- Submissions

Full Text
Research in Pediatrics & Neonatology
PANDAS-Syndrome Based on the Unique Immunological Pathomechanism
Anna Pituch Noworolska*
Immunology Unit, University Children’s Hospital in Kraków, Poland
*Corresponding author: Anna Pituch Noworolska, Immunology Unit, University Children’s Hospital in Kraków, Wielicka 265, 30-665 Kraków, Poland
Submission: July 10, 2023; Published: July 17, 2023

ISSN: 2577-9200 Volume7 Issue5
Opinion
PANDAS-(Pediatric Acute Neuro-Psychiatric Disorders after Streptococci) develops in association with streptococcal infection. In early description of this clinical syndrome it was believed to occur only after α-hemolyticus type of streptococci. Now, we know that all types of streptococci even, without clinical symptoms of infection are possible inductive pathogens for these symptoms. The criteria are precise enough to differentiate between PANDAS, PANS, Tourette tics disease or OCD as psychiatric disease. The onset of symptoms (tics, emotional lability, aggression, OCD, sleep disturbances (insomnia), anxiety especially of separation, new people and new surroundings, serious changes in behaviour) is sudden, with exacerbations after infections and spontaneous resolving in time without infections [1]. This remitting type of course of symptoms is very often the reason for denying this disease, treating as myth’ or just ‘bad behaviour” of child [2].
Watching child symptoms and story of infections we are facing following questions:
a) why only streptococci from all strains of patogenic bacterias are inducing these
symptoms
b) why the course is episodic (relapsing-remitting)
c) is the antibody-mediated autoimmune mechanism only one responsible for
syndrome
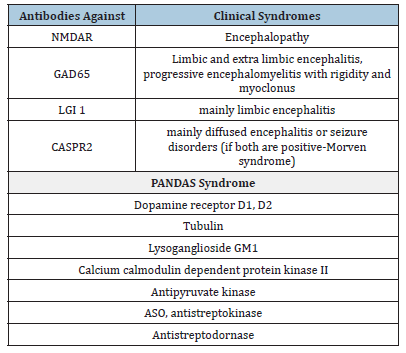
The basic mechanisms postulated from time study of sequele after Streptococci infection in heart disease, joint inflammation and kidney chronic glomerulonephritis are based on antigenic mimicry [1,3-5]. The neurologic complication after Streptococci infection was diagnosed as Sydenham chorea, however, usually it was one episode resolving with antibiotic therapy [1,3,6]. The mimicry was between group A Streptococcal carbohydrate epotipe N-acetyl-beta-D-glucosamine and brain lysoganglioside and tubulin. Antibodies in central nervous system are activating calcium calmodulin dependent protein kinase II (CaMKII). The antibodies isolated from PANDAS patients sera are reacting with dopamine receptors [1-5,7] leading to clinical symptoms. The whole reaction is localised in basal ganglia resulting in their enlargment [1,2,5,6]. In central nervous system morphological indicators for these process are-enlarged striatum caudatum, basal ganglia, globus pallidus, overactivation of microglia and dysregulation within striatal interneurons [1,5,6]. The study of serum and cerebrospinal fluid from patient with symptoms of PANDAS showed the long list of antibodies to neuronal antigens related to the autoimmune process as basic mechanism responsible for clinical symptoms and leading to autoimmune encephalitis [1,6]. The list of antibodies [1] is shown in Table 1. The diagnosis of PANDAS syndrom is based mainly on fulfilling the clinical criteria [1-4,7], as there are no definitive diagnostic laboratory tests for PANDAS [2]. Intermitting course of PANDAS symptoms are typical for systemic autoimmune diseases. Therapy usually started from antibiotics (penicilline, azitromycine usually), antiinflammatory therapy (streoids, NSAID) and antipsychoactive drugs depending on clinical symptoms. In severe course or clinical overt symptoms of autoimmune encephalitis the apheresis, immunoglobulins in high dose and immunosuppression are used. Patients with PANDAS symptoms very often are showing remissions and good response to supporting psycho and behavioral therapy. The majority of children are fully recover during puberty what arise the question about role of hormones, neuronal maturation and final development of immune system in PANDAS syndrome.
Table 1: Antibodies in PANDAS and encephalic syndromes in children and adolescents [1,7].
References
- Baj J, Sitarz E, Forma A, Wróblewska K, Karakuła JH (2020) Alterations in the nervous system and gut microbiota after β-hemolytic Streptococcus group A infection-characteristics and diagnostic criteria of PANDAS recognition. Int J Mol Scie 21: 1476-1500.
- Hutanu A, Reddy LN, Mathew J, Avanthika CH, Jhaveri SH (2022) Pediatric autoimmune neuropsychiatric disorders associated with group A Streptococci: Etiopathology and diagnostic challenges. Cureus 14(8): e27729.
- Cunnigham MW (2019) Molecular mimicry, autoimmunity and infection: The cross-reactive antigens of group A streptococci and their sequelae. Microbiol Spectr 7(4).
- Dop D, Marcu JR, Padureanu R, Niculescu CE, Padureanu V (2021) Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (review). Experim Therap Medicine 21(1): 94.
- Gagliano A, Carta A, Tanca MG, Sotgiu S (2023) Pediatric acute-onset neuropsychiatric syndrome: Current perspectives. Neuropsychiatric Dis Treatment 19: 1221-1250.
- Chain JL, Alvarez K, Macaro BA, Reim S, Bentley R, et al. (2020) Autoantibodies biomarkers for basal ganglia encephalitis in sydenham chorea and pediatric autoimmune neuropsychiatric disorder associated with streptococcal infections. Frontiers in Psychiatry 11: 564.
- Bien CG, Bien CI (2020) Autoimmune encephalitis in children and adolescents. Neurological Res Practice 2(4).
© 2023 Anna Pituch Noworolska. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






