- Submissions

Full Text
Research in Pediatrics & Neonatology
Enthusiastic Women Community Health Workers Will Act as an “Influencers” to Promote Health Care Services and Reduce Maternal and Perinatal Mortality Rates in Rural Ethiopia
Iñaki Alegria*
Pediatrician, Gambo General Hospital, Maternal and Child Health Program director, Oromiya, Ethiopia
*Corresponding author: Iñaki Alegria, Pediatrician, Gambo General Hospital, Maternal and Child Health Program director, Oromiya, Ethiopia
Submission: March 06, 2023; Published: March 24, 2023

ISSN: 2577-9200 Volume7 Issue3
Introduction
First second, minute, hour, day, week, month; each step is a full fight against death in rural southern Ethiopia. Since the first second of life new-born are breathing against death for survive. One million new-born just die after the first seconds of live [1]. Worldwide, 2.6 million new-born die before born, just during labour and delivery. Every year 2.5 million of babies die before celebrating the first month of live, it means around 7000 every day, most of them just the first week of life and 36% of them the first day of life, ¾ the first week [2]. Despite of all, the most dramatical situation is that each death is preventable and a social injustice [3]. More than 80 per cent of new-born deaths are due to of premature birth, complications during labour and delivery and infections such as sepsis, meningitis and pneumonia. More than 99% of these deaths we can avoid having access to affordable and quality health care [4,5].
During last decades under five mortalities has decreased, but the main challenge at this time is decrease neonatal mortality that continues dramatically high in Ethiopia and other low-income countries [6,7]. This is partly because new-born deaths are difficult to address with a single drug or intervention, they require a wide approach. It is also due to a lack of global commitment to new-born survival. The risk of dying as a new-born varies enormously depending on where a baby is born [8,9]. Under 5 mortality declined in Sub-Saharan Africa from 3782 thousand in 1990 to 2715 thousands, but in 2017 sub-Saharan deaths represents 50.1% of all world under 5 deaths whereas in 1990 only 30.1% [10]. In 2017, Ethiopia Under 5 mortality 41/1000 live birth (133000 deaths). New-born 29/1000 (95000 deaths) [10]. But the run for live is not just starting on birth, also not nine months before, is starting when the future mother is a girl, because also depends on her live, studies, nutrition, age. The maternal (620/100,000 live births), perinatal (100/1,000), and infant (80/1,000) mortality rates in Africa are the highest in the world. In sub-Saharan Africa the rates are even higher. The maternal, perinatal, and infant mortality rates are (1,000/100,000 live births), (160/1,000), and (120/1,000), respectively. It is estimated that about half of the world’s maternal and infant mortality cases are in sub-Saharan Africa [11].
New-born Health is an increasingly important issue in the SDG period. Sustainable Development Goal framework and the Global Strategy for Women’s, Children’s, Adolescents Health (2015-2030) [12]. To achieve the SDG, we cannot focus only on new-born. Every Woman Every Child partnership (EWEC) [13] puts the Global Strategy into action: Ending preventable new-born deaths by 2030, the target of 12 or less new-born deaths per 1,000 live births and continue to reduce death and disability, ensuring that no new-born is left behind; ending preventable stillbirths the target of 12 or less stillbirths per 1,000 total births and to continue to close equity gaps [14]. Regarding maternal mortality, is one of the best criteria for assessing the relative performance of health systems. The model was described as three delay system, goes beyond emergency obstetric care [15,16]. The WHO health system building blocks offer a starting point for classifying health system determinants and include the following [17]. In Africa, every year 300,000 women die during the pre-natal, delivery, or post-natal stages of pregnancy, as well as a total of 8,000,000 children under the five years old. The majority are a result of causes that are entirely avoidable given an adequate level of primary care.
