- Submissions

Full Text
Research in Pediatrics & Neonatology
Extracranial Pseudoaneurysm of the Internal Carotid Artery in a Young Child
Fedir Yurochko1, Dzvenyslava Kopanska1*, Roman Trutyak2, Dmytro Beshley2,3,4, Bohdan Malovany1, Daryna Klakovych1 and Wojciech Domka5,6
1Lviv Regional Pediatric Hospital OKHMATDYT, Ukraine
2Danylo Halytsky Lviv National Medical University, Ukraine
3Ukrainian-Polish Heart Center “Lviv”, Ukraine
4Lviv Regional Clinical Hospital, Ukraine
5University of Rzeszow, Faculty of Medicine, Poland
6Clinical Department of Otorhinolarygology, Frederic Chopin Clinical Voivodeship Hospital, Poland
*Corresponding author: Dzvenyslava Kopanska, Lviv Regional Pediatric Hospital OKHMATDYT, Ukraine
Submission: June 24, 2022; Published: July 26, 2022

ISSN: 2577-9200 Volume6 Issue4
Introduction
Extracranial pseudoaneurysms of the Internal Carotid Artery (ICA) in small children are extremely rare, only a few such cases have been described. Pseudoaneurysm-is a blood-filled cavity, that comes into contact with an artery and has a stable connection with its lumen [1,2]. Pseudoaneurysm occurs due to the damage of the artery wall, wall of the pseudoaneurysm is formed by hematoma and connective tissue [1]. There is a high mortality rate due to thromboembolic complications or massive bleeding [1,3,4]. If this condition isn’t treated properly, the mortality rate can reach up to 77% [5]. Because of this fact, general practitioners should be aware of this rare pathology in order to accurately diagnose and treat it, and eventually save a child’s life [3,4].
In this article, we present a case report of a 1-year-7-month-old boy with an extracranial pseudoaneurysm of ICA, which initially manifested as parapharyngeal abscess, sepsis, and respiratory distress. The final treatment plan consisted of endoprosthesis of ICA with the exclusion of pseudoaneurysm from the bloodstream.
Case Report
1-year-7-month-old boy J. was admitted to the Intensive Care Unit of the Lviv Regional Pediatric Hospital OKHMATDYT in severe condition with a previous diagnosis of “Parapharyngeal abscess. Aspiration pneumonia. Sepsis”. It is known that he was ill for 3 weeks, the disease began with fever, signs of acute respiratory infection, pharyngitis. He received oral cefpodoxime. After the previous improvement of his general condition there was a gradual deterioration, due to which the child was admitted to the hospital with a diagnosis of “Parapharyngeal abscess”. In the ENT department of the pediatric hospital of another region, an abscess was punctured and opened, blood was obtained; after that the abscess then began to grow, airway stenosis began, the child was intubated and transferred to the Intensive Care Unit of that hospital, and then to the intensive care unit of Lviv Regional Pediatric Hospital OKHMATDYT.
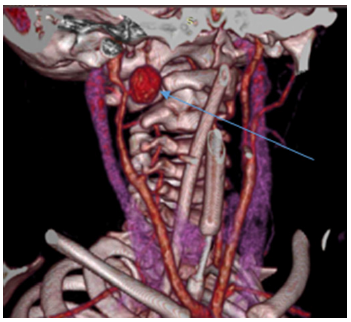
At the admission, the child’s condition was severe, with signs of sepsis. At oropharyngoscopy: large dense elastic non-pulsating protrusion in the parapharyngeal space on the right side, approximately 5x5cm in size, with a shift to the midline of the pharynx. Ultrasound examination of the neck showed an abscess cavity. On MRI of the neck-there is a large abscess and hematoma in the parapharyngeal space (Figure 1). The decision was made to perform an urgent surgery. The parapharyngeal space was opened and drained, there were many blood clots and a small amount of pus in the lumen of it. During the surgical intervention, moderate bleeding developed, which was stopped by tamponade. Hemostatic tampons were removed after 4 days, there were no signs of recurrent bleeding. A few days later a massive bleeding from the pharynx occurred, which led to clinical death of the child. Immediate resuscitation measures were performed, the bleeding was temporarily stopped by finger stamping and the patient’s vital signs were stabilized. Vascular surgeons were called, and the pharyngeal bleeding stopped during the operation after squeezing of the external carotid artery, so the external carotid artery was ligated. In the early postoperative period, a CT scan in a vascular mode was performed, where an extracranial aneurysm of the right ICA was detected (Figure 2).
