- Submissions

Full Text
Research in Pediatrics & Neonatology
Bacteremia and Skin Manifestations by Bacillus Cereus in a Pediatric Patient with Febrile Neutropenia
Marcela Hincapié Echeverría1, Kevin Rico Gutiérrez2 María Alejandra Suárez3 and Carolina Bonilla González4*
1,2Pediatrics resident, School of Medicine, Universidad delos Andes, Bogotá, Colombia
3Pediatric Infectious Disease Specialist, Pediatric Service, Fundación Santa Fe de Bogotá. Bogotá, Colombia
4Pediatric Intensivist, Pediatric Service, Pediatric Intensive Care and Burn Unit, Fundación Santa Fe de Bogotá. Bogotá, Colombia
*Corresponding author: Carolina Bonilla González, Pediatric Intensivist, Pediatric Service, Pediatric Intensive Care and Burn Unit, Fundación Santa Fe de Bogotá. Bogotá, Colombia
Submission: March 01, 2023; Published: March 13, 2023

ISSN: 2577-9200 Volume7 Issue3
Abstract
Bacillus cereus is a gram-positive bacteria known for causing food poisoning, but it can also cause severe infections in immunosuppressed patients. We present a case of a 12-year-old patient with acute lymphoblastic leukemia who developed severe febrile neutropenia and bacteremia by B. cereus, with skin lesions on the lower limbs. The patient received directed antibiotic treatment with an adequate response. Infection by B. cereus in immunosuppressed patients is unusual, and risk factors include corticosteroid use, intrathecal chemotherapy, central venous catheter, and neutropenia. Mortality in these patients is high. It is important to consider the risk of bacteremia in soft tissue infections and the need for an interdisciplinary team for the management of these patients.
Keywords:Pediatrics; Immunodeficiency; Bacteremia; Microorganism; Pathogen; Patient case
Introduction
Bacillus cereus (B. cereus) is a gram-positive, facultative anaerobic, flagellated, sporeforming bacterium that produces toxins and adheres easily to epithelial cells by creating biofilms. Due to its characteristics, it is resistant to high temperatures, dehydration, freezing and radiation. The most recognized clinical manifestations of B. cereus are intestinal, as a consequence of food poisoning. However, they should be recognized, especially in immunosuppressed patients, in whom respiratory infections, endophthalmitis, meningitis, osteoarticular infection, hepatitis, gangrene-like infections, endocarditis, among others, are described. We present the clinical case of a 12-year-old male patient with acute lymphoblastic leukemia (ALL) of B-precursors, who presented severe febrile neutropenia secondary to B. cereus bacteremia, associated with skin lesions on the lower limbs and a positive skin biopsy culture for B. cereus.
Clinical Case Description
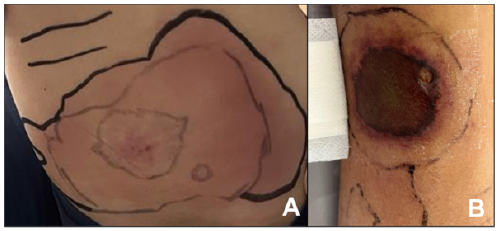
A 12-year-old male patient, with no relevant medical history, presented to the emergency department with a 20-day clinical picture of fever spikes predominately at night, diaphoresis, nausea, vomiting, and asthenia. Cytopenia was documented in the initial blood count, and after completing the necessary studies, a diagnosis of B-cell precursor acute lymphoblastic leukemia (ALL) was confirmed. Subsequently, he started chemotherapy induction according to the BFM ALLIC 09 protocol and prophylaxis with trimethoprim-sulfamethoxazole (TMP/SMX). During his hospital stay, he developed severe febrile neutropenia and disseminated intravascular coagulation. This was associated with purpuric lesions on the lower extremities, mainly in the left perialveolar region and the posterior aspect of the lower third of the left thigh. The lesions were erythematous-violaceous macules with poorly defined, irregular edges, without net-like patterns, with paler areas and some erosions on a rounded, central erythematous-edematous< base, painful to the touch, and with progressive extension (Figure 1A). The patient had no history of recent wounds or trauma at that level. Treatment was initiated according to the institutional protocol for febrile neutropenia with vancomycin and cefepime. Positive blood cultures for B. cereus were obtained. The patient continued the mentioned antimicrobial treatment. However, with progression and an increase in the number of lesions on the lower extremities, with limited mobility of the femoropatellar joint and the foot, the previously described purpuric lesion progressed to a well-defined, regular, and net-like rounded violet plate with a necrotic border and an adjacent erythematous-violaceous halo (Figure 1B), along with increasing acute-phase reactants. Necrotizing fasciitis risk was considered, and ciprofloxacin was added. If there was clinical or paraclinical deterioration, escalation to carbapenem therapy was planned.
Figure 1: A : Progressive extension, B: Net-like rounded violet plate with a necrotic border and an adjacent erythematous-violaceous halo.
A skin biopsy was performed due to suspected septic embolism, with a report of scant superficial perivascular lymphoid infiltration associated with frequent hemosiderin phages and some extravasated erythrocytes. Pathology showed no evidence of hematolymphoid neoplasia involvement. The histopathological diagnosis was pigmented purpuric dermatosis, a finding considered non-specific, possibly due to infection, which was corroborated by positive skin culture for B. cereus. Further studies were conducted for pyomyositis with magnetic resonance imaging of the lower extremities, which showed signs of diffuse bilateral and symmetrical myopathy activity, with extensive laminar perifascial fluid adjacent to the muscles of the anterior extensor compartment of the thigh in its anterolateral aspect, in addition to diffuse subcutaneous edema with slight associated septal enhancement. Control blood cultures were taken on the fourth day of treatment with Vancomycin and Cefepime and on the second day with Ciprofloxacin, with negative results. Therefore, Cefepime was suspended, and treatment continued with Vancomycin for a total of 14 days and Ciprofloxacin, to be determined based on the patient’s evolution.
