- Submissions

Full Text
Significances of Bioengineering & Biosciences
Foot Centering Biomechanics: Part 2: The BioKickstand of The Foot
Dennis Shavelson1* and Sahil Sood2
1Medical Director, The Foot Centering Institute, USA
2President, Valley Radiology Medical Associates, USA
*Corresponding author: Dennis Shavelson, Medical Director, The Foot Centering Institute, Tampa FL, USA
Submission: November 03, 2022 Published: January 04, 2023

ISSN 2637-8078Volume5 Issue5
Abstract
The human foot is an adaptable work of living art. It gathers data from the ground and its surroundings and transports it through the spinal cord to the brain stem, the Limbic brain and the cerebrum for processing. It maintains support, stability and balance creating a foundation for posture. It receives instructions from the brain on how to pose its structure and be engineered by its motors, pulleys, screws, levers and wheels as a biomachine, thousands of times a day over one’s lifetime. Biomechanically, the foot has not been considered as engineered by biomachines that motorize and maintain support and balance of its forefoot, midfoot and rearfoot segments. These segments have independent structure and function but can also close pack to form a single pedal unit of various stiffness and functions allowing the foot to be a multi-function complex machine in closed chain. This paper introduces Supinatory End Range of Motion (SERM) and Pronatory End Range of Motion (PERM) of any joint of the foot and the interval motion that exists in between as the SERM-PERM Interval (S-P Interval) to replace kinetics and kinematics in biomechanics. SERM-PERM examination and the determination of the SERM-PERM Interval determine whether a joint segment will be close packed, flexible, injured or broken in both open and closed chain. This paper introduces The BioKickstand of The Foot as the most important biomachine of the foot and posture because it is the linchpin of human stance and motion. When working, the BioKickstand engages and disengages to morph from being a rigid lever to a functional adapter or anything in between thousands of times a day. S-P Interval motion is not pathological. When broken, the BioKickstand either has a low SERM-PERM Interval and the joint motion is reduced (hallux rigidus) and these BioKickstands are jammed. If the SERM-PERM Interval is high, the joint will not be able to engage for stability and balance (functional hallux limitus, bunions, postural complaints). The BioKickstand of the Foot must be diagnosed as working or broken and treated primarily in addition to any compensatory complaint or injury. this paper considers taking current mainstream lower extremity biomechanics to a neoteric place that may provide a path to improved structural and functional understanding and control of the foundation of human stance and movement, the masterpiece called the Human Foot.
Keywords: Spinal cord; BioKickstand; Rigid lever foot; Microtrauma; Pain; Weakness; Bones and joints
Abbreviations:
SERM: Supinatory End Range of Motion; PERM: Pronatory End Range of Motion; GRF: Ground Reaction Forces
Introduction
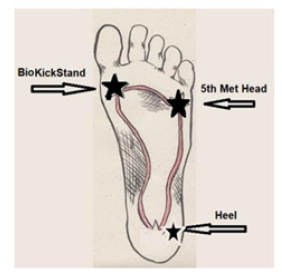
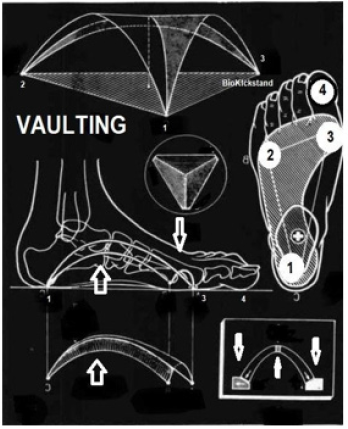
In 1500, Leonardo De Vinci stated that “the human foot is a masterpiece of engineering and a work of art [1]. In 2022, from a more relevant and clinically useful perspective, the authors have updated his quote to read “the human foot is a masterpiece of architecture and engineering and a work of art” - Shavelson-Sood. Bipedal human stance and movement begins at the ground with the foot in a closed chain. The foot has a fanlike vaulted structure that widens and collapses in the forefoot. It is anchored towards the lateral heel and the 5th metatarsal head and mechanized to work at the medial forefoot utilizing its BioKickstand (Figure 1). Biomechanically, the Foot as a whole is a compound machine composed of multiple simple and complex machines working together harmoniously that can seamlessly transition its structural parts (the bones and joints) from being an impacted, close packed, locked, stiff stabilizer, supporter and balancer to being a flexible, mobile, adaptive performer many times a day with blinding speed. The Foot serves as the foundation for human bipedal stance and movement and closed chain biomechanics. Its importance should never be underestimated. This is the second installment introducing a new biomechanical science to consider for researching and practicing Lower Extremity Biomechanics called The Foot Centering Theory of Structure and Function. Part I introduced the basics of Foot Centering and Functional Foot Typing, the initial testing platform for working with The Foot Centering theory [2-8]. Functional Foot Typing examination introduces Supinatory End Range of Motion (SERM) and Pronatory End Range of Motion (PERM) examination of the rearfoot and forefoot segments of the foot that are measured qualitatively. It further determines the rearfoot and forefoot SERMPERM Intervals as the amount of motion that exists between the two. This is the SERM-PERM Interval [9]. This can then be utilized as a starting platform for a neoteric biomechanics algorithm that has its architecture and engineering rooted in the BioKickstand of the Foot. The Foot Centering Theory of Structure and Function Part 2, introduces The BioKickstand of the Foot (Figure 1) as an addition and upgrade to the iconic work of Merton Root DPM in the 70’s [10,11]. The BioKickstand of the Foot is by definition, the most complex machine of the functional human anatomy and the driver of our functional lives.
Figure 1:The bio kickstand of the foot.
