- Submissions

Full Text
Research in Pediatrics & Neonatology
Quantifying the Reduction Soccer Eye Protection has on Pediatric Retinal Trauma
Andrew Suh1, Matthew Lam2, Yasin Shokrollahi3, Pengfei Dong3, Linxia Gu3 and Donny Suh4*
1Tulane University School of Medicine, New Orleans, USA
2Creighton University School of Medicine, Omaha, USA
3Florida Institute of Technology, Department of Biomedical and Mechanical Engineering, Melbourne, USA
4Gavin Herbert Eye Institute, University of California Irvine, Department of Ophthalmology and Visual Sciences, Irvine, USA
*Corresponding author: Donny Suh, Gavin Herbert Eye Institute, University of California Irvine, Department of Ophthalmology and Visual Sciences, Irvine, USA
Submission: August 01, 2023; Published: August 15, 2023

ISSN: 2577-9200 Volume7 Issue5
Opinion
Sports-related ocular injury is most common in the pediatric population, with over half of all cases being reported in patients ≤18 years of age [1]. Soccer, the most popular sport in the world, causes a disproportionate number of eye injuries in individuals <25 years of age [2] and is the second most common cause of sports-related eye injuries after baseball [3]. Despite the risk of potentially vision-threatening injury such as retinal detachment or macular hole, players rarely use protective eyewear. Prior research studying soccer ball trauma has suggested the need for protective eyewear because of the irreversible effects it can have on the eyes but has rarely quantified the degree of ocular protection such eyewear would provide [4]. This investigation provides insight into the mechanisms and efficacy of protective eyewear in reducing retinal damage resulting from collision of a soccer ball by quantifying retinal stress with a Finite Element (FE) computer simulation.
An FE computer simulation allows for the manipulation and measurement of stress, strain, energy, pressure and other biomechanical endpoints during a given clinical scenario with exquisite resolution. In this simulation, an eye model was developed by reviewing medical and mechanical literature of previous eye models used to study eye injuries and eye protection [5]. The model consisted of the sclera, vitreous, retina, retinal vessels and vitreoretinal attachments along the retinal vessels, which are the main components of the eye that are involved during impact trauma. All components were based on the size of an average pediatric eye [6,7]. Additionally, the structure of an average pediatric skull was obtained from the GrabCAD.com website, and the eye model was positioned in the orbit. Finally, two different protective eyewear models were simulated, with characteristics of polycarbonate and acrylic, to evaluate which popular material provided better protection.
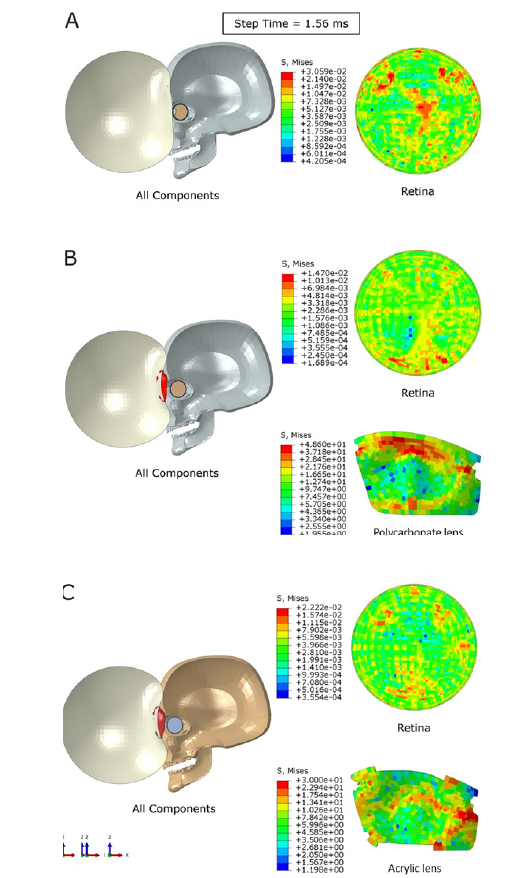
Three scenarios were simulated: Soccer ball impact to the eye without eye protection, with polycarbonate eyewear, and with acrylic eyewear. In each trial, a typical 22.4m/s kick of a regulation-sized soccer ball collided with the eye model from directly straight ahead [8]. Stress and strain energy that the retina experienced were measured in kilopascals (kPa) and millijoules(mJ), respectively. Both types of protective eyewear were found to be effective in lowering ocular stress and strain energy by both absorbing energy in the form of deforming and/or cracking and redirecting energy from the ball to the bony orbit instead of the globe (Figure 1). Compared with the unprotected eye model, polycarbonate eyewear reduced the average stress the retina experienced by 61%, whereas the acrylic model reduced the average stress by 40% (9.7kPa to 3.8kPa and 5.8kPa, respectively), signifying that polycarbonate is the superior material. The polycarbonate and acrylic eyewear also reduced the maximum strain energy experienced by the retina by 69% and 47%, respectively (4.45mJ to 1.39mJ and 2.34mJ, respectively), reducing the severity of deformations of the eye upon impact.