Figure 1: Coronal MRI of our patient’s head in T1-weighted scan shows large parapharyngeal abscess and hematoma.
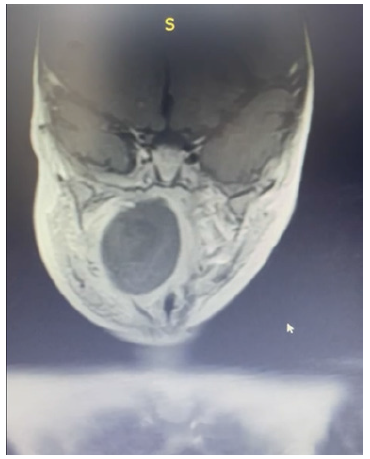
Figure 2: CT scan in a vascular mode; we can see a pseudoaneurysm of the right ICA (arrow).
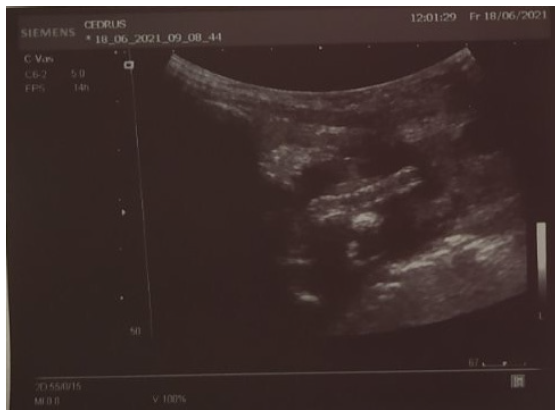
The child was transferred to the specialized center of vascular and cardiac surgery at the Lviv Regional Clinical Hospital, where he underwent endoprosthesis of the right internal carotid artery with the exception of the detected pseudoaneurysm from the bloodstream. Abbott Graft master 4x26mm balloon was used to open the endoprosthesis (Figure 3). After the surgery child was transferred back to Lviv RPH OKHMATDYT. No complications were seen during postoperative period. The child was discharged due to improvement of his condition. The patient was prescribed clopidogrel to prevent endograft thrombosis. Conclusion of ultrasound examinations of neck vessels (Figure 4) within 1 year: condition is stable, the stent is passable. The patient is still being supervised by vascular surgeons.
Figure 3: Arteriogram showing pseudoaneurysm of the right ICA.
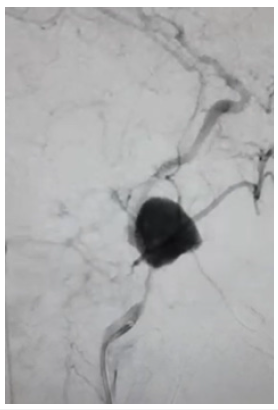
Figure 4: Ultrasound scan of the neck vessels 2 months after endoprosthesis, stent is visualized.
Discussion
Aneurysms of ICA are divided by histopathological characteristics into true and false (pseudoaneurysms). The wall of a true aneurysm consists of all three layers of the artery wall, the wall of the pseudoaneurysm does not have all of them. Causes of extracranial pseudoaneurysm of the Internal Carotid Artery (ICA) include previous ICA surgery, ICA trauma, infection, spontaneous ICA dissection, systemic connective tissue disease, radiation therapy [1,2,6]. The most common infectious causes of ICA pseudoaneurysms in children are meningitis, cervical lymphadenitis and ear infections [2]. Cases of pseudoaneurysms due to deep neck infections and parapharyngeal/peritonsillar abscesses have also been reported. The main cause of vascular spread of the pharyngeal and deep neck infections is the close proximity of ICA to these structures [1,4]. In our case, the pseudoaneurysm occurred due to the direct spread of infection from the deep spaces of the neck to the wall of ICA.