The BioKickstand of the Foot Explained
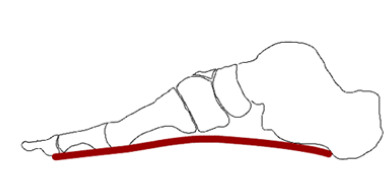
In engineering, there are six simple machines (pulleys, levers, inclined planes, screws, wheel and axles and wedges). A machine composed of two or more simple machines is a complex machine. The BioKickstand of the Foot has examples of all six simple machines making it, next to the brain and heart, the most complex machine of the human body. The BioKickstand of the Foot serves as the linchpin and root of the health, fitness and longevity of our functional lives when we are fixed to the ground (in closed chain). The BioKickstand of the Foot engages when pressed to the ground with enough force at the great toe joint (the 1st MTPJ), to begin a chain of events capable of stiffening the independent bones of the medial forefoot to close pack and function as if one bone. BioKickstand Impaction Force produces a locking force domino effect proximally and laterally into the forefoot, midfoot and rearfoot assisted by peroneus longus, posterior tibial and other minor muscle engines (FHL, FDL, Abductor Hallucis and FHB) and the ligaments of the sole of the foot., This “rigid lever foot” supports, stabilizes and balances the postural chain all the way to the top of the head (Figure 2) [12]. This locking mechanism of the foot occurs when the BioKickstand of the Foot is optimally engaged in stance and when tasking. This extraordinary moment must occur when stability and balance are necessary such as when changing directions, lifting, pushing, moving and tasking efficiently. Engagement of the BioKickstand is regulated by the Central Nervous System as its computer, the nervous system and the myofascial organ as its circuitry and the muscle engines that engage it as its motor. It unlocks naturally due to Ground Reaction Forces (GRF). The BioKickstand of the Foot is composed of the Medial Cuneiform, the 1st Metatarsal Bone and the Great Toe Bones (Figure 3). It becomes active when either the heel or the great toe is elevated from the ground, or the Vault of the Foot becomes more Vaulted in closed chain. When the BioKickstand, for any reason, cannot stabilize the 1st MTPJ in stance or during early midstance, it is broken until proven otherwise. A Broken BioKickstand cannot begin the Impaction closed chain of events that stiffens the pedal bones enough for standing or tasking. This inability to close pack and function as a unit creates a predictable, often preventable domino effect of repetitive microtrauma, pain, weakness, degeneration, deformity and performance and quality of life issues on a case-to-case basis, n=1 (Figure 4).
Figure 2: The locking mechanism of the bio kickstand of the foot.
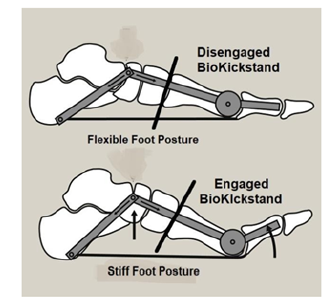
Figure 3:The composition of the biokickstand of the foot.
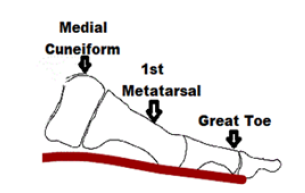
Figure 4:The working bio kickstand of the foot.
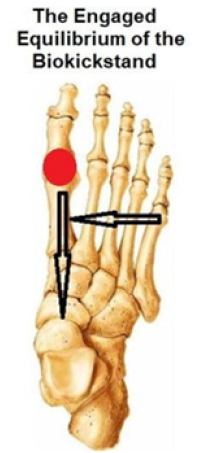
To better understand the BioKIckstand, let’s compare it to the azoic Kickstand that works on an inanimate object such as a Scooter. A Scooter has a back wheel like the rearfoot and a front wheel like the ball of the foot (the forefoot) that supply two contact points with the ground in closed chain. These two contact points cannot independently stabilize, support or balance the scooter upright while stationary. Scooters have a machine called a Kickstand that when manually engaged creates a third point of contact with the ground forming a stable base of support that allows the scooter to stand and balance independently (Figure 5). When forward or backward movement is desired, the kickstand then becomes a handicap and must be manually repositioned off the ground. One would never ride a scooter with its Kickstand down. The human foot, like a scooter, has a rearfoot (rear wheel) and a forefoot (front wheel) that supply two contact points with the ground making it excellent for movement in all directions. It also has a BioKickstand on the medial side of the forefoot, at the bunion joint (1st MTPJ) that can drive a weighted 1st metatarsal head down into the ground forcefully enough to position the BioKickstand to the ground in working order. This is known as the BioKickstand Engaged Position (Figure 6). This anchored position impacts the bones of the BioKickstand to stabilize, support and balance the forefoot skeleton and, by a chain of biomechanical events, the posture for independent standing, lifting, pivoting and shifting of the body. If the BioKickstand cannot engage in phase and with power thousands of times a day, the entire performance and health of the human posture suffers, degenerates and ages. Unlike the Scooter kickstand that needs to be lifted off the ground manually, the BioKickstand is disengaged by the constant upward force applied to it by the hard ground called Ground Reactive Force (GRF). This is known as the BioKickstand Relaxed Position (Figure 6). As the anchoring force reduces under the 1st met head, the BioKickstand becomes less engaged creating a new force equilibrium that makes the foot more flexible, mobile and adaptable for accelerating and changing directions when moving about and tasking. This partially disengaged equilibrium moves laterally into the lesser metatarsal heads at the ball of the foot and then proximally to the lateral side of the midfoot and rearfoot and is known as The Flexible Equilibrium (Figure 7). This Flexible Equilibrium reduces the stability, support and balance of the foot that was provided by the BioKIckstand and makes the appendage more mobile, adaptive and functional in order to move about and perform tasks. As the BioKickstand engages, a new force equilibrium develops that stiffens the foot making it more stiff and anchored for balance, stability and support standing, this decelerates and provides a base of support for changing directions when tasking. This new equilibrium moves proximally down the medial column and medially from the 5th metatarsal head towards the first metatarsal head and is known as The Engaged Equilibrium (Figure 8). This Engaged Equilibrium increases the stability, support and balance of the foot provided by the BioKIckstand and makes the appendage a better anchor and a stronger foundation for the Rigid Lever Foot phase of stance and movement. The pressures under the five metatarsal heads oscillate at different times thousands of times a day within millisecond intervals as we stand or task. Mechanically speaking, there is greater weight under the first metatarsal head and the medial foot when the BioKickstand is engaged and more weight under metatarsal heads 2-3-4 and the lateral side of the foot when the BioKickstand is disengaged (Figures 7 & 8).
