- Submissions

Full Text
Research in Pediatrics & Neonatology
Current Issues of Modern Pediatric Anesthesiology in the Conditions of Combined Epidural Anesthesia in Children
Fayziev OY*, Satvaldieva EA, Yusupov AS and Abzalova MY
Department of Anesthesiology and Resuscitation, Pediatric Anesthesiology and Resuscitation, Tashkent Pediatric Medical Institute. Tashkent, Uzbekistan
*Corresponding author: Fayziev OY, Department of Anesthesiology and Resuscitation, Pediatric Anesthesiology and Resuscitation, Tashkent Pediatric Medical Institute. Tashkent, Uzbekistan
Submission: February 12, 2024; Published: March 18, 2024

ISSN: 2577-9200 Volume8 Issue2
Abstract
Introduction: In pediatrics, the study of pain has also become a highly relevant task, which is intensively
studied in the framework of pediatric surgery, oncology, anesthesiology, neurology, cardiology,
gastroenterology, rheumatology, not counting palliative medicine, age-related physiology.
Method and materials: The study was conducted in the postoperative period in 34 patients after abdominal
surgery. For an objective assessment of the effectiveness of anesthesia, the following research methods were
carried out: A clinical study with the determination of the intensity of pain on a Visual Analogue Scale (VAS)
and the determination of blood pressure, blood pressure, pulse oximetry and echocardiographic study of
central hemodynamic parameters.
Result: Studies of the clinical picture of the course of the postoperative period with monitoring of blood
pressure, oxygen saturation, pulse oximetry, studies of the subjective assessment of pain intensity according
to VAS and an echocardiographic method for studying central hemodynamic parameters showed the relative
stability of patients after adequate pain relief. The use of a combination of drugs: Infulgan - develops an
early analgesic effect, while tramadol realizes its action later, provides prolongation of analgesia. Tramadol
with infulgan in analgesic effect several times exceeded ketorolac.
Conclusion: Multimodal epidural analgesia based on bupivacaine at a dose of 1.0mg/kg reduces early
postoperative complications, promotes rapid rehabilitation and recovery. Pain and its equivalents are one of
the most common reasons for children seeking medical help [1,2]. Postoperative pain syndrome is associated
with the action of a pathogenic irritant and is characterized by subjectively unpleasant sensations, as well
as significant changes in the body, up to serious disruption of its vital functions [3-9]. Pain affecting a child’s
body as a phenomenon of the somatosensory sphere can be accompanied by motor, autonomic, affective
and other manifestations. Almost everyone who has undergone abdominal surgery is characterized by the
occurrence of postoperative pain syndrome, the relief of which improves the quality of life of patients [10-
13]. Pain management is a very important task that must be addressed after surgery. Early rehabilitation is
facilitated by effective pain relief for the patient. It reduces postoperative complications and chronic pain
syndromes [13,14]. Pain as a syndrome is characterized by varying severity and in the vast majority of cases
(more than 80-90%) is accompanied by emotional, psychological and mental disorders. There are many
medications and methods for postoperative pain relief. But, as many different studies in many countries
show, in the early postoperative period, almost half of the patients experience insufficient analgesia [15-
18]. Elimination of pain is a priority in organizing treatment, otherwise a situation arises of treating not
the patient, but the disease. Invasive techniques (spinal cord stimulation, deep brain stimulation and
motor cortex stimulation) are used in neurological clinics [19]. For severe pain in seriously ill children,
epidural anesthesia or intravenous drip administration of analgesics is used, but these methods require
the supervision of an anesthesiologist. It is very important to use effective, optimal epidural analgesia
with the use of bupivicaine, which can be provided to the greatest extent in accordance with the principle
of a multimodal approach: “maximum effect - minimum side effects” [20]. Children do not have special
mechanisms for pain tolerance, but reflex nerve pathways and mediators of the feeling of pain are already
present at the stage of intrauterine development. Children, unfortunately, do not always clearly characterize
the intensity of pain reactions and may tell lies for completely objective reasons [21,22].
Purpose of the work: To increase the effectiveness and safety in the postoperative period undergoing
abdominal surgery by introducing epidural analgesia in children.
