- Submissions

Full Text
Significances of Bioengineering & Biosciences
The Role of Hba1c in Severity and Mortality Rate of ST Segment Elevation Myocardial Infarction for Hospitalized Libyan Non-Diabetic Patients
Abdalgbar A1,2 and Altalhi KGH1*
1Faculty of Medicine University of Omar El mukhtar Albayda, Libya
2Faculty of Medical Technology University of Omar El Mukhtar Albayda, Libya
*Corresponding author:Altalhi KGH, Faculty of Medicine University of Omar El mukhtar Albayda, Libya
Submission: October 04, 2019 Published: November 27, 2019

ISSN 2637-8078Volume3 Issue5
Abstract
Background: The severity of coronary artery disease (CAD) is directly related to the quality of glucose control in diabetic patient. Additionally, diabetes is associated with increased mortality following acute myocardial infarction compared to general population.
Objectives: To evaluate the association of HbA1c level and severity of CAD, and outcome of non-diabetic patient with STEMI in our hospital.
Patients and methods: 60 consecutives non-diabetic patient with acute ST elevation myocardial infarction were treated with thrombolytic therapy included in the present prospective study. Blood glucose and HbA1c level of all patients were measured within 3 hours of admission. Patient were divided into 3 groups according to HbA1c level: with cut-off 6.5% as diagnostic criteria of diabetes mellitus according to (American diabetes association) group (1) 6.5%, group (2) 6.5 to 8.5%, group (3) 8.5% and above, in hospital. Mortality and morbidities of acute STEMI were compared between groups.
Result: The mean age was 63±15 year and mean body mass index was 26.6±6 kg/m², 24 patients (40%) had history of hypertension, 27 patients (45%) of dyslipidemia, 36 patients (60%) were smoker. We found 45 patients with HbA1c≤6.5%, 5 patients with HbA1c 6.5-8.5%, 10 patients with HbA1c≥8.5%. There was strong correlation between admission of HbA1c and admission glucose level (P<0.001). Infarct size as measured by peak creatinine kinase, was not correlated with HbA1c level.
Conclusion: HbA1c is an important risk marker in the absence of history of diabetes mellitus in patients with AMI. The optimal management in these patients may contribute in decrease hospital mortality.
Keywords: Glycosylated hemoglobin (HbA1c); ST elevation myocardial infarction (STEMI); Mortalities; Diabetes
Introduction
Patients with diabetes are at 3-4 times increased risk for cardiovascular mortality compared with non-diabetes [1]. In acute coronary syndrome, glucose metabolism is modified, and stress hyperglycemia commonly occur secondary to increase catecholamine level [2]. In addition to the higher rate of acute ST- elevation myocardial infarction (STEMI) in diabetes, hyperglycemia is associated with poor prognosis in these patients [3]. Higher HbA1c level was associated with high cardiovascular disease and death [4]. There were some other studies supporting the association between admission serum HbA1c level and increased long-term mortality of non-diabetic patients admitted with STEMI and higher rate CAD in these patients [5]. We have evaluated the association of admission level of HbA1c with the hospital outcome of non-diabetic patient with STEMI.
Patients and methods
All patients of both sexes sustaining acute ST elevation myocardial infarction without diabetes were including in the study. Patients with sepsis, hemoglobinopathies or hypothyroidism, tumor, connective tissue diseases, those with sub-acute or chronic MI (longer than 48hr between first symptom and admission) those with renal failure, hepatic failure, iron deficiency anemia and those with past history of diabetes or used anti diabetic medication were excluded from the study. Acute myocardial infarction was defined according to the (European Society of Cardiology and American College of Cardiology Criteria). Increased creatine kinase predominantly in the myocardial band fraction and or increased troponin I (creatine kinase 400U/L or higher and or cardiac troponin I 2μg/L or higher), ischemic symptoms (mainly constrictive chest pain, lasting longer than 30min), and or abnormal electrocardiography (ST elevation 1mm or greater on at least two derivation). MI was defined as acute if the time elapsed between the first symptom and admission was 48hr or less only patients who underwent thrombolytic treatment were included in the study.
All patients were in cardiac care unit, a brief history was obtained from each patient presenting with acute chest pain including presence of risk factors like smoking and hypertension, dyslipidemia and previous history of ischemic heart disease. Clinical examination was done emphasis on signs of cardiac failure, 12 leads electrocardiography (ECG) was done at cardiac care unit and blood sample were sent to laboratory, blood glucose and HbA1c level of all patients were measured within 3hr of admission regardless of whether they had been fasting or not and for cardiac enzyme. The fasting lipid profile was determined on the morning following admission and included total cholesterol, high density lipoprotein and triglyceride. All patients were considered for thrombolytic therapy (Injection streptokinase 1.5 million units over one hour) in the absence of all contraindication the management was according to standard treatment protocol. All patients underwent continues ECG monitoring for at least 48 hours on admission to cardiac care unit and daily during hospital stay.