Figure 5:An engaged azoic kickstand of a scooter.

Figure 6:The biokickstand of the foot in its disengaged and engaged positions.
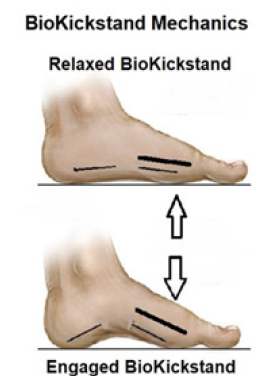
Figure 7:The directions of the flexible equilibrium as the bio kickstand of the foot disengages.
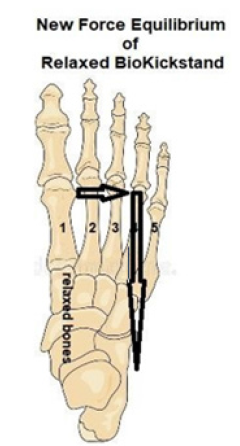
Figure 8:The directions of the engaged equilibrium the biokickstand of the foot engages.
This can be confirmed by X-ray. In a Working BioKickstand, the pressure forces under the five metatarsal heads are distributed on a force plate as follows: 1st met 40%, 2nd met 15%, 3rd met 10%, 4th met 5%, 5th met 30% (Figure 9). In a Broken BioKickstand, the pressure forces under the five metatarsal heads are distributed on a force plate as follows: 1st met 15%, 2nd met 30%, 4th met 25%, 4th met 10%, 5th met 15% (Figure 10). The forefoot weight is now greater 2-3 and 4 These changes represent the Metatarsal Head Pressure Force within the Forefoot SERM-PERM Interval. This means that within the Forefoot SERM-PERM Interval the Pressure Forces under the five metatarsal heads can morph dramatically in a short period of time, thousands of times a day over one’s lifetime without the risk of injury, deformity, arthritis and degeneration. This explains how the foot can be both a rigid lever and a flexible adaptor at different times efficiently, long term. It explains DaVinci’s Masterpiece Foot.
Figure 9:Pressure forces under the five metatarsal heads in a working, engaged bio kickstand of the foot.
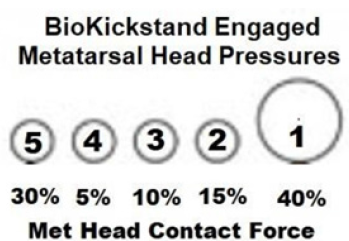
Figure 10:Pressure forces under the five metatarsal heads in a broken.

The functions of the adaptive (stiff or relaxed) BioKickstand of
the Foot include:
a. Control the bioarchitectural and biomechanical chain of events
as the master, complex machine of the human body.
b. Control the contact force under the first metatarsal head in
closed chain.
c. Distribute the contact forces under the five metatarsal heads
differently at different times in closed chain.
d. Control the stiffness and flexibility of the Bony Vault of the Foot
as a chain reaction, in phase and with power.
e. Maintain optimal structural integrity of the foot and posture
in closed chain.
f. Leverage the muscle engines of the foot and leg to increase the
muscular advantage and strength of the muscles.
g. Stabilize and destabilize the foot efficiently and injury free.
h. Not Break!
Broken Biokickstand Biomechanics
A “Broken” BioKickstand is defined as one that is not capable of engaging or anchoring the first metatarsal with enough force to stiffen the bony segments of the medial side of the foot to function as one bone in closed chain. When the BioKickstand is broken, there is not enough rigidity, stiffness, or stability between the bony segments of the medial side of the foot to maintain a static or functional equilibrium during periods of exertion. This leaves the foot and posture too flexible, poorly stabilized, supported and balanced resulting in structural collapse and deformity, degeneration and injury to the bones and soft tissues. This leads to a predictable closed chain of pathological events of repetitive microtrauma, pain, weakness, injury, deformity, degeneration and poor performance up the posture to the head and neck but especially from the lower lumbar area (L-4/L-5) down.
Here are some of the major Pedal Diagnoses that The
BioKickstand of the Foot is the Root Cause of:
a. Functional Hallux Limitus [13]. Bunion Deformity [14].
b. Adult Acquired Flat Foot (AAFD) [15-17].
c. Pediatric Flatfoot [18-21].
d. PTTD [22,23].
e. Plantar Fascitis and the Broken Windlass of the Foot [24].
f. Achilles Tendonitis and Equinus [25]
g. ACL Injury and Knee
h. Hip Dyscrasia
i. Pelvic Floor Disease
j. Low Back Problems–Sciatica [26].
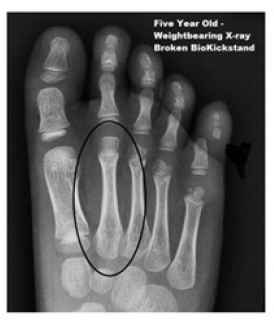
Anecdotally, those who have worked with and practiced with The BioKickstand of the Foot have determined that 80% or more of all people are living life on a Broken Kickstand, some as young as 5 years of age (Figure 11). Only 18% of us possess a working BioKickstand. The remaining 2% have a “Jammed” or rigid BioKickstand which lacks the ability to become more flexible even against GRF. At any stage of time, life or function, if the BioKickstand of the Foot is diagnosed clinically or via x-ray to be Broken, that BioKickstand must be repaired, refreshed or replaced in order to prevent compensatory pathology from continuing up and down the postural chain in the future.
Figure 11:The broken bio kickstand of a five year old.
Diagnosing a Broken Biokickstand-Functional Foot Typing-Forefoot Biomechanics
Functional foot typing is critical
Functional Foot Typing (FFT) of every patient is the starting platform to the diagnosis and integrative treatment of any lower extremity complaint or injury in order to set a baseline for aggressive treatment that will not harm those with different genetics and biomechanics [27].