Keywords:Urinary tract infections; Pathogen; Escherichia coli; Urinary cultures; Antibiotic resistance
Method and Materials
The study was carried out in the postoperative period in 34 patients after urological operations. Children 7-10 years old made up 70.6% of the total number of patients. Children from 11 to 15 years old were 29.4%. Of all patients, 55.9% were boys and 44.1% were girls. To objectively assess the effectiveness of anesthesia, research methods such as a clinical study with determination of pain intensity using a visual analogue scale (VAS) were used. A Japanese echocardiograph “Aloka SSD-260” with a 3.5MHz sensor was used for the study. Echocardiographic data were calculated automatically. Five parameters were determined. The first two are the end-diastolic and systolic volumes of the left ventricle (EDV and ESV, respectively). Cardiac stroke volume (SV) was calculated as the difference between EDV and ESV (in ml), and ejection fraction was calculated as the ratio of ESV to EDV (in %). The fifth parameter was the fraction of circular shortening of the anteroposterior dimension of the left ventricle of the heart. Determination of blood pressure, blood pressure, pulse oximetry and echocardiographic study of central hemodynamics. Some hemodynamic parameters were correlated with the body surface area (S) of the patients, which was determined depending on height and body weight. Statistical processing of the obtained results was carried out using the method of mathematical statistics with the student’s criterion. In the first group, postoperative patients received epidural analgesia with bupivacaine at a dose of 0.5%- 1mg/kg, every five hours for pain symptoms. In the second group, when pain occurred, promedol was used every six hours at a dose of 1mg/kg body weight, as planned.
The clinical course of the condition of patients with subjective assessment of pain intensity according to VAS was studied. Hemodynamics were recorded at the first stage during pain, at the second and third -30 minutes and 60 minutes after anesthesia, respectively, as well as at the fourth -two hours after anesthesia and the fifth - after five hours.
Result
In the first group of children in the early postoperative period, pain did not develop for 5.3 ± 0.5 hours, this is due to intraoperative anesthesia with bupivacaine using the method of multimodal anesthesia and analgesia. The clinical course of the first group with EA + bupivacaine can be judged from Table 1. Half an hour after the administration of bupivacaine into the epidural space, not a single child complained of pain. There was no pain in the wound; coughing and deep breathing were painless. There were no reactions in the patients’ behavior indicating pain. The VAS pain intensity score was 1.28±0.16 points. This is statistically significant in relation to the previous stage (P<0.01). Clinical parameters were also stable. An hour after pain relief, the condition stabilized. Activity increased, there were no complaints, the children moved in their beds without any pain in the wound. Hourly urine output increased to 32.3±5.2ml/hour. The patients felt much better, their appetite and positive emotions appeared. The intensity of pain according to VAS decreased to 0.5±0.05 points. Patients exhibited a motionless body position - 20.3%, a defensive reaction - 25.9%, a wrinkled forehead - 25.9% and sobbing in 20.3%. Two hours after the start of pain relief, a decrease in RR, heart rate, and blood pressure system was noted and diast. These figures were 14.7%, 11.5%, 9.7%, 15.8%, respectively. An hour after anesthesia, 90.7% of patients did not feel pain at rest; 75.9% did not feel pain during movement, coughing and palpation. Only 24% of patients experienced pain during active coughing, which did not worsen the general well-being of the patients. The sedative effect persisted in 62.9% of patients. Behavioral reactions decreased: Defensive actions - 18.5%, wrinkled forehead - 16.6%, sobbing - 16.6%. Motor activity is preserved. Pain intensity according to VAS was assessed as 0.4±0.08 points. RR and heart rate indicators continued to decrease, blood pressure remained stable compared to the previous stage. Reduced in comparison with the initial values were RR, heart rate, and blood pressure system and diast. These figures decreased by 16.2%, 15.6%, 13.8% and 17.5%, respectively. Hourly diuresis remained virtually unchanged: 32.8 ± 4.5ml/hour.
Table 1:Changes in central hemodynamic parameters during postoperative anesthesia with EA+.

Note: * - reliability of differences in indicators in relation to the first stage of the study.