Patients were divided into three groups according to the level of HbA1c with cut-off 6.5% as diagnostic criteria of diabetes mellitus according to (American Diabetes Association 2010) for diagnosis and classification of diabetes mellitus. Patient with HbA1c level of 4.5% to 6.4% group (1), patients with HbA1c level 6.5% to 8.5% group (2) and patients with HbA1c level higher than 8.5% group (3). None of these patients received glucose, Insulin or potassium infusion therapy during admission. All subjects were hospitalized one week after acute myocardial infarction and hospital records were reviewed at this time. Selective coronary angiography was performed after 1 month. Coronary angiogram was analyzed by two experienced observers who were blinded to the identities and clinical information of the patients. Vessel scores were ranged from zero to three, according to the number of diseased major pericardial vessel with significant stenosis (greater than 50% stenosis of the lumen diameter). Statistical analysis: Was performed by using SPSS software (Version 12) difference among groups was analyzed by (t-test) and P value 0.05 was considerable significant.
Result
(Table 1) Total 60 patients with (STEMT) were studied. Patients were divided on the bases of admission HbA1c group (1)≤6.5%; group (2) 6.5-8.5%; group 3≥8.5%. The clinical and biological characteristic according to HbA1c are summarized in (Table 1). The mean age was 63±15 year and mean body mass index was 26. 6±6kg/m², 24(40%) had history of hypertension, 27(45%) of dyslipidemia, 36(60%) were smoker. We found 45 with HbA1c≤6.5%; 5 with HbA1c 6.5-8.5%, 10 with HbA1c≥8.5%. There was strong correlation between admission HbA1c and admission glucose level (P<0.0001). Infarct size as measured by peak creatinine kinase, was not correlated with HbA1c level.
Table 1: Clinical and biological characteristics of the study subjects, according to admission HbA1c level.

Data are mean±Sd, BMI, body mass index i.e. body weight (kg)/hight²(m²). SBP/ DBP, systolic/diastolic blood pressure; CK: Creatinine Kinase.
(Table 2) Patients were divided according to admission glucose group (1), 6.9mmol/L; group (2), 7 to 8.1mmol/L; group (3), 8.2 to 9.5mmol/L; group (4), ≥9.6mmol/L. There was significant positive correlation between admission glucose and infarct size measured by peak creatinine kinase level (P<0.0001). (Table 3) At the end of fourth week coronary angiography performed in remaining 54 patients, revealed that there was significant correlation between HbA1c level at admission and number of disease vessel (P=0.001). (Table 4) We found that patients who died by day 5 were significantly different from patients with non-lethal acute myocardial infarction, with regard to admission plasma glucose (16.6±5.4 vs 8.3±3.4mmol/L, P=0.0001) age (74±10 vs 62±13 year, P=0.002). There was no significant difference in HbA1c value in the survivor and non-survivor (6.7±1.8 vs 6±0.2, P=0.15).
Table 2: Clinical outcome of non-diabetic patients based on quantities of admission plasma
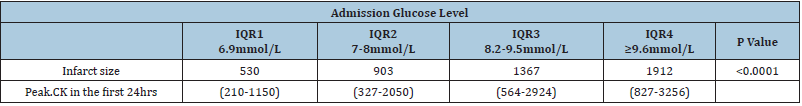
IQR =Interquartile Range; CK= Creatinine Kinase
Value are expressed as median (IQR).
Table 3:Angiographic data of patients according to HbA1c.
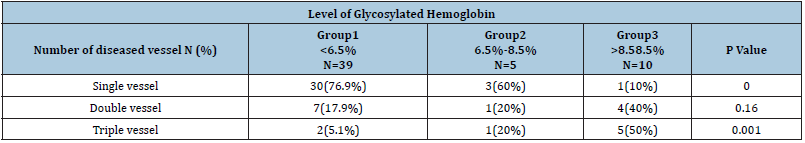
Table 4:Clinical characteristics of patients according to the mortality at 5 days after acute myocardial infarction.

HbA1c=Glycosylated Hemoglobin.