The forefoot serm-perm interval
Every joint of the foot moves dynamically, efficiently and injury free within the interval of its Supinatory End Range of Motion (SERM) and its Pronatory End Range of Motion (PERM) known as the SERM-PERM Interval. The SERM-PERM Interval of the forefoot is measured qualitatively on the sagittal plane within the Bio Kickstand of the Foot (Figure 12) [28]. The forces moving the BioKickstand within its S-P Interval are efficient and injury free and are not involved in injuring or breaking the BioKickstand. Forces capable of moving the BioKickstand beyond its SERM-PERM Interval are met with resistance. The resistance depends on the shape of the joint surfaces and the soft tissues and bones that maintain its position and motion. Initially, this force is known as an Impaction Force. This force acts as a stabilizer that compels joints to function as if they are one bone. When a joint is stressed with a Force greater than impaction, it is said to be a Traumatic Force. Traumatic forces, when repeated (Repetitive Microtrauma) or overused cause pain, soft tissue pathology, muscle engine compensation, dislocation, arthritis and degeneration in that area. A single Traumatic Force that is very high causes an acute injury that is ballistic in nature. More often, it is the Repetitive Microtrauma (RMT) of overuse or training that causes dynamic lesions of the soft tissues and/or bones in areas of weakness or in other areas in compensation unless the weak areas are rehabilitated [5]. Broken BioKickstands are monitored looking for reduced SERM-PERM Interval when tested over time. Clinically, there are three Forefoot Functional Foot Types that exist. They are the Rigid Forefoot FFT, The Stable Forefoot FFT and The Flexible Forefoot FFT (Figure 13) [29]. When one researches the Functional Forefoot FFT’s and the classification of the working state of the BioKickstand of the Foot, every foot can be classed to be found in four subgroups[30]. These are found in Figure 14. This means that 80% of all feet are Fixing one or more of the biomachines, motors, stabilizers and balancers that stabilize, engineer or maneuver the BioKickstand of the Foot that are not operating effectively may still leave the BioKIckstand Broken and not performing well. Unless all components of the BioKickstand are working order, the predictable chain of events of a Broken BioKickstand will continue.
Figure 12:The forefoot SERM-PERM interval.
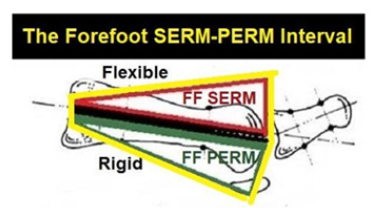
Figure 13:Forefoot FFT testing.
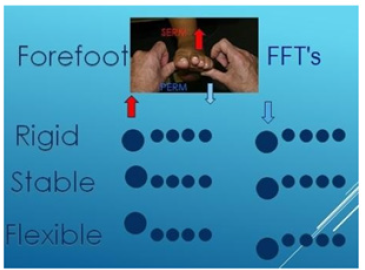
Figure 14:The classification of functional foot types
and biokickstand operational status.
1. Rigid or Stable Rearfoot, Flexible Forefoot Foot Type
Broken BioKickstand (63%)
2. Rigid or Stable Rearfoot, Flexible Forefoot Foot Type
Operational BioKickstand (17%)
3. Flexible rearfoot, Flexible Forefoot Foot Type, Broken
BioKickstand (17%)
4. Rigid rearfoot, Rigid Forefoot Foot Type, Jammed or
Frozen BioKickstand (2%)

The Broken Biokickstand Radiology Diagnosis and Monitoring
Weightbearing AP X-rays of the Foot can be used to diagnose a Broken BioKickstand. This is because the clinical closed chain series of events that occur when a BioKickstand is Broken causes radiographic changes that mirror the clinical signs and symptoms of the BioKickstand [31]. The radiographic changes of a Broken BioKIckstand start in the 1st metatarsal phalangeal joint and go distally into the Hallux while simultaneously coursing laterally along the second to the fourth metatarsals. They then course proximally to the midfoot, rearfoot, ankle joint and up into the posture. This domino effect reflects compensations due to Wolff’s Law of Bone [32,33]. and Davis’s Law of Soft Tissue [34]. which state that bones and soft tissues will adapt to both increases and decreases in forces acting upon them.
Currently, these are the diagnostic radiographic changes of a Broken BioKIckstand that occur over time as parts of the domino effect are listed here: a. Narrowing of the joint space of the 1st MTPJ b. Hallux sessamoid subluxation from under the 1st metatarsal head c. Abductory splay of the 1st metatarsal towards the midline of the body at the medial cuneiform bone d. Increased I-M Angle (3+4) e. Adductory deviation of the Great Toe away from the midline at the 1st MTPJ f. Cortical thinning of the 1st metatarsal shaft g. Diastasis of the 1st and 2nd metatarsal bases (increased space) with a proximal apex h. Diastasis of the medial and intermediate cuneiform bones with a proximal apex i. Narrowing (reduced width) of the shaft of the 1st metatarsal j. Widening (increased width) of the shaft of the 2nd metatarsal k. Cortical thickening of the shaft of the 2nd metatarsal l. Medullary Canal narrowing of the 2nd metatarsal shaft m. Widening of the 3rd metatarsal shaft n. Cortical thickening of the shaft of the 3rd metatarsal o. Medullary Canal thinning of the shaft of the 3rd metatarsal p. Widening of the 4th metatarsal q. Cortical thickening of the shaft of the 4th metatarsal bone r. Medullary Canal thinning of the 4th metatarsal bone s. Navicular changes t. Talar changes u. Diastasis of the Tibia and Fibula v. Everted calcaneus
X-rays of feet with a Working BioKickstand and an Optimal FF SERM-PERM Interval have: A. The transverse shaft thickness of the first metatarsal bone approximately twice that of the 2nd - 3rd and - 4th metatarsals, B. The cortical thicknesses of the 2nd thru 4th metatarsals should be about even with the 2nd metatarsal C. The medullary canal thickness of the metatarsals 1-5 is greater than the cortical thickness of both sides of the shaft. D. The zone between the 1st and 2nd metatarsal bases is well impacted with no spacing noted (No 1-2 Metatarsal Clearing) E. The zone between the medial cuneiform and the middle cuneiform is well impacted with no spacing noted 2nd metatarsal base (Medial Cuneiform-Middle Cuneiform Clearing) (Figure 15).
Figure 15:AP X-ray of foot: working bio kickstand. less than three precursors.