Five hours after anesthesia, one child found it painful to move and breathe deeply. The intensity of pain according to VAS was at the same level as before - score. Hourly diuresis was also normal - 36.2 ± 6.8ml/hour. The duration of pain relief was 5.3 ± 0.42 hours. Thus, the clinical course of EA analgesia provides a clear analgesic effect. Effective and adequate pain relief was observed in 98% of children. During the study, the cardiac index and UI changed slightly. At the fifth stage of the study, the SI indicator was characterized by a tendency to decrease (5.3%). Throughout the study, the pumping function of the heart was stable and FI indicators remained almost unchanged. Changes in MDD showed a tendency towards a gradual slight decrease: from 76.75 ±2.22 at the time of anesthesia to 71.75 ±1.5 4 hours after anesthesia. At the beginning of anesthesia, SRL decreased by 12.5%, compared to the initial data, but after an hour it increased to 18.10±2.77. This figure is 3.1% higher than similar data obtained at the previous stage.
By the fifth hour, the SAR decreased slightly - by 5.9%. The most common were defensive actions (44.4% of observations) and a stationary body position (50%). If we analyze the facial expression, the teeth were clenched (37%), lips were tightly compressed (33.3%), and the forehead was wrinkled (33.3%). In addition, crying, screaming (20.3%) and sobbing (33.3%) were observed. The average VAS pain intensity score was 2.9±0.03 points. 15-20 minutes after administration of the drug into the epidural space, the intensity of the pain syndrome sharply decreased in 72.2% of patients (Figure 1). In the second group of children in the early postoperative period, pain did not develop for 2.2±0.6 hours. When pain occurred, the children became restless and cried and the older ones talked about pain in the wound. In the first group of patients, the clinical course after the surgical period changed as follows (see Table 1). RR was 38.2±1.92 beats per minute, heart rate was 132.8±5.9 beats per minute, systal and diastolic blood pressure was 128±5.56 mmHg. Art and 75.9±3.05mm rt. Art. Respectively (Table 2). After 30 minutes of pain relief with promedol, the children began to feel better, answered questions adequately, and did not complain of pain. There was also no pain felt in the wound; coughing and deep breathing were not painful. Behavioral reactions characterizing pain syndrome were not observed. Clinical parameters remained stable and no significant changes were noted. Heart rate decreased by -17.85% (P<0.05), blood pressure syst. by -10.55%), (BP diast by -13.31%). An hour after pain relief, the condition stabilized, there were no complaints and the children’s activity increased. They were already moving in bed and without any pain in the wound. There was also no pain felt on palpation. The RR indicator significantly decreased - to 31.2±1.87, which is 18.32% less compared to the first stage of the study. Compared to the second stage, the decrease was -1.27%. Heart rate decreased by -18.30% and amounted to 108.5±2.87 - in comparison with the first stage of the study. The ADC and ADD indicators decreased by -13.36% and -17.39%, respectively (to 110.9±3.48 and 62.7±2.23 at P <0.05).
Figure 1:Dynamics of pain intensity assessment according to VAS during postoperative analgesia with EA (bupivacaine) and promedol analgesia.
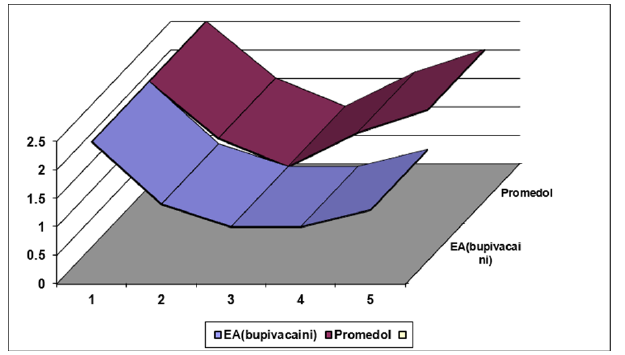
Table 2:Indicators of heart rate and blood pressure during postoperative anesthesia with promedol.

Note: * - reliability of differences in indicators in relation to the first stage of the study.