Figure 1:Stress distribution in the posterior retina and eyewear lens at the same timepoint of 1.56ms. A: Unprotected eye model; B: Polycarbonate lens model (no cracks present); C: Acrylic lens model (some cracks and shatters present around the glasses).
These findings suggested that wearing protective eyewear is an effective means of reducing retinal stress during traumatic eye injury. The use of eye protection should thus be strongly considered for pediatric patients participating in soccer. Furthermore, some athletes are at a particularly higher risk for ocular injury and should thus be more strongly advised to wear protective eyewear. For instance, patients with one eye are at greater risk for injury due to obscured depth perception impairing their ability to quickly judge the position of an oncoming ball [8]. Additionally, patients who have a personal or family history of eye illnesses should be strongly recommended to wear protective eyewear. For example, patients who suffer from myopia tend to have thinner retinas and have an increased risk of retinal tears, retinal detachments, and other serious pathology that may be accelerated by trauma [9]. Patients with Marfan syndrome should also strongly consider protective eyewear, as weakened connective tissues in the eye make them more prone to retinal detachments and retinal hemorrhages [10]. In this investigation, we found that polycarbonate decreased retinal stress more effectively than acrylic. Polycarbonate is also a low-cost thermoplastic with high transparency and good toughness and rigidity, even at relatively high temperatures [4]. Another point to consider is that acrylic breaks more easily than polycarbonate, which could be dangerous in our scenario if broken lens fragments are pushed into the globe by the force of the soccer ball impact. However, there are other aspects to these materials to consider beyond the results of the simulations. Although polycarbonate is not easily broken, the material scratches easily and becomes difficult to see through; acrylic is clearer and does not scratch as easily.
Furthermore, acrylic is less expensive than polycarbonate, which may increase accessibility. Finally, recent research has suggested that excess exposure to polycarbonate plastics can lead to various tissue and organ disorders, especially neurological illnesses [11]. Therefore, it would be best to continue exploring different material options for protective eyewear. The primary limitation of this study is that although FE simulations can suggest that protective eyewear effectively prevents or limits ocular injury, they do not provide direct evidence. Future work to build on the findings of this study should address this limitation by including real-world validation that these findings correlate to reductions in quantity and severity of injury. In vitro studies on sheep and/or monkey eyes and retrospective comparison of outcomes of ocular trauma in soccer players who were and were not wearing protective eyewear at the time of injury would provide relevant clinical correlates.
Another limitation of this study is that the FE eye model focused primarily on the retina. Additional factors, such as agerelated liquefaction of the vitreous or presence of the physiologic lens of the eye, may influence the propagation of translational forces. Future studies will consider various vitreous viscosities and include additional ocular structures, including the physiologic lens.
References
- Haring RS, Sheffield ID, Canner JK, Schneider EB (2016) Epidemiology of sports-related eye injuries in the United States. JAMA Ophthalmol 134(12): 1382-1390.
- Capao Filipe JA, Fernandes VL, Barros H, Falcao RF, Castro CJ (2003) Soccer-related ocular injuries. Arch Ophthalmol 121(5): 687-694.
- Moon S, Ryoo HW, Ahn JY, Jung BP, Kang SS, et al. (2016) Analysis on sports and recreation activity-related eye injuries presenting to the emergency department. Int J Ophthalmol 9(10): 1499-1505.
- Gledhill A, Forsdyke D (2018) An ounce of prevention is better than a pound of cure: Shouldn’t we be doing EVERYTHING to reduce sports injury incidence and burden? Br J Sports Med 52(20): 1292-1293.
- Suh DW, Song HH, Mozafari H, Thoreson WB (2021) Determining the tractional forces on vitreoretinal interface using a computer simulation model in abusive head trauma. Am J Ophthalmol 223: 396-404.
- Saffioti JM (2014) Characterization of pediatric ocular material properties for implementation in finite element modeling.
- Yamazaki J, Yoshida M, Mizunuma H (2014) Experimental analyses of the retinal and subretinal haemorrhages accompanied by shaken baby syndrome/abusive head trauma using a dummy doll. Injury 45(8): 1196-1206.
- Vinger PF, Capão FJA (2004) The mechanism and prevention of soccer eye injuries. Br J Ophthalmol 88(2): 167-168.
- Zhang H, Jiang X (2020) The application of protective devices in sports-related eye injuries. In: Yan H (Ed.), Sports-Related Eye Injuries. Ocular Trauma. Springer, pp. 107-119.
- Razaghi R, Biglari H, Karimi A (2020) Finite element modeling of the eyeglass-related traumatic ocular injuries due to high explosive detonation. Eng Fail Anal 117: 104835.
- Seldén R (1987) Fracture energy measurements in polycarbonate and PMMA. Polymer Test 7(3): 209-222.
© 2023 Donny Suh. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