Initially, a Broken BioKickstand AP X-ray will demonstrate reduction of the cortical thickness of the 1st metatarsal shaft and a transfer 2nd metatarsal cortical shaft increase and medullary cavity decrease reflecting the reduced weightbearing force under the 1st metatarsal head and the increased weightbearing force under the 2nd metatarsal head (Figure 16). This begins the chain of biomechanical chain of events destined to impact human movement up the postural chain (think knocked knees). Next, there is a clearing (separation) of the 1st met- 2nd met bases and to a lesser extent, the 2nd metatarsal shaft thickens in width and mass. Next, the 3rd metatarsal cortical thickness increases and its medullary cavity reduces and the width of the 3rd metatarsal shaft increases in mass. Later, the 4th metatarsal cortical shaft thickness increases, its medullary cavity reduces, and the width of the 4th metatarsal shaft increases in mass see (Figure 17). Reading 4 or more precursor diagnostic findings on an AP X-ray radiology study justifies a diagnosis of a Broken BioKickstand of the Foot. In our combined 60-year experience in both Podiatry and Radiology, the majority of weightbearing AP radiographs taken in radiology practice, when inspected for signs of a Broken BioKickstand are Broken. This is because until the age of three, we have not fully connected the CNS with the peripheral nervous system, autonomic system and spinal reflex arcs together and so until that age (+Babinski Sign), feet should be supported by shoes or used barefooted over soft, forgiving surfaces as much as possible. It should be noted that once a Broken BioKickstand is successfully repaired conservatively or surgically, a reversal of these changes should occur. The 2-3-4 metatarsal shaft follow up x-rays should reveal cortical thickness narrowing, medullary cavity widening, and shaft thickness narrowing and 1st metatarsal shaft cortical thickening (Figure 18). If there is not a reversal, the BioKickstand may still be broken or may need surgery.
Figure 16:AP X-ray, early broken bio kickstand. note the cortical thinning of the 1st metatarsal and cortical thickening of the second metatarsal as well as narrowing of its medullary cavity..

Figure 17:AP X-ray, broken bio kickstand. note the clearing at the 1-2 metatarsal bases and medial and middle cuneiforms, the widened 2nd met, the reduced medullary cavity, the widened 3rd met and reduced medullary cavity. arrows point to many areas of diagnostic pathology of the broken bio kickstand domino effect. clinical tests with high FF SERM- PERM interval.

Figure 18:AP X-ray, post op bio kickstand repair. note increased cortical thickening 1st met, reduced 1st met 2nd met base clearing. reduced 2nd met cortical thickening and reduced 2nd met medullary cavity.

The Major Motor of the Biokickstand-the Peroneus Longus (Pl) Muscle Engine
The primary muscle engine that engages the BioKickstand of the Foot is the Peroneus Longus Muscle Engine (PL). The PL becomes inhibited, exhausted and atrophic after a BioKIckstand is injured or it may be the root cause of the break. This muscle engine and others that also assist in engaging the BioKickstand like Flexor Hallucis Longus, Flexor Digitorum Longus, Flexor Hallucis Brevis and Flexor Digitorum Brevis, deserve more attention and importance in Biomechanics. Studies have determined that 40% of those presenting with ankle instability and foot problems have peroneal dysfunction due to its leverage and power being reduced [35]. In closed chain, at heel contact, the Peroneus Longus pronates the rearfoot to transfer weight and pressure from the lateral to the medial side of the foot. Along with the Peroneus Brevis, it then stabilizes the rearfoot at Pronatory End Range of Motion (PERM) creating close packing of the bones and leveraging of the muscle engines crossing the ankle into the foot (Figure 19) [36-38]. A recent study has determined that the peroneus longus tendon inserts into the first metatarsal base 100% of the time and the medial cuneiform bone only 20% of the time in a fan-like fashion close packing these bones. Their cadaver dissections also revealed PL inserts into the first dorsal interossei muscle 37% of the time, the flexor digiti quinti minimi muscle 31% of the time, the opponens digiti quinti minimi muscle 31% of the time and the oblique head of the adductor hallucis 4% (Figures 20 & 21). The article concluded that the major function of the peroneus longus is to resist varus forces at the base of the first metatarsal. Secondarily, peroneus longus maintains the longitudinal and transverse arches of the foot at the midfoot. It is important to note that most feet close pack before the calcaneus is “overpronated” (everted beyond a midfoot bisection of the lower leg). This means that most Rearfoot FFT’s are Rigid or Stable not Flexible Rearfoot FFT’s. They are not capable of over- pronating without spraining, dislocating or fracturing. In closed chain, during early midstance [39]. The force of the peroneus longus muscle engine pronates the forefoot transferring body weight from the lateral to the medial side of the foot engaging the bones of the BioKIckstand of the Foot. This increases the stability, support, and balance of the foot and also sets up the chain of events allowing the bones of the foot to act as if one bone after midstance (the rigid lever). Unless the peroneus longus muscle engine engages the BioKickstand of the Foot, the foot cannot maintain the vaulted position required for its rigid lever phase It should be noted that there are not many additions to the literature that give evidence to the importance of the PL muscle engine [40]. Finally, PL provides support to the transverse and lateral longitudinal arches as it forms an anastomosis with tendons of the Posterior Tibial Muscle engine to form a stirrup under the Vault of the Foot (Figure 22). All broken BioKickstands coincidentally have a PL that leverages poorly and is anatomically slack and ineffective [41,42].
Figure 19:The peroneus longus belly and the peroneus longus tendon, the cuboid groove stabilizing the ankle and subtalar joint.
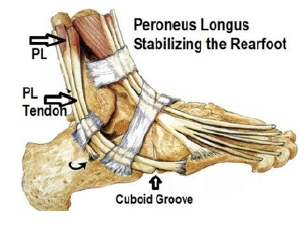
Figure 20:Peroneus longus tendon with multiple insertions in the forefoot and medial cuneiform bone.
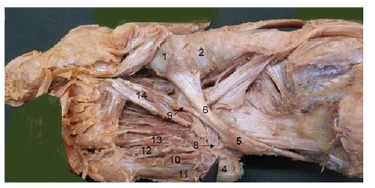
Figure 21:Peroneus longus tendon with multiple insertions in the forefoot.