Extracranial pseudoaneurysm of ICA, which is caused by bacterial factors, is most often associated with S. aureus, Salmonella, Streptococcus pyogenes, Escherichia coli and Klebsiella [1,2]. The incidence of carotid artery aneurysms is increased in HIV-positive patients and occurs due to HIV-associated vasopathy [7]. Congenital causes of aneurysms due to structural defects of the arterial wall (vascular malformations), namely defects in the development of the arterial muscular layer, have also been described in children [4].
Symptoms of extracranial pseudoaneurysm of ICA can range from minimal to large with life-threatening manifestations (airway stenosis, massive bleeding). Symptoms manifest from local exposure, embolism, or rupture of a pseudoaneurysm [2]. Extracranial pseudoaneurysm can manifest in fever and swelling of the neck, disguised as inflammatory diseases [8,9]. If the pseudoaneurysm increases in size, it can push adjacent structures, causing swallowing disorders and shortness of breath [10]. Pressure on the surrounding nerves can cause Horner’s syndrome, hoarseness, dysphagia, earache, and weakness of the tongue muscles. In a pseudoaneurysm, a blood clot may form [1-3]. It can then migrate to the intracranial arteries, blocking them and causing a stroke [11]. If a pseudoaneurysm breaks into neighboring structures, bleeding from the nose, pharynx, ear, or gastrointestinal tract may occur [12,13]. Rupture of the pseudoaneurysm is a potentially life-threatening complication that can occur in one out of three children [1,2,4].
The final diagnosis is established on the basis of imaging studies. Given the availability and cheapness of ultrasound examination, it is the first step in additional diagnostics. The “gold” standard for artery imaging is traditional angiography [14]. Vascular CT and magnetic resonance angiography are useful refinement imaging studies that can determine the extent and presence of an aneurysm thrombus, as well as demonstrate the relationship of the aneurysm to surrounding structures [2]. In our case, we performed ultrasound examination and MRI, which did not reveal any pseudoaneurysms. Then massive bleeding occurred, after which CT scan with vascular mode was performed, where the final diagnosis was made.
Open access surgeries have recently been replaced by endovascular techniques, which are safer and more accessible [3,6]. Open access surgery carries risks of higher morbidity and mortality, as well as a higher risk of cranial nerves injury [6]. However, it is still recommended to use open techniques in children (because stent grafts do not grow, while children do) because of the much better long-term results. Open surgery should also be preferred over endovascular access when carotid artery is involved. Despite this fact, we chose endovascular treatment in this patient. The reason of that was: the location of the pseudoaneurysm (that occurred just before the entrance of the skull), as well as the fact that our patient had a previous surgery (and scar tissue).
Open access surgery includes ligation of the carotid artery, excision of the aneurysm with reconstruction using a subcutaneous vein graft or prosthetic material [2,4]. In children younger than four years, a large subcutaneous vein graft may be too small for supraoptic interposition with a theoretical risk of stenosis [4]. In these cases, the use of a superficial femoral vein graft for interposition is described [4]. Open surgery is especially difficult in children due to the delicate anatomy of their vessels [4].
Endovascular surgeries include stent placement stenting, trans-stent spiral embolization, stent-graft aneurysm exclusion, or carotid endovascular occlusion [2]. In children, certain worries are caused by the adaptation of the growing carotid artery to the existing stent [3]. Our patient is under constant supervision; if in the process of his growth and development, a mismatch of the size of the ICA to the size of the endograft occurs, we will endovasculary open (open more) endograft up to a diameter of 6mm. In our case, endovascular prosthesis of ICA was performed, which ensured the exclusion of pseudoaneurysm from the bloodstream. Given the concomitant retropharyngeal abscess affecting the ICA, there was some concern about stent graft infection, but no signs of infection were detected during the one-year follow-up.
