- Submissions

Full Text
Research in Pediatrics & Neonatology
Subcutaneous Bronchogenic Cyst a Rare Entity
Heera Tharanendran1*, Balagopal Subramanian1 and Seyed Rabia2
1Department of Pediatric Surgery, Kanchi Kamakoti CHILDS Trust Hospital, India
2Department of Pathology, Kanchi Kamakoti CHILDS Trust Hospital, India
*Corresponding author: Heera Tharanendran, Department of Pediatric Surgery, Kanchi Kamakoti Child’s trust hospital, No: 12 A Nageswara road, Tirumurthy nagar, Chennai, India
Submission: May 21, 2023; Published: July 06, 2023

ISSN: 2577-9200 Volume7 Issue5
Abstract
Sub-Cutaneous Bronchogenic Cyst(SBC) is a rare entity and most likely represents ectopic or displaced mesenchyme during early development. We are reporting a 2-year-old girl with swelling over the sternum since birth and a discharging sinus. On evaluation, imaging revealed a well-defined cystic lesion in the pre-sternal deep subcutaneous region without intrathoracic extension. A complete excision was performed, and histopathological examination was suggestive of a bronchogenic cyst. The presentation of a subcutaneous bronchogenic cyst, a relatively rare entity, and its outcome, which was successfully treated with simple excision, are highlighted. This case is presented for its rarity and to create awareness about the entity.
Keywords:Bronchogenic cyst; Cutaneous; Pre-sternum
Case Report
The patient is a 2-year-old female child who presented to us with a swelling over the pre-sternal region since birth. The mother reported intermittent discharge of whitish fluid through a small opening over the swelling, starting around 3 months of age. Antenatal history was uneventful. There was no other relevant medical or surgical history. Physical examination revealed a 15mm *15mm swelling over the pre-sternum in the midline with a small punctum over the summit. The swelling was cystic in consistency; it was partially fluctuant and mobile and there was no active discharge from the punctum on examination. There were no signs of inflammation. Ultrasound examination revealed a well-defined cystic lesion with peripheral thick capsulation and linear vascularity noted in the pre-sternal deep subcutaneous region. The cyst appeared to be communicating with the skin opening. No evidence of intrathoracic or bone extension was identified. The cyst was excised under general anesthesia. Intraoperatively, the cyst was found to be superficial to the sternal periosteum. The cyst was excised in toto with the punctum the contents were mucoid.
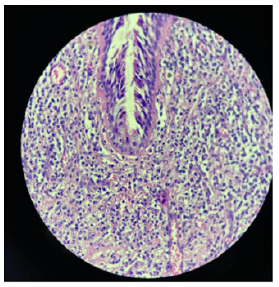
She had no postoperative complications. Histopathological examination demonstrated a cyst lined with pseudostratified ciliated columnar epithelium (respiratory epithelium) with interspersed goblet cells. The wall showed smooth muscle bundles and seromucous glands. Cartilaginous and lymphoid elements were absent, which was suggestive of a bronchogenic cyst. The child is doing well on follow up.
Discussion
Bronchogenic cysts are rare congenital anomalies that are usually located in the mediastinum or lung parenchyma. Bronchogenic cysts in the subcutaneous region are very rare and thought to result from abnormal development of the tracheobronchial system [1]. In 1945, Seybold and Clagett first described a case of SBC [2]. Approximately 50% are present at birth. Most are diagnosed in early childhood. However, few cases have been reported in adulthood. The most common symptoms are swelling with or without draining sinuses, signs of inflammation seen when infected. In the literature so far, approximately 160 cases have been described. There are two theories of origin [3,4]. The first is that the cyst loses connection with the parent bronchus and is left out of the thorax after sternal closure at 9 weeks’ gestation. It then migrates to a cutaneous region. The second theory is that the cyst separates from the developing tracheal bud during sternal closure.
Bronchogenic cysts are classified by Maier according to their site of origin into paratracheal, carinal, hilar, paraoesophageal and atypical, such as diaphragmatic, abdominal, intracutaneous, subcutaneous, or subscapular [5]. The most common location of SBC is the neck (46%), followed by the suprasternal notch (24%), pre-sternal (11%), and scapular regions (11%) [6]. Intradural Extramedullary bronchogenic cysts in the high and mid cervical regions were also reported. In our case, it was located on the manubrium stern in the midline (Figure 1). The diagnosis of bronchogenic cysts is confirmed by histopathological examination. Histologically, the cyst is lined by ciliated and mucin-producing pseudostratified columnar epithelium of respiratory type, although stratified squamous epithelium may be present in the outer part of the cyst or as a sinus on the surface [7]. There may also be smooth muscle fibers, cartilage, or mucous glands in the wall of the cyst. Sakaguchi et al. [8] found in their study of 5 cases of subcutaneous bronchogenic cysts that all cases had respiratory epithelium, mucinous glands in 4 cases, and smooth muscle bundles in 2 cases. Cartilage was not seen. In our case, respiratory epithelium, mucinous glands, and smooth muscle bundles were seen without cartilaginous tissue (Figure 2 & 3).
Figure 1:Clinical photograph of the child showing swelling over the pre-sternum with a punctum at the summit..