There was an improvement in the skin lesions, which were in the resolution phase, with improvement in pain and femoropatellar joint limitation, modulation of the systemic inflammatory response, and resolved shock. The patient was transferred to inpatient care to continue antibiotic treatment. However, on the seventh and ninth day of treatment with Ciprofloxacin and Vancomycin, respectively, he presented new inflammatory changes in the neck.
Discussion
B. cereus infection in immunosuppressed patients is uncommon, especially in pediatric cancer patients, and this is the 47th reported case in the literature. A similar case in a pediatric patient was recently reported in our region [1]. B. cereus infection is of great importance in immunosuppressed patients, with mortality rates as high as 52% and it should be included in the differential diagnosis [2]. Risk factors for this condition include high-dose systemic corticosteroid use, recent intrathecal chemotherapy, central venous catheter placement, and neutropenia [2]. Our patient had all of these risk factors. Gastrointestinal manifestations are still the most common in immunosuppressed patients, and our patient had nausea, but there was improvement after changing from oral to systemic corticosteroid administration, without presenting any other gastrointestinal symptoms [2]. Extraintestinal involvement has been described in different reports [1,3]. Regarding soft tissue involvement, it is rare, although it has been described as a primary skin infection in immunocompromised and immunocompetent patients, usually associated with traumatic lesions, with cellulitis being the most common clinical manifestation [4].
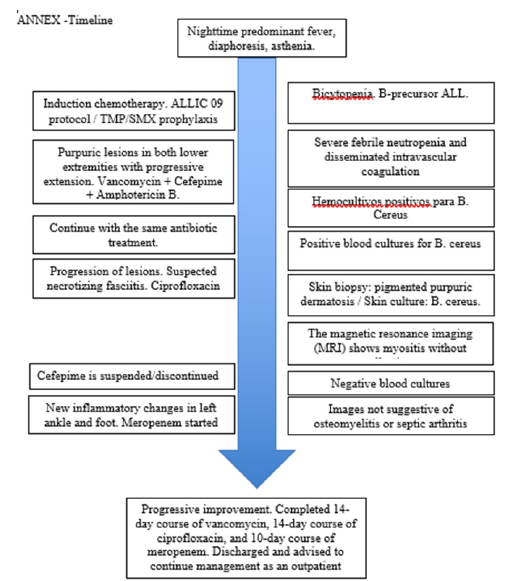
According to a study at St. Jude Children’s Hospital, 10 cases of primary skin infection by B. cereus in children with cancer and neutropenia were reported over a period of five years. The primary lesion was papules or vesicles, with subsequent appearance of a black scar in the center of the lesion and rapid progression to cellulitis, similar to infection by B. anthrax [4,5]. Regarding treatment, B. cereus produces three different beta-lactamases, three types of phospholipase C and a matrix metalloproteinase, making it a microorganism with antimicrobial resistance to penicillin’s, cephalosporins and trimethoprim-sulfamethoxazole (TMP/SMX), but sensitive to aminoglycosides, carbapenems, vancomycin and fluoroquinolones [6,2]. In a study of B. cereus bloodstream infections, no vancomycin-resistant strains were found, although quinolone resistance was found in about 10% [7]. Our patient had an adequate response to vancomycin and ciprofloxacin, but with the reappearance of local inflammation signs in the lower extremity, carbapenem was added due to suspected gram-negative bacteria infection, which was not confirmed, with an adequate response and clinical resolution of symptoms. This case is similar to those reported with respect to risk factors; however, skin manifestations have been poorly described. Our case is relevant for healthcare professionals responsible for monitoring and treating immunosuppressed patients, as it emphasizes the need to consider the risk of bacteremia in soft tissue infections and the importance of an interdisciplinary team for managing these patients (Annex).
Figure 2: Timeline
References
- Calderón GA, Buitrago EJ, Luengas MM, Godoy CJ (2020) Bacillus cereus bacteremia and brain lesions in an adolescent with acute lymphoid leukemia. Colombian Journal of Hematology and Oncology 7(2): 48-51.
- Arora S, Thakkar D, Upasana K, Yadav A, Rastogi N, et al. (2021) Bacillus cereus infection in pediatric oncology patients: A case report and review of literature. ID Cases 26: e01302.
- Koop L, Garg R, Nguyen T, Gujjula NR, Velagapudi M (2021) Bacillus cereus: Beyond gastroenteritis. WMJ 120(2): 145-147.
- Bottone EJ (2010) Bacillus cereus, a volatile human pathogen. Clinical Microbiology Reviews 23(2): 382-398.
- Henrickson KJ, Flynn PM, Shenep JL, Pui CH (1989) Primary cutaneous bacillus cereus infection in neutropenic children. Lancet 1(8638): 601-603.
- Enosi TD, Mathur A, Ngo C, Man SM (2021) Bacillus cereus: Epidemiology, virulence factors, and host-pathogen interactions. Trends Microbiology 29(5): 458-471.
- Ikeda M, Yagihara Y, Tatsuno K, Okazaki M, Okugawa S, et al. (2015) Clinical characteristics and antimicrobial susceptibility of Bacillus cereus blood stream infections. Ann Clin Microbiol Antimicrob 14: 43.
© 2023 Carolina Bonilla González. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