Ethiopia, the oldest independent and second most populous country in Africa with a population of over 96 million , a unique cultural heritage with a diverse population mix of ethnicity and religion, who served as a symbol of African independence throughout the colonial period, and a founding member of the United Nations and the African base for many international organizations; a country of nearly 85.9 million where the great majority of people 84% live in rural areas, maternal and new-born mortality remains a serious problem. In 2011, the maternal mortality ratio was estimated at 676 deaths per 100,000 live births; neonatal mortality was estimated at 37 deaths per 1000 live births. Child mortality is still high and neonatal mortality contributes about 40% of all deaths [17]. Highest perinatal mortality with a rate of 130 per 1000 live births. The Ethiopian Demographic and Health Survey (EDHS 2016) reported the national perinatal mortality rate as 46 per 1000 pregnancies, showed a higher rate among women living in rural areas. The same study indicated a regional prevalence of 45 per 1000 pregnancies in the Oromia Region [18]. The perinatal mortality rate of 85 per 1000 total deliveries Obstructed labour, mal presentation, preterm birth, antepartum hemorrhage and hypertensive disorders of pregnancy were independent predictors for perinatal deaths [17]. In Ethiopia specifically, there were 412 maternal death per 100,000 live births, in Oromo region there were 20% of births were assisted by a skilled provider and there were 37 neonatal and 79 under-five deaths per 1,000 live births according to the 2016 Demographic and Health Survey. 80% of Ethiopia’s population lives in rural communities that lack adequate health care, yet the government allocates only 20% of its heath care budget to these same communities. As such, according to ‘The Sub-Saharan African Medical Study’ (2011), less than 20% of licensed health professionals work in rural areas. The lack of educated personnel and the lack of other resources required of a functioning health center, such as electricity, along with poor accessibility and certain anthropological factors contribute to these high mortality rates. These issues are severely acute for Gambo Hospital’s catchment population which gives reasons to expect that the mortality rates are even higher here.
In Oromia region there were 20% of births were assisted by a skilled provider and there were 37 neonatal and 79 under-five deaths per 1,000 live births according to the 2016 Demographic and Health Survey. In rural communities of Ethiopia, women often give birth in unsanitary conditions, without running water, and assisted by family members or traditional midwives. The perinatal and infant mortality rate reaches 180 deaths per 1000 cases. Ethiopia regarding Human Development Index (HDI) is at position 173 out of 189 countries inside the category of low human development countries. Ethiopia is also below the average for the countries in the low human development group and below the average of countries in sub-Saharan area. Despite global improvement, the inequalities and differences between urban and rural, richest and poorest and increased. Inequality and access to care remain a problem. The 214 World Health Report identified one of the main problems is the lack of registrations and audits. To improve this the Ethiopian Federal Ministry of Health, develop de Maternal and Perinatal Death Surveillance Response (MPDSR) adding the neonatal registration.
Objectives
In Ethiopia, Primary health care (PHC) is delivered through health centers and at community-level through health posts staffed with health extension workers (HEWs). The HEWs, on average two per health post, divide their time between health post and community outreach activities. Nurses from the health center supervise HEWs. We are following Strategic objectives for Every New-born and Ending Preventable Maternal Mortality [14] and implementing the Global Strategy for Health Workforce. Our main strategic objectives: Improving quality and experience of care, while ensuring full integration of services for mothers and babies across the continuum of care; Strengthen health systems to optimize the organization and delivery of care through the workforce, and primary health care; Reach every woman and newborn by minimizing inequities in access to and coverage of care; Empowering parents, families and communities, and engage with society. The program is in 40 kebeles, 40 health post, 10 health centers belonging to three woredas of West Arsi Zone in Oromia region in the southeast of Ethiopia. Distributed on the next way: Arsi Negele woreda: Basako, Gambelto and Kelo Duro health centers; Qore woreda: Beta Wontesha, Qore, Gobe, Shiree and Lencha Ansha health centers; Heban Arsi worede: Goljota and Meti health centers. The health system in Ethiopia there is a decentralization from the reginal to the woreda (district). Woredas are the basic decentralized administrative unit. It is called three-tier health service system and it is structured on the next way. The primary care level is compounded by health post, health center and primary hospital. The Ethiopian Federal Ministry of Health launched the Health Extension Program HEP with the main goal of improving the health care in rural area. HEP is based on Alma-Ata Declaration* of 1978, that focus on Primary Health Care as the starting point to achieve the main objective of “Health for all”. Although the program was implemented in all the country, not all the regions achieved a properly outcome as we will analyze. According the Ethiopian Health Extension Program, the Ethiopia’s health service delivery is structured into a three-tier system: primary, secondary and tertiary levels of care. The HEP is positioned, implemented and managed under the umbrella of the primary health care unit (PHCU) Two HEWs are assigned to one health post to serve a population ranging from 3000 to 5000 in a village (kebele). Five health posts and a health center work in collaboration and form the PHCU that serves 25,000 people. The health center serves as a referral center. The health post is under the supervision of the district health office and the kebele administration and receives technical support from the nearby health center.