Conclusion
Although extracranial pseudoaneurysms of ICA are extremely rare in children, they pose a high risk to the child’s life in the absence of adequate treatment. This disease should always be considered as differential diagnosis of neck and parapharyngeal abscesses, especially in young children. Ultrasound examination, CT and MRI in a vascular mode should be used as additional diagnostic techniques, with doctors’ preoccupation with pseudoaneurysms. Endovascular intervention is the safest type of treatment of this condition for children.
References
- Requejo F, Sierre S, Lipsich J, Zuccaro G (2013) Endovascular treatment of post-pharyngitis internal carotid artery pseudoaneurysm with a covered stent in a child: A case report. Childs Nerv Syst 29(8): 1369-1373.
- Krikwood ML (2015) Extracranial carotid artery aneurysm, UpToDate.
- Garcia-Monaco RD, Kohan AA, Martinez-Corvalan MP, Cacchiarelli N, Peralta O, et al. (2012) Thrombin injection failure with subsequent successful stent-graft placement for the treatment of an extracranial internal carotid pseudoaneurysm in a 5-year-old child. Cardiovasc Intervent Radiol 35(3): 704-708.
- Pourhassan S, Grotemeyer D, Fokou M, Heinen W, Balzer K, et al. (2007) Extracranial carotid arteries aneurysms in children: single-center experiences in 4 patients and review of the literature. J Pediatr Surg 42(11): 1961-1968.
- Salinger S, Pearlman S (1933) Hemorrhage from pharyngeal and peritonsillar abscesses: Report of cases, resume of the literature and discussion of ligation of the carotid artery. Arch Otolaryngol 18(4): 464-509.
- Pulli R, Dorigo W, Pratesi G, Fargion A, Pratesi C (2013) Single-center experience on endovascular repair of noninfected extracranial internal carotid artery pseudoaneurysms. Ann Vasc Surg 27(5): e13-e17.
- Padayachy V, Robbs JV (2012) Carotid artery aneurysms in patients with human immunodeficiency virus. J Vasc Surg 55(2): 331-337
- Lee NN, Long G, Ngai S, Sahrir S, Parker A, et al. (2004) Right internal carotid pseudoaneurysm mimicking a retropharyngeal abscess in a child. Med J Malaysia 59(5): 685-687.
- Gupta R, Patro SK, Chauhan N, Kumar A (2019) A giant pseudoaneurysm mimicking retropharyngeal abscess in a child. Pediatr Emerg Care 35(5): e79-83.
- Tannuri U, Mendes de Almeida N, Piske R, Matsumoto T (2003) Giant pseudoaneurysm of the internal carotid artery causing upper airway obstruction in a 10-month-old infant treated by endovascular occlusion and surgical drainage. J Pediatr Surg 38(9): 1393-1395.
- Ruff MW, Nasr DM, Klaas JP, Renaud DL (2017) Internal carotid artery pseudoaneurysm and ischemic stroke secondary to retropharyngeal and parapharyngeal abscess. J Child Neurol 32(2): 230-236.
- da Silva PS, Waisberg DR (2011) Internal carotid artery pseudoaneurysm with life-threatening epistaxis as a complication of deep neck space infection. Pediatr Emerg Care 27(5): 422-424.
- Gralla J, Brekenfeld C, Schmidli J, Caversaccio M, Do DD, et al. (2004) Internal carotid artery aneurysm with life-threatening hemorrhages in a pediatric patient: Endovascular treatment options. J Endovasc Ther 11(6): 734-7348.
- Almolani F, Almomen A, Alhamam J, Alsheef H, Aldhurais A, et al. (2021) Internal carotid artery pseudoaneurysm presenting with bloody otorrhea and Horner’s syndrome in a child. Am J Otolaryngol Head Neck Surg 4(4): 1133.
© 2022 Dzvenyslava Kopanska. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