RR decreased two hours after anesthesia with promedol by -16.23% (32±1.54), heart rate - by -14.53% (113.5±2.83). There was a decrease in blood pressure by 12.81% (111.6±2.95) and blood pressure by 16.60% (63.3±2.45), and the changes were significant compared to stage 1 of the study. There was a decrease in RR by 10.21% (34.3±1.86), HR by -3.31% (128.4±2.86), AD by 7.03% (119±2.56) and ADD by 3.29% (73.4±2.15) five hours after anesthesia. Before anesthesia with promedol, the subjective assessment of pain intensity according to VAS was 2.47±0.18 points. The children answered questions adequately and did not complain of pain at rest. Their condition was stable. In the early postoperative period, 8 children (22.5%) had increased body temperature, while the rest were normal. Hourly urine output reached 24.4±4.7ml/hour. There was no pain at rest three hours after anesthesia in 91% of children. 59.2% of patients felt pain during movement, coughing and palpation, and 46.8% felt moderate pain during severe coughing and palpation of the wound, which did not worsen their general well-being and did not cause significant suffering. Maintained sedation was recorded in 22.2% of patients. The general condition and motor activity of the children improved. They tried to make themselves as comfortable as possible in their beds. They responded to manipulations and dressings painlessly. Among the behavioral reactions: immobility (25%), defensive movements (19%), wrinkled forehead (17%), sobbing (21%) were significantly reduced. The average pain intensity according to VAS reached 0.8±0.08 points. If compared with the initial indicators, they were reduced by 17.1%, 17.3%, 9%, 13.4%, respectively, RR, HR, systolic blood pressure and diast. In terms of hemodynamics and respiration, there was an increase in RR, HR, BP syst., BP diast by 5%, 12.3%, 1.2%, 4.5% compared to the previous stage, although in relation to the outcome they remained reduced by 12.9%, 7%, 7.8% and 9.4% respectively.
Discussion
Epidural blockade with bupivacaine 0.5% 1.0mg/kg was the main analgesic component in the postoperative period. The developed model in the postoperative period at this dosage helps to achieve controlled analgesia and complete pain relief. The study showed that adequate postoperative pain relief for those who have undergone abdominal surgery lasts for 5-7 hours, which also leads to a reduction in the drug load on the child’s body and increases the pharmaco-economic effect of the optimized technique. Thus, the results of a study of the clinical picture of the course of the postoperative period with monitoring of blood pressure, oxygen saturation, pulse oximetry, a study of subjective assessment of pain intensity using VAS and an echocardiographic method for studying central hemodynamic parameters showed that the relative stability of the condition of patients ensures adequate pain relief for pain syndrome after surgery in children. Subsequently, epidural blockade with bupivacaine 0.25% - 0.5-1mg/kg was used for postoperative pain relief, and the duration of the catheter in the epidural space did not exceed 3 days and did not increase the risk of infection. Pain relief with epidural anesthesia promotes an early analgesic effect. Long-term epidural anesthesia was performed for children after abdominoperineal proctoplasty, which contributed to the normalization of intestinal motility and the functioning of the gastrointestinal tract.
Conclusion
1. The use of epidural blockade in the postoperative period
for protection with 1mg/kg bupivacaine; this dose led to a
decrease in the pharmacological load on the child’s body,
reduced the likelihood of early complications by 2 times, and
helped reduce the cost of surgical treatment by 54% (2 times).
2. The developed model of epidural anesthesia as a
component of postoperative multimodal analgesia during
abdominal operations in children using bupivacaine is optimal
for the above-mentioned traumatic abdominal operations in
children. A necessary condition is mandatory practical training
of anesthesiologists to perform regional blocks in children,
knowledge of the anatomical, physiological and functional
features for its safe implementation.
3. In the early postoperative period, the resumption of pain,
on average, was recorded: 5.3±0.5 hours and 2.2±0.6 hours
after surgery, respectively, in children of groups 1 and 2, which
also emphasizes the adequacy of multi-level multimodal pain
relief + long-term analgesic effect of epidurally administered
bupivacaine.
References
- Aleksandrovich YS, Gorkovaya IA, Miklyaeva AV (2020) Effect of anesthesia in the ante-and intranatal periods of development on the cognitive status of children aged from 0 to 3 years. Annals of the Russian academy of medical sciences 75(5): 532-540.
- Agzamxodjaev TS, Fayziev OY, Yusupov AS, Turaevna NN (2020) Combined multimodal anesthesia for abdominal surgeries in children. Russian Journal of Pediatric Surgery 24(3): 188-193.
- Fayziev OY, Agzamkhodzhaev TS, Yusupov AS, Mamatkulov IA (2018) Improvement of combined multimodal anesthesia in abdominal surgical interventions in children. Russian Pediatric Journal 21(6): 362-365.
- Garin C (2020) Enhanced recovery after surgery in pediatric orthopedics(ERAS-PO). Orthop Traumatol Surg Res 106(1S): S101-S107.