Volunteer CHWs (including traditional birth attendants, health promoters, and reproductive health agents) help HEWs in mobilizing the community. A Health post has one of two health extension workers and a catchment population of 3000 to 5000 people. Is a place where is provided only community health education and preventive services: Immunization, deworming, vitamin A distribution, MUAC nutritional screening. A health center has a 60000 to 100000 catchment population. In this place is provided preventive and curative services and is a training center for HEW. A primary hospital provides in-patient and out-patient services, caesarean section, emergency surgery, blood transfusion. Is a training center for nurses, health officers, general practitioners, IESO, midwives? A Health Extension Worker is a woman with residence in the village, knowledge of the local language, graduation at least 10th grade, with the willingness to remain in the village and serve the community. Representatives from the woreda and the community are the persons who will select the HEW in each health post. A HEW works in contact with voluntary community health workers. Each HP has 2 HEW with one-year training. HEWs are often younger women who may not be trusted by the community to assist during delivery. A recent analysis of strengths, weaknesses, opportunities, and threats identified numerous weaknesses in the HEP, including low health service utilization; weak referral systems; low service quality; shortage of drugs, medical supplies, and equipment; and lack of a career trajectory for HEWs. The analysis also raised a concern that the increasing number of tasks allocated to HEWs and their growing workload will compromise their ability to complete their tasks. Finally, additional challenges for the HEP include high levels of staff turnover and lack of integration of services.
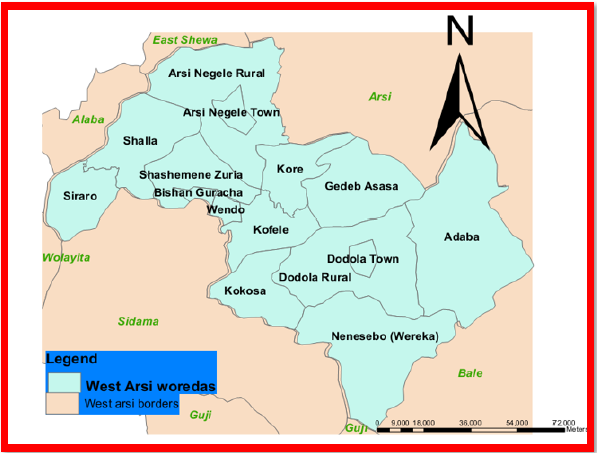
A model family is a family that is acting as a role model in the community supporting health messages and leading desired practices and behaviors. Model families are trained in maternal health, able to influence their relatives and neighbors to adopt the same practices, leader experience-sharing initiatives, work as a part of the health army to engage communities for health improvement. Health Development Army is an organized movement of communities through participatory learning and action meetings. They identify bottlenecks at local level, develop feasible strategies, is a platform to discuss and prioritize bottlenecks and strategies and to share best practices experiences. Women’s Development Army, Community-Based Data for Decision-Making (CBDDM) and a Participatory Community Quality Improvement strategy. HEW act at different level: Household level community level, schools and youth centers level, health post level. Roles and responsibilities of the health system are stablished by Ethiopian Federal Ministry of Health, Oromia Regional Health Office, West Arsi Zone Health Department, 3 woredas Health Offices (Arsi Negele, Kore and Heban Arsi woredas Health Office) (Figure 1,2).
Figure 1: Oromia Region, Ethiopia.

Figure 2: West Arsi Zone Woreda.
The Ethiopia’s health system if full of challenges. To overcome them, first is necessary a deep analyze and understand the reason behind each gap, as we are going to analyze during this article. Despite these successes, the HEP had also challenges since the launch of the program. There were resource gaps, including medical equipment and drugs; limited supportive supervision; absence of a well-established referral system; high turnover of HEWs; absence of clear career structure for HEWs; unattractive salary scale; and, inadequate delivery and curative services in 2008. Most of the health posts, specially in rural Oromia areas, did not have basic infrastructures like water supply, electricity, and waiting rooms for women in labour [12]. Living and working conditions of HEWs were not conducive during the early phase of the implementation of the HEP, according to a study published in 2007. HEWs were deployed in remote areas where housing was very important in motivating and retaining them in the communities. The relationships between HEWs and other CHWs was not clearly established by 2008. A recent study, published in 2017, on job-related wellbeing indicated that stress and burnout were recognized among healthcare workers. Notwithstanding these, there were an unmet need for interventions to manage burnout or emotional difficulties. In a study published in 2018, it was identified that the majority (88%) of HEWs had poor knowledge on danger symptoms and signs, and complications in pregnancy. Moreover, most HEWs did not feel confident enough to undertake delivery independently because of limited practice during the training. Even later, in a study published in 2013, it was found that the skill and competency of HEWs to handle maternal health services was less trusted. In another paper in 2015, only 50.5% of study participants perceived that HEWs were competent to deliver curative and delivery services. A recent study identified that pre-service education did not prepare HEWs for all the tasks that comprise their scope of practice. The studies also showed that the HEP did not have a statistically significant effect on delivery and postnatal care services in 2009 [13]. Utilization of clean and safe delivery was very low (19%) with only 1% of study participants giving birth at health posts in 2012 and 2013 [16]. HEP was not associated with skilled deliveries, nor with some new-born health care indicators in 2012 [17]. Health facility delivery was not significantly associated with visit by HEWs during pregnancy [OR = 0.87 (95% CI 0.25, 2.96)] in 2013 [17].
