year outcomes of a prospective, randomized investigational device exemption clinical trial. Journal of Neurosurgery: Spine 1-11.
- Eliasberg CD, Kelly MP, Ajiboye RM, SooHoo NF (2016) Complications and rates of subsequent lumbar surgery following lumbar total disc arthroplasty and lumbar fusion. Spine 41(2): 173-181.
- Berg S, Tullberg T, Branth B, Olerud C, Tropp H (2009) Total disc replacement compared to lumbar fusion: A randomized controlled trial with 2-year follow-up. European Spine Journal 18(10): 1512-1519.
- Sköld C, Tropp H, Berg S (2013) Five-year follow-up of total disc replacement compared to fusion: A randomized controlled trial. European Spine Journal 22(10): 2288-2295.
- Patel SA, Li NY, Yang DS, Reid DB, Disilvestro KJ, et al. (2020) Patients who undergo primary lumbar spine fusion after recent but not remote total hip arthroplasty are at increased risk for complications, revision surgery and prolonged opioid use. World Neurosurg 144: e523-e532.
- Heckmann ND, Lieberman JR (2021) Spinopelvic biomechanics and total hip arthroplasty: A primer for clinical practice. J Am Acad Orthop Surg 29(18): e888-e903.
- Yang G, Li Y, Zhang H (2019) The influence of pelvic tilt on the anteversion angle of the acetabular prosthesis. Orthopaedic Surgery 11(5): 762-769.
- Abbott JH, Fritz JM, McCane B, Shultz B, Herbison P, et al. (2006) Lumbar segmental mobility disorders: comparison of two methods of defining abnormal displacement kinematics in a cohort of patients with non-specific mechanical low back pain. BMC Musculoskeletal Disorders 7: 45.
- Heckmann N, McKnight B, Stefl M, Trasolini NA, Ike H, et al. (2018) Late dislocation following total hip arthroplasty: Spinopelvic imbalance as a causative factor. J Bone Joint Surg Am 100(21): 1845-1853.
© 2024 John Alex Sielatycki, This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