Figure 22:The anastomosis of posterior tibial - peroneus longus tendons that stirrup the foot.

The Posterior Tibial (Pt) Muscle Engine-The Major Engager of The Medial Midfoot Vault
The Posterior Tibial Muscle Engine (PT) has been misunderstood and overrated in Biomechanics. Although the PT is the most powerful supinator muscle engine of the vault of the foot, it is too weak to have enough force to maintain the Vault of the Foot on its own. The PT fails in most feet resulting in structural collapse and what is now being called the stages of PTTD [43]. Both the muscle belly and the tendon of the Posterior Tibial Muscle Engine lies deep either against or adjacent to bone making it a major stabilizer, supporter and balancer of the Foot (Figure 23a). It is so deep under the calf muscles that many diagnostic testing and therapeutic procedures that work for other muscles cannot be used successfully almost all anatomy texts and biomechanics teachings, mistakenly, the Posterior Tibial Muscle Engine insertions are described in a manner similar to this: “Its insertion is complex: on the side there are multiple insertions on the navicular tuberosity; on the plantar, the main tendon has insertions on all of the tarsal bones with the exception of the talus, and on the second, third, and fourth metatarsals, with fan- shaped fascicles” (Figure 23b) [44].
Figure 23a:Posterior tibial muscle engine deep anatomy.

Figure 23b:Mistaken posterior tibial muscle engine - plantar insertions as a multi-osseous fan that can engage the midfoot biomechanically in closed chain[45].

There is a recent high level addition to the literature where seven authors dissected 118 cadavers for the insertions of the Posterior Tibial Muscle Engine. All 118 had an insertion in the Navicula and the medial cuneiform, As to the insertions into other pedal bones by the PT tendon, the authors proved that there were four different lesser insertion classifications into other bones that affect the power, pull and biomechanics of the PT tendon (Figures 24-26) - refer to reference 44.The article strongly suggests that many cases of PTTD are linked to a weak PT insertion that is more like a closed fan than an open one which has been previously unappreciated. This also goes to explain why clinically, to date, soft tissue repairs such as tendon transfers of other flexors or Anterior Tibial to the navicular often fail [45,46]. In Foot Centering Theory, supporting the Vault of the Foot conservatively with props or surgical procedures that repair the Broken BioKickstand that is involved in all of these cases could possibly lead to better outcomes with reduced biomechanical collateral damage (Figure 27) [47]. This is the same mechanism that is used to repair a sagging roof in architecture. “Until we can classify the plantar insertion of the Posterior Tibial Insertion on a case-to-case basis for conservative and surgical planning of PTTD, the Posterior Tibial Muscle Engine must be considered weak, poorly leveraged and powerless to engage the midfoot and tarsus of The Vault of the Foot and needs strengthening, reduced activity and/or conservative or surgical support” [48]. The literature is now suggesting that aggressive conservative treatment for PTTD should be the primary option reserving surgery as a salvage last option [49,50].
Figure 24:Posterior tibial insertion classification type 1. !st met base and medial cuneiform insertion. note: there are no fanned insertions into lateral tarsal bones or mets 2-3-4. the fan is closed.
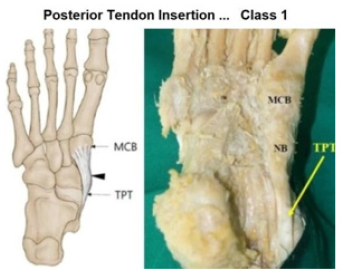
Figure 25:Posterior tibial insertion classification type 2. there is one additional insertion into the lateral cuneiform. there are no other insertions into tarsal or metatarsal bases. the fan is closed.
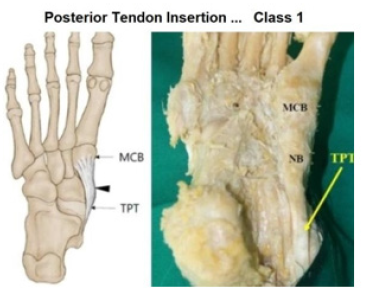
Figure 26:Posterior tibial insertion classification type 3. multiple pt types that insert into more of a fanlike distribution showing varying degrees of the fan being open.

Figure 27:Supporting the vault of the foot with conservative or surgical treatment, note the lift under the navicular area and the drop under the 1st and 5th metatarsal heads that posterior tibial cannot accomplish.
Treatment of a Broken Biokickstand of the Foot
The treatment of a Broken BioKickstand of the Foot deserves stand-alone publication and for that reason, Treatment of a Broken BioKickstand of the Foot will be deferred to future publications of The Foot Centering Theory of Structure and Function.
Discussion
The recent literature contains a dearth of neoteric diagnostic and conservative treatment theories as the focus of podiatry practice has become more and more surgical and the practice of physical therapy and other therapeutic disciplines have become complaint and pain focused on the sacrifice of root cause care and conservative nonoperative care including biomechanics. All professionals with a core interest in human movement, tasking and function need to work together to set the Biomechanical Ship back on course for the sake of the future of mankind. A future that is not waiting for an injury or a weakness or a deformity or a degenerative process but one that is proactive, preventative and patient focused. This paper attempts to evolve current, mainstream biomechanics and human movement towards a more straightforward, acceptable, teachable, researchable and purposeful status to improve those suffering from events rooted in underpinning biomechanical and bioarchitectural pathology. It suggests we look at biomechanics as more of a qualitative process, consider changes in terminology and elevation of goal sets that aim these sciences towards better and more valid clinical outcomes than current theory and deterministic research is providing [51]. We acknowledge that The Foot Centering Theory of Structure and Function has its flaws and areas that need fine tuning and upgrading but suggest that open minded readers frustrated with the current state of biomechanics may find it worthy of visiting, practicing, editing and advancing over time [52].