Gambo Rural General Hospital is the unique provider of affordable and accessible health care to a rural population dispersed in large distances isolated by poor pathways, economic difficulty, and familiar and occupational responsibilities, among other obstacles. Its catchment population suffers elevated mortality rates for women in pre-natal, delivery, and post-natal stages of pregnancy as well as widespread malnutrition. A network of primary care among the local villages of the catchment population is a legitimate solution to the prevalence of the simple but detrimental problems affecting maternal and pediatric health. This network requires the education and management of rural health workers for the enhancement and maximization of care provided by local health posts. The main goal is to improve the maternal and pediatric health of the catchment population through the empowerment and education of rural women health workers thereby providing enhanced care to isolated villages and families.
References
- (2014) Lancet Glob Health. 2(6): e323-33.
- (2015) Trends in maternal mortality: 1990 to 2015. Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division, p. 98.
- (2013) United Nations Millennium Development Goals.
- Maureen EC, Marie AB, Dawit T, Daniel B, Ayele T, et al. (2017) Maternal and neonatal services in Ethiopia: Measuring and improving quality. Bull World Health Organ 95(6): 473-477.
- Darmstadt GL, Tanya M, Mariam C, Win B, Saul M, et al. (2013) A strategy for reducing maternal and newborn deaths by 2015 and beyond. BMC Pregnancy and Childbirth 13: 216.
- Darmstadt GL, Zulfiqar AB, Simon C, Taghreed A, Neff W, et al. (2005) Evidence-based, cost-effective interventions: How many newborn babies can we save? Lancet 365(9463): 977-988.
- Bryce J, Bernadette D, Archana D, Vincent F, Joy EL, et al. (2008) Countdown to 2015 for maternal, newborn, and child survival: The 2008 report on tracking coverage of interventions. Lancet 371(9620): 1247-1258.
- (2017) FMOH (Federal Ministry of Health).
- Ethiopia Health Extension Program. Institutional Arrangements for HSDP IV.
- Tedbabe D, Yared A, Brian M (2014) Local understandings of care during delivery and postnatal period to inform home based package of newborn care interventions in rural Ethiopia: A qualitative study. BMC International Health and Human Rights 14: 17.
- Memirie ST, Stéphane V, Ole FN, Carol L, Kjell AJ (2016) Inequalities in utilization of maternal and child health services in Ethiopia: The role of primary health care. BMC Health Services Research 16: 51.
- World Health Organization (2010) The world health report. Health systems financing: The path to universal coverage. Geneva: World health organization.
- (2006) Central statistical agency [Ethiopia] and ICF international. Ethiopia demographic health survey 2005. Addis Ababa and Calverton, Maryland: Central Statistical Agency and ICF International.
- Roro FE, Mitike MS, Lynn MS (2018) Determinants of perinatal mortality among cohorts of pregnant women in three districts of North Showa zone, Oromia Region, Ethiopia: Community based nested case control study. BMC Public Health 18: 888.
- (2014) Central Statistical Agency [Ethiopia]. Ethiopia Mini Demographic and Health Survey. Addis Ababa, Ethiopia.
- Asheber G (2000) Perinatal mortality audit at Jimma Hospital, South-Western Ethiopia 1990-1999. Ethiopian Journal of Health Development. 14(3): 335-343.
- (2012) Central Statistical Agency [Ethiopia] and ICF international. Ethiopia demographic and health survey. Addis Ababa, Ethiopia, and Calverton, Maryl and USA: Central Statistical Agency and ICF International.
© 2023 Iñaki Alegria. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






