- Submissions

Full Text
Research in Pediatrics & Neonatology
Aqueduct of Sylvius Stenosis: A Case Report
Codey Pedersen* and Yaron Ivan
Medical Doctor, Department of Health, USA
*Corresponding author: Codey Pedersen, Medical Doctor, Department of Health, USA
Submission: February 08, 2024; Published: March 26, 2024

ISSN: 2577-9200 Volume8 Issue2
Abstract
MESH: Aqueduct of sylvius, aqua ductal web, hydrocephalus, ataxia, CSF blockage The Aqueduct of Sylvius is the narrowest portion of the path of Cerebrospinal Fluid (CSF) in the brain and connects the third and fourth ventricles [1]. It is therefore the most common site of interventricular blockage of CSF [2]. Rarely (approximately 1 in 5000) children are born with a congenital blockage of the aqueduct, which can have serious clinical consequences. We present a case of an 11-year-old male who presented to the ED with two weeks of declining motor function, ataxia, and confusion as well as three months of intermittent headaches, subsequently shown to be caused by hydrocephalus due to an aqueductal web.
Introduction
The Aqueduct of Sylvius is the narrowest portion of the path of Cerebrospinal Fluid (CSF) in the brain, and connects the third and fourth ventricles [1]. It is therefore the most common site of interventricular blockage of CSF [2]. Rarely (approximately 1 in 5000) children are born with a congenital blockage of the aqueduct, which can have serious clinical consequences. When the aqueduct is blocked it can lead to significant accumulation of CSF and an increase in ventricular pressure leading to compression of the brain, and numerous symptoms. A majority of congenital cases present in utero or in neonates due to the hydrocephalus caused from the buildup of CSF [3]. However, secondary to compensation mechanisms, some patients do not become symptomatic until physiologic increases in CSF production during adolescence [3]. We present a case of an 11-year-old male who presented to the ED with two weeks of declining motor function, ataxia, and confusion as well as three months of intermittent headaches, subsequently shown to be caused by hydrocephalus due to an aqueductal web.
Case Report
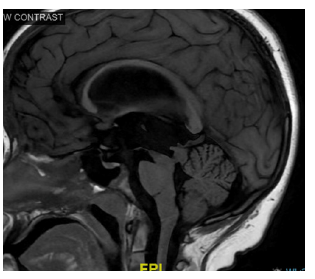
An 11-Year-old male with no significant past medical history who was up to date on vaccinations presented to the ED with a two-week history of worsening ataxia, dizziness, multiple falls, and loss of fine motor skills. His course of illness began two months prior with intermittent headaches and a rapid decline of fine motor skills and worsening ataxia acutely over the week prior to presentation. Review of systems was significant for one episode of urinary incontinence, and loss of memory as the previous week had progressed. Physical exam was as follows, heart rate of 85bpm, Blood Pressure of 110/60mm/hg, respiratory rate 20bpm and 98% O2 saturation on room air. The Patient had a positive rhom burg sign, ataxic gate, ataxic finger to nose and vertical nystagmus. Labs were significant for WBC of 8.310^3/ul (4.0- 10.8 10^3/ul), Hgb 13.6g/dL (11.5-16.0g/dL), Hct 40.4 % (35%-47%), PLT Count 319, Sodium of 137mmol/L (137-145mmol/L, Potassium of 4.6mmol/L(3.5-5.0mmol/L), Chloride 109mmol/L (95-107mmol/L), Carbon Dioxide 24mmol/L (22-30mmol/L), BUN 9mg/dL(7- 17mg/dL), Creatinine of 0.50 mg/dL(0.50-1.30mg/dL) and Glucose of 122mg/dL (70-100mg/ dL). Computer tomography (CT) of the brain was obtained in the emergency room due to the concerning history and physical exam findings and was significant for hydrocephalus secondary to suspected aqueductal stenosis (Figure 1A, B). Subsequently the patient was admitted and had Brain Magnetic Resonance Imaging (MRI) which indicated severe obstructive hydrocephalus with severe dilation of the lateral and third ventricle, with no dilatation of the 4th ventricle and soft tissue in the region of the aqueduct concerning for a web (Figure 2). On the next day the patient was evaluated in the operating room by Neurosurgery. Using neuro-endoscopy, they identified an extremely small pinhole present in the aqueduct, allowing minimal passage of CSF. An endoscopic third ventriculostomy was performed, opening a small hole in the floor of the 3rd ventricle between the infundibular recess and mamillary bodies, and using a Fogarty balloon to dilate this. This allowed CSF communication with the pre-pontine subarachnoid space. On subsequent re-evaluation at the two-week follow-up with Neurosurgery the patient had complete resolution of his symptoms.
Figure 1A:Axial CT Showing enlarged Ventricles and hydrocephalus with suspected aqua ductal stenosis.
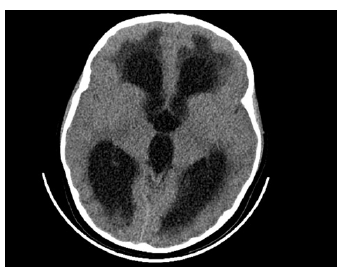
Figure 1B:Axial CT Showing enlarged Ventricles and hydrocephalus with suspected aqua ductal stenosis.