Figure 2:HPE-Low power view of cyst wall a) Respiratory epithelium; b) Smooth muscle cells; c) Seromucous glands
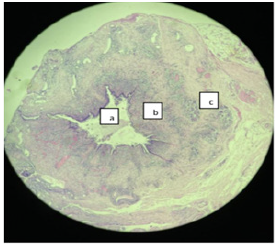
Figure 3:High power view of pseudostratified ciliated epithelium.
The differential diagnosis includes branchial cleft cysts, epidermal inclusion cysts, thymic cysts, cystic teratomas, and thyroglossal duct cysts [9]. The thymic cyst contains distinct epithelial constituents, Hassall’s corpuscles, whereas thyroglossal duct cysts uniquely possess thyroid follicles. Distinguishing branchial from bronchogenic cysts is difficult. Although bronchogenic cysts are more likely to contain only pseudostratified ciliated epithelium without lymphoid tissues, branchial cleft cysts with similar characteristics have been reported. The midline location and histologic appearance of this patient’s cyst support the diagnosis of a subcutaneous bronchogenic cyst [10]. However, in our case, the diagnosis was only made postoperatively with the histology report. Imaging helps to delineate the plane of the swelling. In our case, an ultrasonogram of the swelling revealed that the lesion was in the deep subcutaneous plane without intrathoracic extension. Surgical excision of the entire cyst is recommended. Complications like recurrence after incomplete excision and malignancy arising from SBC were reported in the literature [11]. Malignant transformation of the cyst, including the development of melanoma [12] and adenocarcinoma arising from subcutaneous bronchogenic cyst were reported [10] further supporting the decision for early excision. The recommended approach is an elliptical incision over the lesion to completely excise an intact cyst and exclude intrathoracic extension [11].
Conclusion
Subcutaneous Bronchogenic cysts are a rare entity. It needs complete excision to prevent recurrence and malignant changes. Histopathology is a main cornerstone in the diagnosis of these lesions. This case is presented for its rarity and to create awareness about the entity.
References
- Takako N, Misato K, Hiromi K, Nobuharu H, Koichi U (2020) A case of giant subcutaneous bronchogenic cyst. Arch Clin Med Case Rep 4(4): 590-595.
- Seybold WD, Clagett OT (1945) Presternal cyst. J Thorac Surg 14(3): 217-220.
- Kim NR, Kim HH, Suh YL (2001) Cutaneous bronchogenic cyst of the abdominal wall. Pathol Int 51(12): 970-973.
- Zvulunov A, Amichai B, Grunwald MH, Avinoach I, Halevy S (1998) Cutaneous bronchogenic cyst: Delineation of a poorly recognised lesion. Pediatr Dermatol 15(4): 277-281.
- Maier HC (1948) Bronchiogenic cysts of the mediastinum. Ann Surg 127(3): 476-502.
- Mohammed F, Philip M (2017) Bronchogenic cyst-a rare case mimicking a laryngocoele. Journal of Surgical Case Reports 17(3): 55.
- Carden C, Dykes E, Pollock AM (2008) An unusual midline swelling: Case report of cutaneous bronchogenic cyst. Eur J Pediatr Surg 18(5): 345-346.
- Sakaguchi T, Hamada Y, Nakamura Y, Takeshi S, Hiroshi H, et al. (2017) Subcutaneous bronchogenic cyst: Report of five cases and review of the literature. Journal of Pediatric Surgery Case Reports 19: 9-15.
- Shah SK, Stayer SE, Hicks MJ, Mary LB (2008) Suprasternal bronchogenic cyst. J Pediatr Surg 43(11): 2115-2117.
- Yu HJ, Kwon HM, Park JW, Hwang DK, Ahn DK, et al. (2001) A case of cutaneous bronchogenic cyst over the left scapula. J Dermatol 28(10): 572-575.
- Kim PS, Mary C, Daniel JG, Vlada A, Elena S, et al. (2012) Unusual presentation of a cutaneous bronchogenic cyst in an asymptomatic neonate. J Pediatr Surg 47(7): E9-E12.
- Tanita M, Kikuchia NK, Ogoshi K, Toshiaki S, Nobuko T, et al. (2002) Malignant melanoma arising from cutaneous bronchogenic cyst of the scapular area. J Am Acad Dermatol 46(2 Suppl): S19-21.
© 2023 Heera Tharanendran. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