Discussion
The present study confirms previous observation in diabetic subjects suggesting that higher glucose level during AMI are associated with increased mortality [6]. In recent study, [5] reported that higher admission glucose level in non-diabetic patients treated with reperfusion therapy for ST segment elevation MI were associated with significantly larger enzymatic infarction size and lower left ventricular ejection fraction. This is because a stress response is accompanied by high level of catecholamine and cortisol and these hormones increase glycogenolysis and lipolysis and reduce insulin sensitivity, resulting in elevated glucose level [7]. There for, patients with elevated glucose level may represent with an increased stress response, due to more sever hemodynamic compromise or more extensive myocardial damage [8,9]. Elevated cytokine, particularly tumor necrosis factor-Alpha (TNF-α), also increase glucose level. TNF-α is released in AMI and directly decrease myocardial contractility, probably by inducing myocardial apoptosis [10,11]. TNF-α also cause impaired endothelial function [12]. This in turn, may be responsible for the impaired myocardial perfusion. We found positive correlation between peak creatinine kinase and admission plasma glucose concentration in our patients. Conversely, no correlation was found with HbA1c value. Although acute hyperglycemia at admission and during stay has clearly been associated with adverse outcome in patients with acute MI [13,14,5].
Our study shows admission HbA1c level are not associated
with high mortality in non-diabetic STEMI population treated with
streptokinase. In our study high HbA1c in non-diabetic patients
associated with multi vessel involvement of coronary arteries.
Similarly [15] reported a significant correlation between HbA1c
level at admission and positive exercise that result after the four
weeks follow up. Hyperglycemia in STEMI patients was strongly
associated with increased mortality within 5 days although there is
clear correlation between admission glucose and HbA1c level, they
appear to represent related but different phenomena. Patients with
elevated glucose level have larger MI area. Recently a prospective
cohort study showed that in non-diabetic general population,
as elevated HbA1c level is a risk factor for the development of
cardiovascular events independently of fasting glucose [4]. The
international expert committee recommended the use of HbA1c in
diagnosis diabetes with a cut-off 6.5% [16].
The advantage of HbA1c over the fast blood glucose are its
lower intra-individual variability, assessment in non-fasting state
and superior in monitoring blood glucose level [4,17]. Preiss et al.
[1], and Selvin et al. [4] has suggested that glycosylated hemoglobin
is superior to fasting blood glucose in predicting long-term risk of
CAD in non-diabetes. Similar result is reported by Park et al. [18]
and colleagues among non-diabetic women. In a cohort of European
men [19] and colleagues reported that HbA1c correlates linearly to
subsequent cardiovascular morbidity [19]. The American Diabetes
Association suggests that individual with HbA1c concentration of
5.7-6.4% should be informed of their increased risk for diabetes as
well as cardiovascular disease [17].
Conclusion
HbA1c is an important risk marker in the absence of history of diabetes mellitus in patients with AMI. The optimal management in these patients may contribute in decrease hospital mortality [20- 25]. People at high risk for type II diabetes mellitus should receive lifestyle counseling and if needed pharmacological therapy to reduce their risk of developing hyperglycemia and type II diabetes mellitus but specially to prevent or slow the development of CAD [26,27].
References
- Hwang PS, Coady S, Pencina S, Agostino MD, Savage PRS, et al. (2009) Trends in all-cause and cardiovascular disease mortality among women and men with and without diabetes mellitus in the-framingham Heart study, 1950 to 2005. Circulation 119(3): 1728-1735.
- Husband DJ, Alberti KG and Julian DG (1983) Stress hyperglycemia during acute myocardial infarction: an indicator of pr-existing diabetes. Lancet 2(8343): 179-181.
- Wahab N, Cowden E, Pearce N, Gardner M, Merry H, et al. (2002) Is blood glucose an independent predictor of mortality in acute myocardial infarction in the thrombolytic era. J Am Coll Cardiol 40(10): 1748-1754.
- Selvin E, Streffes M, Zhu H, Matsushita K, Wagenknecht L, et al. (2010) Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med 362(9): 800-811.
- Timmer J, Hoekstra M, Nijsten M, Horest ICV, Ottervanger JP, et al. (2011) Prognostic value of admission glycosylated hemoglobin and glucose in nondiabetic patients with ST-segment-elevation myocardial infarction treated with percutaneous coronary intervention. Circulation 124(6): 704-711.
- Sewardsen M, Vythilingum S, Jailal I, Becker PJ (1989) Prognostic importance of admission plasma glucose in diabetic and nondiabetic patients with acute myocardial infarction. Q J Med 71(265): 461-6.
- Seaquist ER, Anderson J, Childs B, Cryer P, Jack DS, et al. (2013) Hyopglycemia and diabetes: a report of a workgroup of the American Diabetes Association and Endocrine Society. Diabetes Care 36(5): 1384-1395.