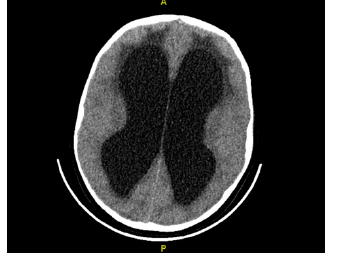
Figure 2:Brain Magnetic Resonance Imaging(MRI) which indicated severe obstructive hydrocephalus with severe dilation of the lateral and third ventricle, with no dilatation of the 4th ventricle and soft tissue in the region of the aqueduct concerning for a web.
Discussion
Etiology
Hydrocephalus is the most common disease treated by pediatric neurosurgeons and is responsible for approximately $2 Billion in health costs per year [4,5]. It is a common disorder of CSF physiology resulting in fluid backup, increased ventricle size, and increased intracranial pressure. Studies have shown genetic factors contribute to both syndromic and non-syndromic forms of hydrocephalus, with the focus of this discussion being non syndromic [4]. Three genes have been linked to non-syndromic congenital hydrocephalus in humans and most are due to some common heritably form of aqueduct stenosis [5]. Mutations in genes coding for cell adhesion molecules, tight junction proteins and cell migration regulators are the culprit gene mutations which cause the stenosis [4,5]. Intraventricular blockage of CSF due to cerebral aqueduct web is a rare congenital abnormality that can lead to severe neurologic symptoms due to the backup of CSF and hydrocephalus causing increased Intra-cranial pressure.
Clinical presentation
Most congenital cases of aqueductal stenosis, and hydrocephalus present in infancy with progressive macrocephaly, feeding intolerance, irritability, vomiting, bulging fontanels, developmental delay, or if part of a syndrome with other syndromic components [4,5]. If there is a known family history or a known carrier, prenatal ultrasound can detect ventriculomegaly as early as fetal age of 20 weeks’ gestation [4]. However, some patients present later in adolescence depending on differences in flow dynamics and degree of stenosis, and obstruction. When presenting later, patients have signs and symptoms which often include extensive headaches followed by progressive neurologic symptoms such as ataxia, papilledema vision changes, nausea, vomiting, mental status changes, and memory changes [4].
Treatment
The most common management of all hydrocephalus including aqueductal stenosis has been placement of a CSF shunt, which diverts CSF from the ventricles into the peritoneal cavity [4]. However, since the early 1990s there has been increase in the use of endoscopic treatment for hydrocephalus which involves putting an endoscope into the frontal horn of the lateral ventricle through the foramen of Monro and into the third ventricle where an opening is made enabling communication into the prepontine cistern [4]. This is similar to the procedure performed on the case presented. If corrected via neurosurgery either through shunt placement or endoscopic resection, most patients have good outcomes with complete resolution of symptoms. Emergency medicine physicians hold a crucial role in the recognition, diagnosis and treatment plan of obstructive hydrocephalus. As in this case it is important to hold a low threshold for imaging and extensive workup when neurologic symptoms are involved. Headaches although a common chief complaint often have classic symptoms of migraine and when these aren’t present it is important to consider alternative diagnoses. Acute onset headaches with no history or obvious cause that are persistent require a more extensive workup. The key to diagnosis is a thorough physical exam and low threshold for imaging. As in this case, if identified early patients can have complete resolution of symptoms with minimal/no complications or residual deficits.
Summary
Hydrocephalus is a rare cause of neurologic symptoms in children, however, the most likely site of intraventricular blockage of CSF drainage is the aqueduct of Sylvius. Most cases present in infancy with progressive macrocephaly, feeding intolerance, irritability, vomiting, bulging fontanels, developmental delays, or if part of a syndrome with other syndromic components [4,5]. However, flow dynamics, and non-complete obstruction can cause some patients to present later in life such as the case presented here. Late presentations often have symptoms similar to this case, extensive headache history, followed by progressive neurologic symptoms including ataxia, vision changes, nausea, vomiting, mental status changes, and memory changes [4]. A rare cause of aqueductal blockage is an aqueductal web which is seen in this case. Patient with webs can have severe symptomatic consequences, which can be treated with neurosurgical intervention through placement of a VP shunt, or endoscopic CSF diversion.
Acknowledgement
The authors thank Todd Hankinson, MD, Pediatric Neurosurgeon at the Children’s Hospital of Colorado for editing several drafts of the manuscript.
References
- Zarei F, Zeinali RB, Iranpour P, Sefidbakht S (2022) A case of aqueductal obstruction by web with no sign except a headache. Radiol Case Rep 17(10): 3767-3769.
- Cinalli G, Spennato P, Nastro A, Aliberti F, Trischitta V, et al. (2011) Hydrocephalus in aqueductal stenosis. Childs Nerv Syst 27(10): 1621-4162.
- Flora N (2005) Compensated aqueduct of Sylvius obstruction by web-a case report. Indian Journal of Radiology and Imaging 15(1).
- Kahle KT, Kulkarni AV, Limbrick DD, Warf BC (2016) Hydrocephalus in children. Lancet 387(10020): 788-799.
- Simon TD, Riva CJ, Srivastava R, Bratton SL, Dean JM, et al. (2008) Hospital care for children with hydrocephalus in the United States: Utilization, charges, comorbidities, and deaths. J Neurosurg Pediatr 1(2): 131-137.
© 2024 Codey Pedersen. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