There are many important points of possible debate and
unanswered questions that need further study and reporting. They
include:
a. Declaring Rootion Biomechanics, Subtalar Joint Theory and
overpronation of the Rearfoot Iconic but in need of iconoclastic
replacement due to its stagnation of Biomechanics for so long
[53,54].
b. Adding Structure of the human body as foundational in
biomechanical thinking and problem solving.
c. Accepting that the Forefoot may be the greatest root cause in
biomechanics and in need of independent examination and
diagnosis.
d. The holistic introduction of adaptability of the tissues (Wolff’s
and Davis’s Laws) and the neuromuscular systems as keys
to understanding and practicing biomechanics and human
movement.
e. The introduction of a primary complex biomachine, The
BioKickstand of the Foot, as a diagnosis for biomechanical
treatment before, during and after injury, pain and performance
complaints. rather than the structures and muscle engines and
simple machines that are only parts of this complex machine as
this should take biomechanics to greater heights as a science.
f. Adding biomechanical radiology as a diagnostic and monitoring
tool in the diagnosis toolbox as a separate subfield of radiology
in the care of the life , heatl and lifestyles of mankind.
g. The fact that the Posterior Tibial tendon insertion in the foot
has different classes may play a role in the ability of the midfoot
to become a rigid lever.
h. The fact that the Peroneus Longus tendon insertion in the
foot has different classes may play a role in the ability of the
BioKickstand of the Foot to engage and work.
i. Present biomechanics in a more stochastic rather than
deterministic fashion allowing peer reviewed, clinically
applicable research “to surface” [55].
Future Applications of the Foot Centering Theory
SERM-perm examination in children for early prevention and treatment
In 1940, S.S. Lifson, a dentist, presented a novel plan to The American Public Health Association entitled How the community dentist can participate in a school dental program. The plan included that “all children should be examined to discover dental defects, and all such examinations should be conducted by dentists”. We all know how well this program has worked regarding dental health and hygiene. School Vision programs have had similar success. Foot Centering can be the algorithm that enables foot examination to be added to other professions to begin school preventive medicine programs [56].
Prevention of diabetic ulcers/amputations
As SERM-PERM Foot Typing predicts the locations of areas of potential extreme pressure in the weightbearing foot, foot typespecific, it can be used at any age and stage to predict the locations of potential diabetic or neuropathic or overuse syndrome ulceration.
Performance enhancement
Since a Broken BioKickstand reduces the stability, support, strength and balance of the feet and posture, once repaired or replaced, a well functioning BioKickstand of the Foot will allow muscle engines and other tissues to be more able and focused on performance of stance, movement and tasking than previous.
Fall prevention
Since a Broken BioKickstand increases sway, perturbation and balance of the feet and posture, once repaired or replaced, a well functioning BioKickstand of the Feet will allow for improved stability, support, strength and balance of the feet and posture reducing the risk and existence of falls.
Research
Applications and Tools of Broken BioKickstand Biomechanics
Conclusion
The authors have introduced a neoteric, iconoclastic approach to the understanding of foot biomechanics in describing the medial cuneiform, first metatarsal and great toe as the BioKickstand of the Foot and have merged it with SERM-PERM Foot Typing Classification and Foot Centering Theory with and Radiologic Imaging to advance Human Biomechanics from the ground up. We describe using literature, references. and a logical progression that the forefoot is the critical target of underpinning biomechanical care. The BioKickstand of the Foot is the most essential machine in human biomechanics. Understanding, diagnosing, treating and monitoring the BioKickstand of the Foot is a key that may unlock the art and science of human bipedal stance and movement to greater importance going forward.
References
- Rinzler C (2013) Leonardo's foot: How 10 toes, 52 bones and 66 muscles shaped the human world. Bellevue Literary Publishing, US.
- Shavelson D (2018) The functional foot typing system; lower extremity biomechanics. BipedMed Publishing, US.
- https://zoboko.com/text/gw0p563w/lower-extremity-biomechanics/125.
- Shavelson D, Steinberg J, Bakotic B (2017) The diabetic foot; principles of diabetes mellitus. In: Poratsky L (Ed.), Springer Inter Pub, US.
- Shavelson D (2018) The foot centering theory of structure and function: Controlling pedal stability, support, strength, symmetry and balance improve closed chain stance and function. Foot and Ankle Quarterly 29(4): 263-279.
- Shavelson D (2009) The common functional foot types, The foot in closed chain.
- Shavelson D (2010) Functional foot type closed chain characteristics. The Foot in Closed Chain.
- Shavelson D (2010) The supine biomechanical evaluation. The Foot in Closed Chain.
- Shavelson D (2009) Profiling the pedal snowflakes. The Foot in Closed Chain.
- Shavelson D (2009) The functional foot typing forefoot exam. The Foot in Closed Chain.
- Root ML, Orien WP (1977) Normal and Abnormal Function of the Foot, Clinical Biomechanics Corp. Los Angeles, US.
- Shavelson D (2010) Beyond root, subtalar neutral and pronation. The Foot in Closed Chain.
- Welte L, Kelly l, Lichtwark G, Rainbow M (2018) Influence of the windlass mechanism on arch-spring mechanics during dynamic foot arch deformation. J R Soc Interface 15(145).
- Scherer P (2007) Understanding the biomechanical effcts of hallux limitus. Podiatry Today 20(8).
- Chang c, Wang Q, Guo J, Li D, Fan Y, et al. (2020) The biomechanical relationship between hallux valgus deformity and metatarsal pain. J Health Eng.
- Richie D (2007) Biomechanics and clinical analysis of the adult acquired flatfoot. Clinics in Podiatric Medicine and Surgery 24(4): 617-644
- Henry J, Shakked R, Ellis SJ (2019) Adult-acquired flatfoot deformity. J Foot & Ankle Ortho 4(1).
- Fernandez S, Gonzalez-Martin C, Alonso-Tajes, Seoane-Pillado T, Pertega-Diaz S, et al. (2017) Flat foot in a random population and its impact on quality of life and functionality. J Clin Diagn Res 11(4): LC22-LC27.
- Pourghassem M, Kamali N, Mehrdad F, Soltanpour N (2016) Prevalence of flatfoot among school students and its relationship with BMI. Acta Ortho et Truamat Turcica 50(5): 554-557.
- MacKenzie A, Rome K, Evans A (2012) The efficacy of nonsurgical interventions for pediatric flexible flat foot: a critical review. J Pediatr Orthop 32(8): 830-834.