- Gosselink AT, Liem AL, Reiffers S, Zijlstra F (1998) Prognostic value of predischarge radionuclide venrticulography at rest and exercise after acute myocardial infarction treated with thrombolytic therapy or primary coronary angioplasty. The Zwolle myocardial infarction study group. Clin Cardiol 21(4): 254-60.
- Geare DVS, Boura JA, Grines LL, Neill WW, Grines CL (2001) Predective value of the killip classification in patients undergoing primary precutaneous coronary intervension for acute myocardial infarction. Am J Cardiol 87(9): 1035-8.
- Li D, Zhao L, Liu M, Du X, Ding W, et al. (1999) Kinetics of tumor necrosis factor alpha in plasma and the cardioprotective effect of monoclonal antibody to tumor necrosis factor alpha in acute myocardial infarction. Am heart J 137(6): 1145-52.
- Li YP, Reid MB (2001) Effect of tumor necrosis factor-alpha on skeletal muscle metabolism. Curr Opin Rheumatol 13(6): 483-7.
- Fujita H, Morita I, Murota S (1999) A possible involvement of in transporter in tumor necrosis factor alpha and cycloheximide-induced a apoptosis of endothelial cells. Mediators Inflamm 8(4-5): 211-8.
- Capes S, Hunt D, Malmberg K, Gerstein H (2000) Stress hyperglycemia and the risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet 355(9206): 773-778.
- Norhammar A, Tenerz A, Nilsson G, Efendic S, Ryden I (2002) Glucose metabolism in patients with myocardial infarction and no previous diagnosis of diabetes mellitus: A prospective study. Lancet 359(9324): 2140-2144.
- Cakmak M, Cakmak N, Cetemen S, Tanrverdi H, Teskin O, et al. (2008) The value of admission glycosylated hemoglobin level in patients with acute myocardial infarction. Can J Cardioln 24(5): 375-378.
- Gillett M (2009) International expert committee report on the role of the HA1c assay in the diagnosis of diabetes: Diabetes Care 2009;1327-1334. Clin Biochem Rev 30(4): 197-200.
- American Diabetes Association (2010) Diagnosis and classification of diabetes mellitus. Diabetes care 33(Suppl 1): S62-S69.
- Park S, Connor BE, Wingard D, Shan J, Edelstein S (1996) GHB is better predictor of cardiovascular disease than fasting or post challenge plasma glucose in women without diabetes. The Rancho bernardo Study. Diabetes Care 19(5): 450-456.
- Khaw K, Wareham N, Luben R, Bingham S, Oakes S, et al. (2001) Glycated haemoglobine, diabetes and mortality in men in Norfolk cohort of european peospective investigation of cancer and nutrition (EPIC-Norfolk). BMJ 322(7277): 15-18.
- Ashra FH, Boroumand MA, Amirzadegan A, Talesh SA, Davoodi G (2013) Hemoglobin A1C in nondiabetic patients an independent predictor of coronary artery disease and its severity. Diabetes Res Clin Pract 102(3): 225-232.
- (1996) The absence of a glycemic threshold for the development of long-term complications the perspective of the Diabetes Control and Complications trial. Diabetes 45(10): 1289-1298.
- Gerrity R, Natarajan R, Nadler J, Kimsey T (2001) Diabetes induced accelerated atherosclerosis in swine. Diabetes 50(7): 1654-1665.
- Ghaffari S, Nadiri M, Pourafkari L, Sepehrvand N, Movasagpoor A, et al. (2014) The predictive value of total neutrophil count and neutrophil/lymphocyte ratio in predicting in- hospital mortality and complications after STEMI. J Cardiovascular Thorac Res6(1): 35-41.
- Kassaian SE, Goodarznejad H, Boroumand MA, et al. (2012) Glycosylated hemoglobin (HbA1c) level and clinical outcomes in diabetic patients following coronary artery stenting. Cardiovascular Diabetology 11: 82.
- Pai J, Cahill L, Hu F, Rexorde K, Manson J, et al. (2013) Hemoglobin a1c is associated with increased risk of incident coronary heart disease among apparently healthy, nondiabetic men and women. J Am Heart Assoc 2(2): e000077.
- The Joint European Society (2000) Cardiology/American college of cardiology Committee for the Redefinition of myocardial infarction myocardial infarction redefined-a consensus document. Eur Heart J 21: 1502-1513.
- Wiviott S, Braunwald E, Angiolillo D, Meisel, S, Dalby A, et al. (2008) Greater clinical benefit of more intensive oral antiplatelet therapy with prasugrel in patients with diabetes mellitus in the trial to assess improvement in therapeutic outcomes by optimizing platelet inhibition with prasugrel-thrombolysis in myocardial infarction 38. Circulation, 118(16): 1626-1636.
© 2019 Altalhi KGH. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