- Debono B, Wainwright TW, Wang MY, Freyr GS, Michael MHY, et al. (2021) Consensus statement for perioperative care in lumbar spinal fusion: Enhanced recovery after surgery (ERAS®) society recommendations. Spine J 21(5): 729-752.
- Avila EK, Elder JB, Singh P, Xi C, Mark HB (2013) Intraoperative neurophysiologic monitoring and neurologic outcomes in patients with epidural spine tumors. Clin Neurol Neurosurg 115(10): 2147-2152.
- Banaschewski T, Christine JS, Daniel B, Jan KB, Jonna K, et al. (2012) Neuropsychological correlates of emotional lability in children with ADHD. Child Psychol Psychiatry 53(11): 1139-1148.
- Baron R, Maier C, Attal N, Binder A, Bouhassira D, et al. (2017) Peripheral neuropathic pain: A mechanism-related organizing principle based on sensory profiles. Pain 158(2): 261‐272.
- Behdad S, Behdad S, Mortazavizadeh A, Ayatollahi V, Saidhossein K (2014) The effects of propofol and isoflurane on blood glucose during abdominal hysterectomy in diabetic patients. Diabetes Metab J 38(4): 311-316.
- Bergmans E, Jacobs A, Desai R, Masters OW, Thies KC (2015) Pain relief after transversus abdominis plane block for abdominal surgery in children: A service evaluation. Local Reg Anesth 8: 1-6.
- Bilimoria KY, Yaoming L, Jennifer LP, Lynn Z, Thomas EK, et al. (2013) Development and evaluation of the universal ACS NSQIP surgical risk calculator: A decision aid and informed consent tool for patients and surgeons. J Am Coll Surg 217(5): 833-842.e1-3.
- Bjorgaas HM, Elgen I, Boe T, Hysing M (2013) Mental health in children with cerebral palsy: Does screening capture the complexity? Scientific World Journal 2013: 468402.
- Boavista BHL, Leme SP, Ferreira CF, Pelosi P, Rieken MRP (2020) Immunomodulatory effects of anesthetic agents in perioperative medicine. Minerva Anestesiologica 86(2): 181-195.
- Öksüz G, Bilal B, Gürkan Y, Urfalioğlu A, Arslan M, et al. (2017) Quadratus lumborum block versus transversus abdominis plane block in children undergoing low abdominal surgery: A randomized controlled trial. Reg Anesth Pain Med 42(5): 674-679.
- Raja SN, Carr DB, Cohen M, Finnerup NB, Flor H, et al. (2020) The revised international association for the study of pain definition of pain: Concepts, challenges and compromises. Pain 161(9): 1976-1982.
- Rawal N (2012) Epidural technique for postoperative pain: Gold standard no more? Reg Anesth Pain Med 37(3): 310-317.
- Reynolds RA, Legakis JE, Tweedie J, Chung Y, Ren EJ, et al. (2013) Postoperative pain management after spinal fusion surgery: An analysis of the efficacy of continuous infusion of local anesthetics. Global Spine J 3(1): 7-14.
- Rove KO, Brockel MA, Saltzman AF, Dönmez MI, Brodie KE, et al. (2018) Prospective study of enhanced recovery after surgery protocol in children undergoing reconstructive operations. J Pediatr Urol 14(3): 252.e1-252.e9.
- Russell P, Ungern VSBS, Schug SA (2013) Perioperative analgesia in pediatric surgery. Curr Opin Anaesthesiol 26(4): 420-427.
- Sama HD, Bang'na MAF, Djibril M, Assenouwe M, Belo M, et al. (2014) Post-operative pain management in paediatric surgery at Sylvanus Olympio University Teaching Hospital, Togo. Afr J Paediatr Surg 11(2): 162-165.
- Schnabel A, Reichl SU, Meyer Frießem C, Zahn PK, Pogatzki ZE (2015) Tramadol for postoperative pain treatment in children. Cochrane Database Syst Rev 2015(3): CD009574.
- Sebe A, Hayri LY, Zikret K, Mehmet OA, Muge G (2014) Comparison of midazolam and propofol for sedation in pediatric diagnostic imaging studies. Postgrad Med 126(3): 225-230.
© 2024 Fayziev OY. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