- Halabchi F, Mazaheri R, Mirshahi M, Abbasian L (2020) Pediatric flexible
- Ford S, Scannell B (2017) Pediatric flatfoot: Pearls and pitfalls. Foot Ankle Clin 22(3): 643-656.
- Bubra P, Keighley G, Rateesh S, Carmody D (2015) Posterior tibial tendon dysfunction: an overlooked cause of foot deformity. J Family Med Prim Care 4(1): 26-29.
- Yao K, Yang T, Yew W (2015) Posterior tibial tendon dysfunction: overview of evaluation and Orthopedics. 38(6): 385-391.
- Latt L, Jaffe D, Tang Y, Talianovic M (2020) Evaluation and treatment of chronic plantar fasciitis. Foot Ankle Orthop 5(1).
- Demassa N, Whitaker M (2015) Equinus: Its surprising role in foot pathologies. Lower Extremity Review pp. 27-30.
- Bird AR, Payne CB (1999) Foot function and low back pain. The Foot 9(4): 175-180.
- Shavelson D (2011) The biomechanics of the diabetic foot. Global perspective on diabetic foot ulcerations.
- (1985) Injury biomechanics research and the prevention of impact injury; injury in America; Institute of Medicine (US) and National Research Council (US) Committee on Trauma Research. National Academies Press, US.
- Peacock D (2015) The peacock press test. Podiatry Management pp.137-143.
- Kanatli U, Yetkin H, Simsek A, Ozturk A, Esen E, et al. (2008) Pressure distribution patterns under the metatarsal heads in healthy individuals. Acta Orthop Traumatol Turc 42(1): 26-30.
- Roque W, Arcaro K, Bayarri AA (2013) Mechanical competence of bone: A new parameter to grade trabecular bone fragility from tortuosity and elasticity. IEEE Transactions on Biomedical Engineering 60(5): 1363-1370.
- Stock J (2022) Wolff’s law - bone functional adaptation; the International Encyclopedia of Biological Anthropology. John Wiley & Sons, US.
- Wolf J, Fallat L (2020) Osseous remodeling secondary to a chronic intermetatarsal ganglion cyst: a case report. Foot and Ankle Surgery 29(5): 1098-1100.
- Cyron C, Humphrey J (2017) Growth and remodeling of load-bearing biological soft tissues. Mechanica 52(3): 645-666.
- Palmieri-Smith R, Hopkins J, Brown T (2009) Peroneal activation deficits in persons with functional ankle instability. The American Journal of Sports Medicine 37(5): 982-988.
- Batdek R, Zdolsek A, Stroinik V, Dolened A (2018) Peroneal muscle activity during different types of walking. J Foot Ankle Res 11(50).
- Wang X, Rosenberg S, Michael B. Mechlin, Mark E (2005) normal variants and diseases of the peroneal tendons and superior peroneal retinaculum: MR imaging features. Radiographics 25(3).
- Cifuentes-DPC, Pasapula C, Gutierrez NB, Larrainzar GR, Bayod J (2021) Peroneus longus overload caused by soft tissue deficiencies associated with early adult acquired flatfoot: a finite element analysis. Clinical Biomechanics 86: 105383.
- Edama M, Takabayaashi T, Hirabayashi R, Yokota H, Inai T, et al. (2020) Anatomical variations in the insertion of the peroneus longus tendon. Surgical and Radiologic Anatomy 42(10): 1141-1144.
- Zhang X, Pauel R, Deschamps K, Jonkers I, Vanwanseele B (2019) Differences in foot muscle morphology and foot kinematics between symptomatic and asymptomatic pronated feet. Scand J Med Sci Sports 29(11): 1766-1773.
- Johnson C, Christensen J (1999) Biomechanics of the first ray. Part I. The effects of peroneus longus function: A three-dimensional Study on a Cadaver Model. J Foot Ankle Surg 38(4): 313-321.
- Mendez RG, Guzman VR, Valencia O, Watanabe K (2021) Contribution of the peroneus neuromuscular compartments to eversion and plantarflexion of the ankle.
- Barn R, Rafferty D, Turner D, Woodburn J (2012) Reliability study of tibialis posterior and selected leg muscle EMG and multi-segment foot kinematics in rheumatoid arthritis associated pes planovalgus. Gait & Posture 36(3): 567-571.
- Park J, Kim D, Kwan H, Lee M, Choi Y, et al. (2021) A new anatomical classification for tibialis posterior tendon insertion and its clinical implications; A cadaveric study. Diagnostics 11(9): 1629.
- Lhoste Trouilloud A (2012) The tibialis posterior tendon. J Ultrasound 15(1): 2-6.
- Ikpeze T, Brodell J, Chen R, Oh I (2019) Evaluation and treatment of posterior tibial tendon insufficiency in the elderly patients, Geriatr Orthop Surg Rehabil.
- Shavelson D. Personal
- Campbell J (2000) Tendon transfers for posterior tibial tendon Techniques in Orthopaedics 15(3): 174-182
- Steb H, Marzano R (1999) Conservative management of posterior tibial tendon dysfunction, subtalar joint complex, and pes planus deformity. Clin Podiatr Med 16(3): 439-451.
- Shavelson D. A biomechanical paradigm shift: part I: Transforming lower extremity biomechanics terminology, nomenclature and science as an upgrade to “STJ neutral” and “normal” biomechanics. Journal of Bioengineering and Biosciences 1(5).
- Shavelson D. Wellness biomechanics kinesiology and kinetics.
- Smith R, LIchwark G, Kelly L (2021) The energetic function of the human foot and its muscles during accelerations and decelerations. J Ep Biol 224(13).
- shavelson D (1989) The foot in closed chain the future of biomechanics. Journal of Current Podiatry.
- Shavelson D (2019) The case for researching biomechanics and human movement using a stochastic model in a peer reviewed journal to generate qualitative evidence. Journal Significances of Bioengineering and Biosciences 3(1).
- Lifson SS (1940) How the community dentist can participate in a school dental program. Journal of School Health 10(8): 234-237.
© 2023 Dennis Shavelson, This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






